Table of Contents
Double aortic dissection in a patient with Marfan disease. A case report
Published on: 27th December, 2022
Marfan syndrome is a dominant autosomal genetic disease of the connective tissue, leading to various complications. Cardiovascular complications are the main ones, with dilation of the aorta and aortic dissection which is the main cause of death. Double dissection with different sites of departure is scarcely reported by the literature. We reported the case of a 22-year’s-old young patient admitted for acute chest and abdominal pains, and cardiogenic shock. Investigations reported a double dissection of the aorta with a recent one of type A and an old one of type B. Ghent diagnostic criteria were used to allow the diagnosis of Marfan disease. Surgical management corrected successfully the type A dissection.Early diagnostic and adequate management of aortic complications can reduce the high mortality rate of patients with Marfan syndrome.
Correlation between chronic inflammation of rheumatoid arthritis and coronary lesions: “About a monocentric series of 202 cases”
Published on: 6th December, 2022
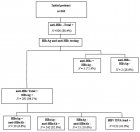
Introduction: Cardiovascular diseases are the leading cause of death in the world, headed by coronary artery disease, which is secondary to atherosclerosis. The latter recognizes classic risk factors such as diabetes, high blood pressure, tobacco, and dyslipidemia and other less classic factors such as chronic inflammation of rheumatoid arthritis. Many studies have highlighted the correlation between this chronic inflammation and clinical coronary disease but very few have focused on the anatomical correlation. Objective: To describe the correlation between the chronic biological inflammation of rheumatoid arthritis and anatomical coronary lesions on angiography. Method: This observational, retrospective, single-center study, including over 10 years, of patients with rheumatoid arthritis, confirmed the EULAR 2010 criteria and presented with coronary artery disease requiring coronary angiography. Patients with missing data or in whom coronary angiography was not done were excluded (n = 14). We divided then the patients according to the existence or not of chronic inflammation to study the impact of the latter on the existence (Stenosis < 50% vs. stenosis ≥ 50%), the extent (single vs. multivessel disease), and the severity of the coronary lesions (syntax score < 32 vs. ≥ 32). Results: 202 patients (49♂/153♀) aged between 30-75 years with a history of rheumatoid arthritis have had a coronary event requiring coronary angiography, were included; The mean ejection fraction at baseline was 57.3% +/- 5.8 (37 vs.-65%). 75% of them were ≥ 65 years old. 55% were diabetics, 61% with hypertension, 38% with dyslipidemia, and 19% were smokers. Chronic inflammation was diagnosed in 70% of them on non-specific parameters (ESR, CRP, fibrinogen, anemia, and rheumatoid factor). All patients had coronary angiography, which made it possible to identify the coronary lesions according to their existence (Stenosis < 50%: 51 patients vs. stenosis ≥ 50%: 151 patients), the extent (single: 86 patients vs. multivessel disease: 116 patients) and the severity of the coronary lesions (syntax score < 32: 142 patients vs. ≥ 32: 60 patients). Chronic inflammation of rheumatoid arthritis was correlated in bivariate and multivariate analysis (after excluding the impact of other risk factors) with the existence and extent of coronary lesions (p < 0.05) but not with their severity (p > 0.05). Discussion: The two limitations of this work are the monocentric nature of the study and the absence of specific inflammatory parameters such as anti-CCP antibodies. Strengths are anatomical correlations and multivariate analysis. Chronic inflammation apart from any influence of the various risk factors predisposes to the existence and extent of coronary lesions (p < 0.05). The severity of coronary lesions assessed by Syntax Score was not correlated with chronic inflammation, although other studies suggest that this inflammation is the cause of complex lesions.Interpretation: Rheumatoid arthritis is associated with an increase in cardiac morbidity and mortality. Atheromatous lesions are more frequent in those patients than the existence of classic cardiovascular risk factors would suggest. Several explanations could account for this risk: the inflammatory syndrome and its impact on the cardiovascular risk factors and the vessel and the deleterious effect of the treatments. This requires stricter screening and management of risk factors in rheumatoid arthritis.
Percutaneous Atrial Septal Defect (ASD) closure technique in case of association with an azygos continuation of the inferior vena cava “case report”
Published on: 2nd December, 2022
Introduction: Atrial Septal Defect (ASD) is the most common congenital heart disease, accessible to percutaneous closure in 90% of cases. The closure procedure is performed usually under local anesthesia and TTE by femoral access. The association of OS-ASD with an azygos continuation of the inferior vena cava is very rare (< 0.1/1000 births) making femoral access impossible. Only a few cases are mentioned in the literature, here we describe the procedure as faithfully as possible. Important clinical finding: We present a case of a 32-years-old female candidate for percutaneous closure of OS-ASD with right cavity dilatation who present during her procedure an unusual guidewire path suspecting an azygos continuation of the inferior vena cava, confirmed by CT angiography, making impossible the closure via the femoral approach. Therapeutic intervention: After being confronted with the categorical patient refusal of the surgery, we performed successfully the procedure; one month later; under general sedation by internal jugular approach. We finished with manual compression before extubating the patient. Outcomes: The follow-up was favorable at the cost of a hematoma at the puncture site and brachial plexus compression, which regressed after 3 days. Conclusion: We opted for general anesthesia and intubation to guide the procedure by TEE. We placed it in the aorta, which gave us good stability to continue successfully the procedure. We underestimated the risk of complication at the puncture site, which could have been avoided by using a vascular suture device or more prolonged compression. Main takeaway lesson: Percutaneous closure is the reference treatment for OS-ASD. In case of is associated with an azygos continuation of the inferior vena cava, the right internal jugular vein remains a reasonable approach; it requires discussion and rigorous preparation by the whole team. The management of the puncture site in this situation remains delicate and requires great concentration.
