Case Report
Congenital Quadricuspid Aortic Valve, a Rare Cause of Aortic Insufficiency in Adults: Case Report
Cyrus Kocherla* and Kalgi Modi
Department of Cardiology, Louisiana State University Medical Center, Shreveport, Louisiana
*Address for Correspondence: Cyrus Kocherla, Department of Cardiology, Louisiana State University Medical Center, Shreveport, Louisiana, Email: [email protected]
Dates: Submitted: 16 December 2016; Approved: 19 January 2017; Published: 23 January 2017
How to cite this article: Kocherla C, Modi K. Congenital Quadricuspid Aortic Valve, a Rare Cause of Aortic Insufficiency in Adults: Case Report. J Cardiol Cardiovasc Med. 2017; 2: 003-007.
DOI: 10.29328/journal.jccm.1001005
Copyright License: © 2017 Kocherla C, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
INTRODUCTION
Quadricuspid aortic valve (QAV) is rare congenital malformation of the aortic valve with estimated prevalence of 0.013% to 0.043% [1-4]. QAV is most commonly associated with aortic insufficiency (AI), which is found in almost 75% of cases [5]. QAV can also be associated with other cardiac defects such as ventricular or atrial septal defects, patent ductus arteriosus, subaortic fibromuscular stenosis, malformation of the mitral valve, and coronary anomalies [3]. Up to 40% of all patients with QAV undergo aortic valve replacement surgery most commonly due to progressive AI in 88% of case [2,3,6]. Here we report a case from our institution of a woman with QAV with severe AI and anomalous origin of the right coronary artery.
CASE REPORT
