Research Article
Value of electrocardiographic T wave inversion in lead aVL in prediction of Mid Left Anterior Descending Stenosis in patients with stable Coronary Artery disease
Gehan Magdy* and Awad Yousef
Cardiology department, Faculty of medicine, Alexandria University, Egypt
*Address for Correspondence: Dr. Gehan Magdy, Cardiology Department, Faculty of Medicine, Alexandria University, Egypt, Tel: 00201017802182; Email: [email protected]
Dates: Submitted: 31 July 2017; Approved: 17 August 2017; Published: 18 August 2017
How to cite this article: Magdy G, Yousef A. Value of electrocardiographic T wave inversion in lead aVL in prediction of Mid Left Anterior Descending Stenosis in patients with stable Coronary Artery disease J Cardiol Cardiovasc Med. 2017; 2: 056-062.
DOI: 10.29328/journal.jccm.1001015
Copyright License: © 2017 Magdy G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: T wave inversion; Left anterior descending artery; Stable coronary artery disease
Abbreviations: CAD: Coronary artery disease; ECG: Electrocardiogram; LAD: The left anterior descending coronary artery; LCX: Left circumflex coronary artery; LV: Left ventricular; LM: Left main coronary artery: RCA: Right coronary artery
ABSTRACT
Background: The electrocardiogram (ECG) is a simple and noninvasive bedside diagnostic tool with a well-established role in the diagnosis of coronary artery disease (CAD). We aimed to study the diagnostic value of electrocardiographic ST-T wave changes in lead aVL in prediction of site of coronary artery stenosis in patients with chronic stable angina.
Patients and Methods: study was conducted on 156 patients referred for invasive coronary angiography with history of stable CAD as proved by non- invasive tests, 12 lead ECG was recorded and fully interpreted with more focus on T wave direction in aVL lead. T waves in aVL were categorized into one of three groups: upright, flat or inverted.
Results: regarding T wave in lead aVL, inverted T wave was reported in 71(45.5%) patients, 58 (37.2%) patients were with upright T wave in lead aVL and 27(17.3%) patients were with flat T wave in lead aVL, and we found that inverted T wave in lead aVL was most evident in 56(73.7%) patients with mid LAD with (highest κ value equal to 0.550[moderate agreement], and p value<0.001.
Conclusions: This study confirmed the diagnostic value of T wave inversion in lead aVL in prediction of mid left anterior descending artery lesions in patients with stable coronary artery disease.
INTRODUCTION
Coronary artery disease (CAD) is an important cause of death, complications and resource use throughout the industrial and developing world [1]. It is estimated that 1 in 3 adults in the United States has some form of cardiovascular disease, including 13 million with CAD and nearly 9 million with angina pectoris [2]. The electrocardiogram (ECG) is a simple and noninvasive bedside diagnostic tool with a well-established role in the diagnosis of CAD. For instance, T wave inversion in anterior or inferior location and or ST-segment depression has been associated with high incidence of CAD [3-8]. The management of proximal obstructive CAD is more important as larger myocardial areas are supplied downstream from the stenosis. The left anterior descending coronary artery (LAD) which supplies 40% to 50% of total left ventricular (LV) myocardium and may result in major ischemic damage, for this reason early detection of LAD stenosis has a vital role for patients with CAD to avoid damaging a large functional part of LV [9-12]. We aimed to study the diagnostic value of electrocardiographic ST-T wave changes in lead aVL in prediction of site of coronary artery stenosis in patients with chronic stable angina.
METHODS
Study populations
This study is a prospective observational study was conducted in one year between January 2015 to December 2015 , and included 156 patients referred to Alexandria main University hospital for invasive coronary angiography with history of stable CAD as proved by non- invasive tests (ECG, stress echocardiography, treadmill exercise, myocardial perfusion imaging or multi-slice computed tomography coronary angiography),exclusion criteria were clinical situations that may result in secondary aVL lead T wave inversion and /or ST segment depression as bundle branch block either left or right, left ventricular hypertrophy and strain and paced ventricular rhythms.