How to manage balloon entrapment during percutaneous coronary intervention of a calcified lesion “Case report”
Published on: 2nd December, 2022
Percutaneous coronary angioplasty is a minimally invasive procedure aimed at unclogging a coronary artery with a low complication rate (with a serious complication rate of 3% to 7% and a mortality rate of 1.2%). Device entrapment during PCI is a rare but life-threatening complication that occurs in < 1% of PCIs and balloon entrapment comes second after coronary guidewires. We present the case of 68-years-old man, smoker, hypertensive and type2 diabetic that presents angina with evidence of ischemia on myocardial tomoscintigraphy and in whom the radial coronary angiography reveals a tight calcified mid LAD stenosis. During his PCI and after dilatation with an NC balloon 2.5 × 12 the latter refuses to deflate and remains trapped in the lesion with the appearance of pain and ST-elevation despite several attempts to dilute the product in the inflator and to burst it by overexpansion. Traction on the balloon resulted in the deep intubation of the guiding-catheter, which comes in contact with the trapped balloon, and the rupture of the latter’s hypotube, which remains inflated at the site of the lesion and mounted on the 0.014 guidewire. We put a second 0.014 guidewire distally in the LAD and twisted with the distal part of the first guidewire, then we introduced a second balloon 2.0 × 20 over the second guidewire until the distal part of the guiding-catheter and inflated to trap the stucked balloon. We gradually removed this emergency assembly that allowed us to retrieve the trapped balloon. The control injection revealed a thrombotic occlusion of the LAD treated by thrombectomy and anti-GPIIbIIIa followed by a DES 2.75 × 28 placement. The patient was discharged 48 hours later with a good LVEF. The possible balloon entrapment mechanisms are an acute recoil of a highly calcified lesion with compression of the incompletely deflated balloon, which seems to be the case in our patient, strangulation of the proximal balloon end by the guiding-catheter if the balloon is removed before complete deflation and break or bend of the hypotube. The solutions in case of undeflatable balloon entrapment are to dilute the product in the inflator, to burst it by overexpansion, to pierce it through a stiff guidewire (or through its other end on a Microcatheter or OTW balloon), to cut its outer part and let it empty passively, to introduce a second guide-wire and perform a Buddy-Balloon or to transfer the patient to Surgery. Material entrapment remains a rare but life-threatening complication, its eviction requires the choice of material size and gentle manipulations (small balloons in the event of a calcified lesion) and its management uses different techniques, the choice of which depends on the clinical and anatomical situation.
Oncocardiology: Far beyond the cardiotoxicity
Published on: 29th November, 2022
Approximately 73.4% of global deaths are caused by chronic non-communicable diseases, among them, cardiovascular and cerebrovascular diseases, tumors, and chronic respiratory diseases ranked in the top 3 respectively [1]. An accumulating body of evidence showed that the risk of all-cause mortality in cancer patients with cardiovascular disease (CVD) was 3.78 times higher than that of those without CVD and 8.8% of cancer survivors died of CVD [2]. Heart failure (HF) is a serious manifestation or terminal stage of various heart diseases. Although myocardial damage and dysfunction are the main causes of HF, the cardiovascular injury caused by the tumor itself and the detrimental effect of cancer treatment also play an important role. More recently, the data has suggested that up to 25% - 30% of patients with HF have histories of cancer for about 10 years; and cancer also determines the prognosis of heart HF [3].
Acute ischemic stroke for alteplase or medical care alone or intervention with/without alteplase in Palestine (AIS-AMI Palestine)
Published on: 22nd November, 2022
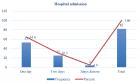
Background: Stroke is the most common cause of permanent disability and the third most common cause of death in Palestine. We aimed to examine patterns of stroke presentation, causes, management and outcomes at the largest public Mistry of health hospitals in Palestine.Methods: Comprehensive data from all patients with acute ischemic stroke who were admitted to al-Shifa hospital between November 2021 and July 2022 and treated with alteplase alone or endovascular intervention with or without alteplase were prospectively collected and compare with acute ischemic stroke patients who were treated with medical care alone at Palestine medical complex hospital at 2018. Acute ischemic stroke presentation patterns, in-hospital evaluation and management, mortality, and morbidity were evaluated. Results: Medical care alone group: 138 patients with acute ischemic stroke, mean age was 65 ± 14 years and 49% were women. Most of the patients received antiplatelet therapy (98%), although none received thrombolysis. Only 17% received physical therapy evaluation. In-hospital mortality was 13%, and a modified ranking score of 0 -2 was in 44 patients (32%). Endovascular intervention with/without alteplase group: 56 patients with acute ischemic stroke. The mean age was 61 ± 12 years and 41% were women. All patients received brain computed tomography scans, although few received other investigations such as carotid Doppler (13%). Most patients with ischemic stroke received antiplatelet therapy (99%), although 39 patients (70%) received thrombolysis. Only 61% received physical therapy evaluation. In-hospital mortality was 7%. The modified ranking score 0 - 2: 32 patients (57%).Conclusion: This study conducted in Palestine showed that among patients with acute ischemic stroke, functional outcomes according to modified ranking score 0 - 2 were better by endovascular therapy with/without alteplase than with medical care alone.