A 58-year-old African American woman with history of uncontrolled hypertension, obesity, recurrent pancreatitis and hypothyroidism on replacement therapy who presented with complaints of chest pain and progressive dyspnea on exertion with carrying out activities of daily living.
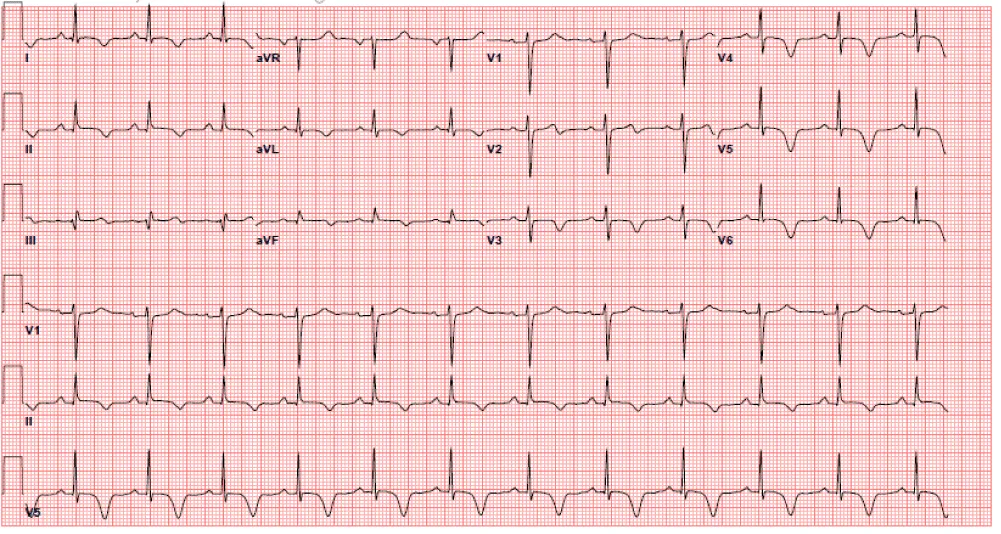
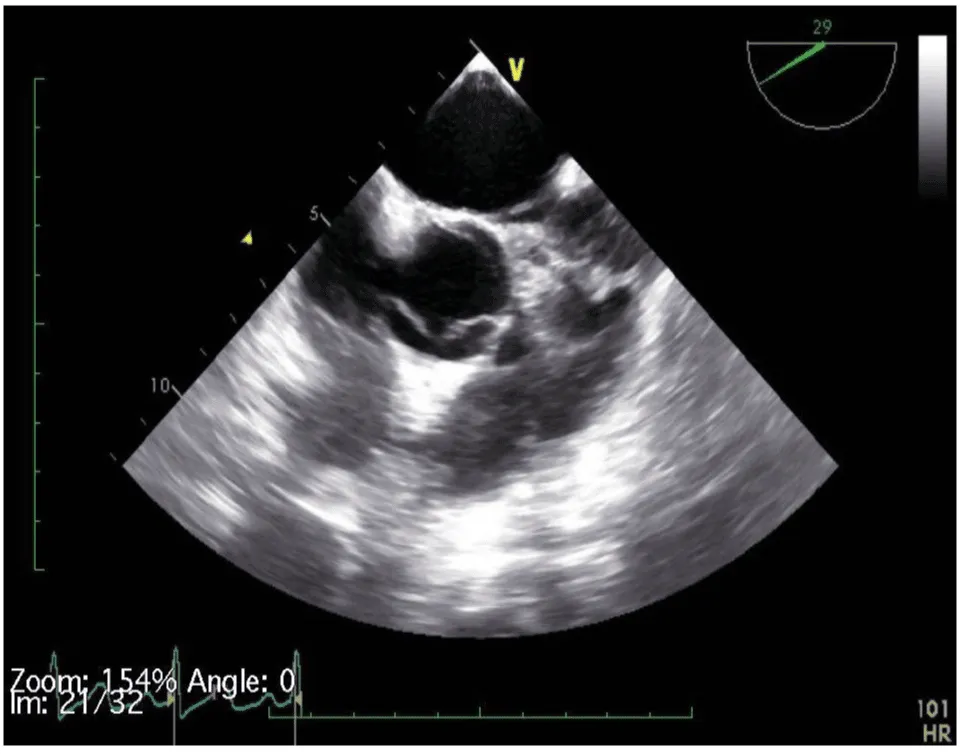
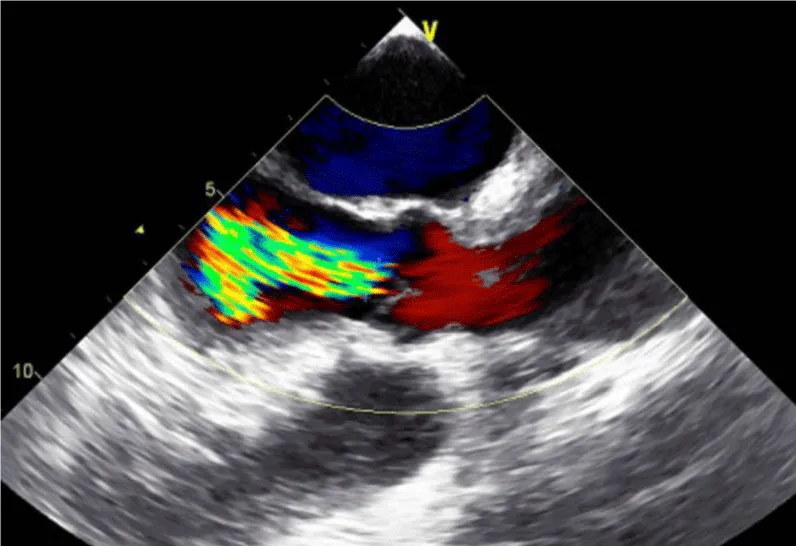
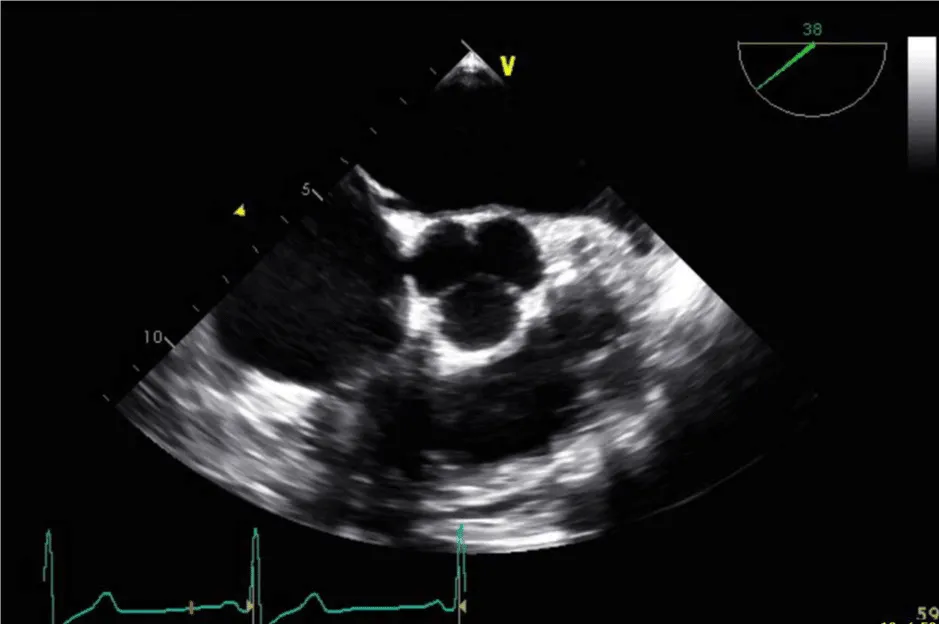
Her initial vital signs upon presentation to the hospital were; blood pressure: 161/76 mm Hg, heart rate: 96 beats per minute, respiratory rate: 27 breaths per minute. Physical exam revealed a cardiac auscultation findings of a grade 2 diastolic murmur which was loudest at the 2nd right intercostal space as well as a grade 2 systolic flow murmur. Cardiac biomarkers were elevated with initial troponin-I of 0.33 ng/mL, peak of 2.28 ng/mL and subsequent down trend. Electrocardiography (Figure 1) showed sinus rhythm with anterior and inferolateral T wave inversion and chest radiograph (Figure 2) was unremarkable. She underwent coronary angiography which revealed normal coronary arteries. The takeoff of the right coronary artery (RCA) was noted to be superior and anterior to its normal position (Figures 3A and 3B). Transthoracic and transesophageal echocardiography (TEE) revealed normal left ventricular systolic function and severe insufficiency of the aortic valve with Quadricuspid morphology (Figure 4A in Diastole, Figure 4B in Systole, Figure 4C Long Axis of the aortic valve). She underwent aortic valve replacement with a # 19mm ON-X mechanical valve. Intraoperatively it was noted that the ostium of the right coronary artery was over the aberrant leaflet. Her postoperative course was complicated by the development of supraventricular tachycardia, posteriorly localized pericardial effusion, severe hemolytic anemia, renal failure and pancreatitis leading to her death eleven days after the surgery.
DISCUSSION AND CONCLUSION
QAV is a congenital malformation of the aortic valve, which is rarely encountered with an estimated prevalence of 0.013% to 0.043% with nearly equal gender distribution [1-4]. Most cases of QAV reported in the literature have been encountered incidentally intraoperatively during aortic valve surgery or autopsy. The most common associated valvular abnormality is AI, with isolated AI in 75% of cases [5]. QAV is also associated with anomalous origin of coronary arteries in up to 10% of cases [5,7]. Several hypotheses have been proposed to explain the development of congenital QAV, however the mechanism still remains poorly understood. During embryogenesis, normally after the septation of the cardiac outflow tract or conotruncus, three mesenchymal swellings develop into semilunar leaflets of the aortic valve. In cases of congenital QAV, animal studies have suggested that the supernumerary cusp may result from the division of one of the three mesenchymal ridges, which normally form the leaflets of the aortic valve during valvulogenesis [8]. The development of the aortic valve leaflets normally occurs just after the development of the coronary artery origins from the sinuses of valsalva. Studies in rodents have shown that in congenital QAV, the division of the valve cushion starts at a very early stage of valve formation. It may be possible that abnormalities of the aortic cusps could be related embryo logically to the development of coronary artery anomalies [6,8-11].