METHODS
An informed consent was obtained from all patients, and the study was approved by the ethical committee. Each patient was subjected to:
Clinical evaluation
Including full history taking including age, gender, CAD risk factors, clinical examination including heart rate and blood pressure.
Electrocardiogram [13]
ECG was recorded in a 12-lead format at a paper speed of 25 mm/s and fully interpreted with more focus on T wave direction in aVL lead. T waves in aVL were categorized into one of three groups: upright, flat or inverted and ST segment were categorized as isoelectric, depressed or elevated.
Coronary angiography [13,14]
It was done to all patients, the left main coronary artery (LM), LAD, left circumflex (LCX), and right coronary artery (RCA) were defined and plotted on the data sheet. The ostial lesion was defined as lesion affecting the origin of the vessel and or within 3 millimeters (mm) from the origin. Proximal LAD was defined as segment 3 mm from LAD origin to the first diagonal branch (D1), mid LAD from D1 to second diagonal branch (D2) and distal LAD segment was beyond D2.Proximal LCX was defined as segment 3 mm after the origin of LCX to first obtuse marginal branch (OM1), mid LCX from OM1 to second obtuse marginal branch (OM2) and distal LCX was the segment beyond OM2.Proximal RCA 3 mm from RCA origin to the right ventricular branch, mid RCA from the right ventricular branch to RCA bifurcation and distal RCA was the segment beyond its bifurcation .Regarding lesion severity significant coronary artery disease is considered when lesion is ≥50% luminal narrowing.
STATISTICAL ANALYSIS
Statistical analysis was performed using SPSS 20 (Chicago, IL, USA).Continuous variables were presented as mean±SD, categorical variables were expressed as percentages and evaluated with a Chi square test or Fisher’s exact test. In order to determine the predictive value of the T wave inversion the kappa coefficient was used to measure inter rater agreement for categorical items. Binary regression analysis was used to determine the most significant predictors of LAD stenosis. A probability value of p<0.05 was considered significant.
RESULTS
Basic characteristics
In this study 156 patients previously diagnosed chronic stable angina on clinical basis were included, 120 patients (76.9%) were males, their mean age 56.37±11.07 years. Smoking and hypertension were the most prevalent risk factors, 101(64.7%) patients were smokers, 94(60.3%)patients were hypertensive controlled on medications, 77(49.4%) patients were dyslipidemic, 65(41.6%) were diabetics, 60(38.5%) patients with family history of CAD and 12(7.7%) patients were with history of old cerebrovascular accidents, all patients were on full medical treatment for chronic stable angina including betablockers in 156(100%), acetyl salicylic acid in 156(100%) , oral nitrates in 135(86.5%), nicorandil in 21(13.4%), statins in 156(100%), angiotensin converting enzyme inhibitors in 45(28.8%). By examination the mean systolic blood pressure was 134.29±17.49mmHg, the mean diastolic blood pressure was 81.70±9.71mmHg, the mean heart rate was 65.32±10.25.
Angiographic data
Normal coronary angiograms were present in 21(13.5%), one vessel disease in 62(39.7%), 2 vessel disease in 48(30.8%), and multivessel disease were in 25(16%) of cases, the LAD was the most commonly affected coronary artery in 109(69.9%), followed by the RCA in 64(41%), and the LCX was in 54(34.6), and LM was in 9(5.8%) patients.
Regarding the segmental coronary artery stenosis distribution we found that the most common coronary artery affected in our study was the LAD, and among LAD lesions mid LAD lesions were the most prevalent than other LAD lesions accounting 76(48.7%), proximal LCX lesions 30(19.2%) were the most in all LCX lesions, also the mid RCA lesions 35(22.4%) were the common in all RCA lesions (Table 1).
| Table 1: Segmental distribution of the coronary arteries in the patients. | |||
| No (%) | LAD (n = 109) |
LCX (n = 54) |
RCA (n = 64) |
| Ostial | 1(0.6) | 19(12.2) | 10(6.4) |
| Proximal | 36(23.1) | 30(19.2) | 23(14.7) |
| Mid | 76(48.7) | 7(4.5) | 35(22.4) |
| Distal | 16(10.3) | 11(7.1) | 17(10.9) |
| LAD: Left Anterior Sescending, LCX: Left Circumflex, RCA: Right Coronary Artery. | |||
ECG data
In our study 144(92.3%) patients were in sinus rhythm and only 12(7.7%) patients were in atrial fibrillation and the mean heart rate was 74.29±13.13bpm.
