About Mayo Clinic
Mayo Clinic
Articles by Mayo Clinic
His bundle pacing in heart failure: A review of current literature
Published on: 3rd March, 2020
OCLC Number/Unique Identifier: 8560715663
Biventricular (BiV) pacing revolutionized the heart failure management in patients with sinus rhythm and left bundle branch block; however, left ventricular-lead placement is not always technically possible. Also, BiV pacing does not fully normalize ventricular activation and, therefore, the ventricular resynchronization is imperfect. On the other hand, right ventricular pacing for bradycardia may cause or worsen heart failure in some patients by causing dyssynchronous ventricular activation. His bundle pacing comes as an alternative to current approaches as it activates the ventricles via the native His-Purkinje system, resulting in true physiological pacing, and, therefore, is a promising site for pacing in bradycardia and traditional CRT indications in cases where it can overcome left bundle branch block. Furthermore, it has the potential to open up new indications for pacing therapy in heart failure, such as targeting patients with PR prolongation, but a narrow QRS duration. In this article we explore the history, clinical evidence, proposed mechanisms, procedural characteristics, and the role in current therapy of His bundle pacing in the prevention and treatment of heart failure.
Inter-Observer Variability of a Commercial Patient Positioning and Verification System in Proton Therapy
Published on: 6th February, 2017
OCLC Number/Unique Identifier: 7286354964
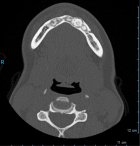
Purpose:Accurate patient positioning is crucial in radiation therapy. To fully benefit from the preciseness of proton therapy, image guided patient positioning and verification system is typically utilized in proton therapy. The purpose of this study is to evaluate the inter-observer variability of image alignment using a commercially available patient positioning and verification system in proton therapy.
Methods:The VeriSuite patient positioning and verification system (MedCom GmbH, Darmstadt, Germany) provides a six degrees of freedom correction vector by registering two orthogonal x-ray images to digitally reconstructed radiograph (DRR) images that are rendered in real time from the planning computed tomography (CT) images. Six cases of various disease sites, including brain, head & neck, lung, prostate, pelvis, and bladder, were used in this study. For each case, the planning CT images and a daily orthogonal x-ray portal image pair were loaded into the VeriSuite system. The same set of x-ray images and CT images for each case were reviewed and aligned separately by each of the 10 radiation therapist, following the clinical procedure for the corresponding disease site. The resulting correction vectors were then recorded and analyzed.
Results:Our study shows that the inter-observer variation (One standard deviation) in image alignment using the VeriSuite system ranged from 1.2 to 2.0 mm for translational correction and from 0.6 to 1.3 degrees for rotational correction for the six cases. The use of fiducial markers for prostate patient alignment achieved the least inter-observer variation while the bladder case produced the largest.
Conclusions:Inter-observer variation in image alignment could be relatively large, depending on the complexity of patient anatomy, image alignment approach, and user experience and software limitations. Automatic registration and fiducial markers could potentially be used to align patient more accurately and consistently. To ensure adequate tumor coverage in proton therapy, inter-observer variability in patient alignment should be carefully evaluated and accounted for in patient setup uncertainty analysis and treatment planning margin determination.
Preliminary Report on the Effect of Mesenchymal Stem Cell Therapy in Patients with Chronic Lung Allograft Dysfunction
Published on: 28th August, 2018
OCLC Number/Unique Identifier: 7844548189
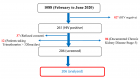
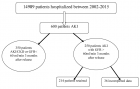
Background: Mesenchymal stem cell (MSC) effects can shift immune responses toward anti-inflammatory and tolerogenic phenotypes, potentially helping patients with bronchiolitis obliterans syndrome (BOS).
Methods: We evaluated the effect of infusing allogeneic MSC intravenously in 9 patients with moderate BOS refractory to standard therapy who were not candidates for retransplant, dividing them into 3 dosing groups: Group 1, 1×106 MSC/kg (n=3); Group 2, 2×106 MSC/kg (n=3); and Group 3, 4×106 MSC/kg (n=3). We recorded pulmonary function tests, laboratory variables, and serum biomarkers pre- and post-MSC infusion.
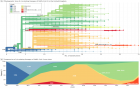
Results: These patients had significant decline in forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) over 1 year pre-MSC infusion (mean ± SD) FVC, 3.11±0.98 L, and FEV1 1.99+0.64 L versus FVC 2.58±1.03 and FEV1 1.61±0.52 just before infusion (P<0.05); representing a mean loss of 530 mL in FVC and 374 mL in FEV1 over 12 months. One year post-MSC infusion, mean FVC and FEV1 increased to 2.66±1.01 L and 1.63±0.55 L, respectively (changes no longer significant compared to before MSC infusion). Patients in Group 1 showed elevation of tolerance-inducing T regulatory cells and increased levels of epidermal growth factor. Tolerance-inducing Th-2 cytokines increased in Groups 1 and 2. These changes were not significantly different in these small sub-groups.
Conclusion: MSC infusion appears to slow down or reverse the progressive decline in lung function in some patients with moderate BOS, possibly by inducing anti-inflammatory effects and promoting cell proliferation and angiogenesis.
Long-term clinical outcome of minimally invasive versus open single-level transforaminal lumbar interbody fusion for degenerative lumbar diseases with a minimum follow-up of 2 years: A meta-analysis protocol
Published on: 18th July, 2019
Introduction: Minimally invasive surgical transforaminal lumbar interbody fusion (MIS-TLIF) is a relatively new approach for fusion of the lumbar spine. It was developed in addition to traditional open transforaminal interbody fusion (OTLIF) to minimize iatrogenic soft tissue damage and prevent denervation and atrophy of the paraspinal trunk musculature. Potential disadvantages of MIS-TLIF are inadequate neural element decompression and higher risk of cage migration, resulting in persistent symptoms and a need for reoperation. Other disadvantages include inadequate visualization of bony landmarks for instrumentation, and less robust postero-lateral arthrodesis than open approaches, which may affect fusion rates. Several studies have reviewed the differences between both treatments for degenerative lumbar disease, but they mainly focused on the perioperative and short-term post-operative outcomes. Since the potential disadvantages of MIS may be expected after a longer follow-up, we performed a meta-analysis comparing MIS-TLIF with O-TLIF for long-term outcomes.
Questions/purposes: In this systematic review, we compared clinical outcome of MIS and open single level TLIF for degenerative lumbar disease with a minimum follow-up of 2 years, with regard to [1] clinical outcomes (VAS pain scores and Oswestry Disability Index [ODI], [2] adverse events (reoperation, revision, readmission, implant failure rate, infection, cage migration, cage extrusions), and [3] Fusion rate.
Conclusion: This meta-analysis will provide a detailed summary of the long-term clinical outcome of minimally invasive versus open single-level transforaminal lumbar interbody fusion for degenerative lumbar diseases. Previous meta-analyses have been published, but all focused on the peri-operative or short-term outcomes. This meta-analysis is the first in including only studies with a minimum follow-up of 2 years.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."