QAV dysfunction is absent or minimal at an early age with the mean date of recognition in about the 5th or 6th decade of life. The management of QAV is related to presence of AI and about 45.2% of patients with QAV undergo AVR in adulthood for progressive AI [10]. The mechanism behind the development of AI is thought to be due to the uneven distribution of shear stress and also due to abnormal leaflet coaptation [3,12].
In our case as we described, the QAV was noted to have three equal sized cusps and one larger cusp and is a type E valve according to the 1973 Hurwitz and Roberts’s classification [4]. Congenital QAV predisposed her to the development of severe AI and was associated with the finding of an anomalous origin of the right coronary artery. The RCA originated from the right dorsal or posterior cusp of the aortic valve and the left main coronary artery originated from the left ventral or anterior cusp, nomenclature of the cusp orientation is as proposed by Fernandez et al. [13]. In their study of quadricuspid aortic valves in Syrian hamsters [13]. The supernumerary cusp was identified as the right dorsal cusp and the RCA originated from that corresponding right dorsal sinus which was identified intraoperatively. Although the presence of the patient’s comorbidities such as uncontrolled HTN, obesity and recurrent pancreatitis did not have a causal relationship with the finding of QAV or the development of severe AI, they likely played a role in her post-surgical mortality.
In our case as we described, the QAV was noted to have three equal sized cusps and one larger cusp and is a type E valve according to the 1973 Hurwitz and Roberts’s classification [4]. Congenital QAV predisposed her to the development of severe AI and was associated with the finding of an anomalous origin of the right coronary artery. The RCA originated from the right dorsal or posterior cusp of the aortic valve and the left main coronary artery originated from the left ventral or anterior cusp, nomenclature of the cusp orientation is as proposed by Fernandez et al. [13]. In their study of quadricuspid aortic valves in Syrian hamsters [13]. The supernumerary cusp was identified as the right dorsal cusp and the RCA originated from that corresponding right dorsal sinus which was identified intraoperatively. Although the presence of the patient’s comorbidities such as uncontrolled HTN, obesity and recurrent pancreatitis did not have a causal relationship with the finding of QAV or the development of severe AI, they likely played a role in her post-surgical mortality.
In our case as we described, the QAV was noted to have three equal sized cusps and one larger cusp and is a type E valve according to the 1973 Hurwitz and Roberts’s classification [4]. Congenital QAV predisposed her to the development of severe AI and was associated with the finding of an anomalous origin of the right coronary artery. The RCA originated from the right dorsal or posterior cusp of the aortic valve and the left main coronary artery originated from the left ventral or anterior cusp, nomenclature of the cusp orientation is as proposed by Fernandez et al. [13]. In their study of quadricuspid aortic valves in Syrian hamsters [13]. The supernumerary cusp was identified as the right dorsal cusp and the RCA originated from that corresponding right dorsal sinus which was identified intraoperatively. Although the presence of the patient’s comorbidities such as uncontrolled HTN, obesity and recurrent pancreatitis did not have a causal relationship with the finding of QAV or the development of severe AI, they likely played a role in her post-surgical mortality.
The diagnosis of QAV was facilitated by TEE, which revealed the characteristic findings. The short axis views of the aortic valve are optimal for making the diagnosis of QAV. The classic X shaped commissural aortic valve pattern in diastole (Figure 4B) compared to the Y shape of a trileaflet valve is diagnostic (Figure 4D) [3].