Regarding T wave in lead aVL, inverted T wave was reported in 71(45.5%) patients [60(38.5%)patients was with isolated T wave inversion in lead aVL, and 11(7.1%)patients was in aVL and other leads], 58 (37.2%) patients were with upright T wave in lead aVL and 27(17.3%) patients were with flat T wave in lead aVL.
Regarding ST segment in lead aVL, it was isoelectric in a large number of patient 126 patients (80.8%), depressed ST segment in 27 patients (17.3%) and elevated ST segment in 3 patients (1.9%). Other ECG abnormalities as (frequent premature contractions, poor R progression, T wave alternans) were present in about 14(9%) patients.
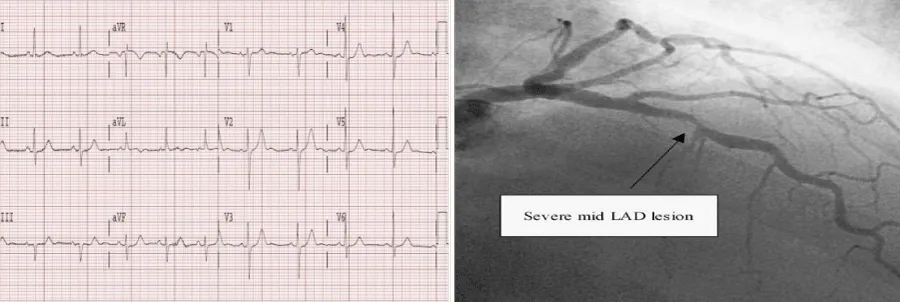
So the T wave inversion in lead aVL was the most common ECG finding in patients with stable CAD and we study its distribution according to different segmental stenosis of CAD as ( Table 2) and we found that T wave inversion in lead aVL was most common in 56(73.7%) patients with mid LAD stenosis (Figure 1).
| Table 2: Distribution of T wave inversion in lead aVL according to different coronary artery segmental stenosis. | ||||
| Inverted T with in lead aVL | ||||
| No (n = 85) |
Yes (n = 71) |
|||
| No | % | No | % | |
| LM | 6 | 7.1 | 3 | 4.2 |
| Ostial LAD | 1 | 1.2 | 0 | 0.0 |
| Proximal LAD | 25 | 29.4 | 11 | 15.5 |
| Mid LAD | 20 | 23.5 | 56 | 78.9 |
| Distal LAD | 16 | 18.8 | 0 | 0.0 |
| Ostial LCX | 18 | 21.2 | 1 | 1.4 |
| Proximal LCX | 26 | 30.6 | 4 | 5.6 |
| Mid LCX | 2 | 2.4 | 5 | 7.0 |
| Distal LCX | 7 | 8.2 | 4 | 5.6 |
| Ostial RCA | 0 | 0.0 | 10 | 14.1 |
| Proximal RCA | 19 | 22.4 | 4 | 5.6 |
| Mid RCA | 28 | 32.9 | 7 | 9.9 |
| Distal RCA | 12 | 14.1 | 5 | 7.0 |
| LAD: Left Anterior Descending, LCX: Left Circumflex, RCA: Right Coronary Artery | ||||
Figure 1: Example of isolated T wave inversion in lead aVL and the coronary angiogram of that case showed significant mid LAD stenosis as shown by black arrow.
To study the significance of T wave inversion in lead aVL in prediction of mid LAD stenosis using the Kappa test (κ), (highest κ value equal to 0.550[moderate agreement], and highest accuracy of 77.56%, and it was statistically significant p value<0.001), also the binary logistic regression for the parameters that affecting mid LAD stenosis revealed that T wave inversion in lead aVL was the only abnormal finding that predicted mid LAD lesions (B=1.869,odds ratio 6.480, 95%, confidence interval LL2.421- UL17.344, <0.001).