Atrial fibrillation in elite athletes. What is missing?
Published on: 27th October, 2022
Although the beneficial effect of physical activity in the general population is well established, in elite athletes under vigorous physical activity, the effect on the electrical system of the heart is controversial. Indeed, several studies have shown an increased rate of atrial fibrillation among athletes, whereas others suggest that improved exercise capacity with training reduces atrial fibrillation recurrence. The pathophysiologic explanation of that discrepancy is missing, although several underlying mechanisms have been proposed. Taking into account the current knowledge, it seems that, although the beneficial effects of exercise are well recognized, there are conflicting data regarding the relation of the occurrence - the rate of atrial fibrillation to high-volume exercise and too long-term training. Its significance on the quality of life especially in highly trained athletes remains to be elucidated. Therefore, this short review will try to discuss this discrepancy and hopefully underlie the arising arguments.
A patient with pulseless ST elevation myocardial infarction caused by a very late stent thrombosis
Published on: 24th September, 2022
Background: Persistent contrast staining is highly associated with stent thrombosis. Case summary: A 75-year-old woman presented with new-onset effort angina. A coronary angiogram revealed a 90% blockage of the distal left main trunk (LMT) and a 99% blockage of the ostial left anterior descending coronary artery (LAD). A 3.0 × 18-mm CYPHER™ the stent had previously been implanted into the dominant proximal circumflex artery (LCx) in 2009 because of unstable angina. The patient developed pulseless ST elevation myocardial infarction after the withdrawal of antiplatelet therapy before a scheduled CABG. The patient recovered with VA-ECMO and PCI using aspiration thrombectomy and urgent CABG.Discussion: This case highlighted that a preoperative patient may develop thrombosis at a previous stent site with peri-stent contrast staining and withdrawal of an antiplatelet regimen in certain settings poses an imminent risk for preoperative deterioration. A bridging strategy using intravenous PY12 inhibitor before CABG should be considered in this setting. The revascularization strategy should be selected based on coronary anatomy, hemodynamic status and baseline risk for CABG. A hybrid revascularization approach should be considered in this patient population.
Does global longitudinal strain improve stratification risk in heart failure with preserved ejection fraction?
Published on: 8th September, 2022
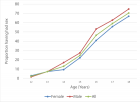
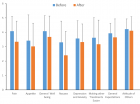
Background: Heart Failure with Preserved Ejection Fraction (HFPEF) accounts for more than half of the cases of heart failure.Long regarded as an abnormality of left ventricular diastolic function, recent studies using longitudinal strain (two-dimensional speckle tracking mode) have suggested that left ventricular longitudinal systolic function is altered in HFPEF.Despite these interesting pathophysiological perspectives, the data in the literature on the prognostic value of the alteration of longitudinal strain are controversial. Given these conflicting results, it is difficult to confirm the magnitude and prevalence of impaired LV longitudinal systolic function in patients with HFPEF and its prognostic relevance. Purposes: This work aims to study the prognostic value of Global the left ventricle’s Global Longitudinal Strain (GLS) Algerian cohort of patients with HFPEF. Patients and methods: We conducted a monocentric prospective observational study from April 2018 to April 2020, with a minimum follow-up of 1 year for each recruited patient. We included patients over the age of 18 referred to the echocardiography laboratory for chronic or acute HFpEF, defined according to the criteria of ESC 2016. 153 consecutive patients underwent clinical examination, biological tests, and echocardiography with measurement of GLS at rest, in addition to routine management by the attending physicians.Results: 153 patients were collected. The average age of our patients is 73 +/- 11 years ranging from 42 to 91 years old. The female population is predominant with a rate of 67%. Comorbidities are predominant mainly by arterial hypertension (86%) and diabetes (64%), with a history of atrial fibrillation (46%).63% of patients have impaired GLS (< 16%). Contrary to our hypothesis, GLS was not shown to be a powerful predictor of cardiovascular events in HFPEF patients either in dichotomous analysis (OR = 0.79; p = 0.64) or in continuous analysis (OR = 0.97; p = 0.69).We were able to identify that congestive venous signs, anemia, and pulmonary hypertension, are the main independent prognostic factors in our Algerian population study. Conclusion: We were unable to demonstrate the prognostic role of mpaired GLS in our population of patients with HFPEF.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."