With the increasing use of advanced imaging modalities such as TEE, cardiac CT and cardiac MRI, the incidence of QAV is reported to be increasing [3,12]. The majority of patients develop progressive valvular dysfunction requiring surgery and any delay in diagnosing QAV is presumably associated with worse outcomes surgically when these patients do undergo aortic valve surgery. In our case the patient’s significant preoperative comorbidities likely played a role in increasing her postsurgical mortality although not directly causative of severe valvular heart disease. Therefore, early detection is essential and it is important to recognize the characteristic morphological features on echocardiography to aid in the accurate diagnosis and treatment of rare congenital aortic valve disease.
REFERENCES
- Larson EW, Edwards WD. Risk factors for aortic dissection: a necropsy study of 161 cases. Am J Cardiol. 1984; 53: 849-855. Ref.: https://goo.gl/1LZd8G
- Feldman BJ, Khandheria BK, Warnes CA, Seward JB, Taylor CL, et al. Incidence, description and functional assessment of isolated quadricuspid aortic valves. Am J Cardiol. 1990; 65: 937-938. Ref.: https://goo.gl/M1zMvm
- Jagannath AD, Johri AM, Liberthson R, Larobina M, Passeri J, et al. Quadricuspid aortic valve: a report of 12 cases and a review of the literature. Echocardiography. 2011; 28: 1035-1040. Ref.: https://goo.gl/b0yHGJ
- Hurwitz LE, Roberts WC. Quadricuspid semilunar valve. Am J Cardiol. 1973; 31: 623-626. Ref.: https://goo.gl/poCmHJ
- Tutarel O. The quadricuspid aortic valve: a comprehensive review. J Heart Valve Dis. 2004; 13: 534-537. Ref.: https://goo.gl/9CK1vb
- Timperley J, Milner R, Marshall AJ, Gilbert TJ. Quadricuspid aortic valves. Clin Cardiol. 2002; 25: 548-52. Ref.: https://goo.gl/zY3icV
- Tutarel O. Quadricuspid aortic valves and anomalies of the coronary arteries. Journal of Thoracic and Cardiovascular Surgery. 2004; 127: 897. Ref.: https://goo.gl/w9ncy8
- Fernández B, Fernández MC, Durán AC, López D, Martire A, et al. Anatomy and formation of congenital bicuspid and quadricuspid pulmonary valves in Syrian hamsters. Anat Rec. 1998; 250: 70-79. Ref.: https://goo.gl/b3eEgA
- Zhu J, Zhang J, Wu S, Zhang Y, Ding F, et al. Congenital quadricuspid aortic valve associated with aortic insufficiency and mitral regurgitation. J Cardiothorac Surg. 2013; 8: 87. Ref.: https://goo.gl/nk3An1
- Idrees JJ, Roselli EE, Arafat A, Johnston DR, Svensson LG, et al. Outcomes after repair or replacement of dysfunctional quadricuspid aortic valve. J Thorac Cardiovasc Surg. 2015; 150: 79-82. Ref.: https://goo.gl/pcqJow
- Bogers AJ, Gittenberger-de Groot AC, Poelmann RE, Péault BM, Huysmans HA. Development of the origin of the coronary arteries, a matter of ingrowth or outgrowth? Anat Embryol (Berl). 1989; 180: 437-441. Ref.: https://goo.gl/v3Uca2
- Tsang MY, Abudiab MM, Ammash NM, Naqvi TZ, Edwards WD, et al. Quadricuspid aortic valve: Characteristics, Associated Structural Cardiovascular Abnormalities, and Clinical Outcomes. Circulation. 2016; 133: 312-319. Ref.: https://goo.gl/6lPaSu
- Fernández B, Durán AC, Martire A, López D, Sans-Coma V. New embryological evidence for the formation of quadricuspid aortic valves in the Syrian hamster (Mesocricetus auratus). J Comp Pathol. 1999; 121: 89-94. Ref.: https://goo.gl/ybppoe