DISCUSSION
The ECG remains the key test in the diagnosis of acute and chronic coronary syndromes [15,16]. In the setting of acute coronary syndrome, several ECG findings help to localize the occlusion site of the LAD coronary artery with respect to its major branches as ST segment elevation in lead aVR was found to be very useful in identifying LAD occlusion proximal to first septal perforator [17,18]. Until now the value of T wave changes in lead aVL in diagnosing CAD in patients with chronic stable angina has not yet been well addressed in literature , and might be considered non-significant by most physicians. There is accumulating evidence however, that changes in lead aVL have significance for patients [19-21]. In our study we found that inverted T wave in lead aVL is mainly diagnostic for mid LAD stenosis in patient with stable CAD. It was difficult for us to find several studies to be compared with our study as a limited number of studies had indicated that ST segment or T wave abnormality in specific leads can be an early sign of a significant lesion in a specific coronary artery. Farhan et al. [13], analyzed ECGs of 257 consecutive patients undergoing coronary angiography, all patients had chronic stable angina, all patients with secondary T wave inversion had been excluded (66 patients). The remaining 191 patients constituted the study population and found that T wave inversion in aVL was found to be the only ECG variable significantly predicting mid segment (LAD) lesions (Odds Ratio 2.93, 95% Confidence Interval 1.59-5.37, p=0.001. which is totally in agreement to our study , also Hassen GW et al. [22]. In a multidisciplinary prospective study, a single ECG with isolated T wave inversion in lead aVL that was interpreted by the computer as normal was given to all participants to interpret in writing. The readings by all physicians were compared by level of education and by specialty to one another and to the computer interpretation. They found of the 191 physicians participated in the study 48 (25.1%) identified and143 (74.9%) did not identify the isolated T wave inversion in lead aVL, and at the end of the study they showed a case report of the association of inverted T wave in the ECG and the mid LAD stenosis and concluded that subtle ECG findings should be emphasized in their training so as not to miss significant findings that could cause morbidity and mortality. Also Hassen GW et al., in another study [23], concluded in his review article T wave inversion alone in lead aVL with no pathologic QS and/or ST-T changes in other leads is usually described as normal ECG by the referring physicians and computer assisted ECG interpretation. The aforementioned cases and studies highlight the importance of the ECG changes in lead aVL and their prognostic significance. Health care providers should be alert of T wave inversion in aVL especially in presence of major risk factors for CAD and in absence of secondary causes that might alter the polarity of T wave. This will help early detection and treatment of patients with stable CAD.
STUDY LIMITATIONS
The study is limited by its small sample size and by the study population, which only included patients with stable coronary artery disease and did not include those with acute coronary syndromes.
CONCLUSIONS
This study confirmed the diagnostic value of T wave inversion in lead aVL in prediction of mid left anterior descending artery lesions in patients with stable coronary artery disease.
REFERENCES
- Gaziano JM, Manson J, Ridker PM. A Textbook of Cardiovascular Medicine 8th ed Philadelphia, PA: Saunders Elsevier. 2007.
- Mensah GA, Brown DW. An overview of cardiovascular disease burden in the United States. Health Aff (Millwood). 2007; 26: 38-48. Ref.: https://goo.gl/Ay6Fff
- Masood Ali Akbar, Imran Waheed, Salman Munir, Shahid Amin, Nadeem Hayat Mallick. Study of electrocardiographic t wave inversion in patients with tight mid left anterior descending artery stenosis. Cardiovasc Dis. 2014; 12: 30-32.
- Nyman I, Areskog M, Areskog NH, Swahn E, Wallentin L. The RISC Study Group. Very early risk stratification by electrocardiogram at rest in men with suspected unstable coronary heart disease. J Intern Med. 1993; 234: 293-301. Ref.: https://goo.gl/J34NZQ
- Okada M, Yotsukura M, Shimada T, Ishikawa K. Clinical implications of isolated T wave inversion in adults: electrocardiographic differentiation of the underlying causes of this phenomenon. J Am Coll Cardiol. 1994; 24: 739-745. Ref.: https://goo.gl/LbLea3
- De Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982; 103: 730-736. Ref.: https://goo.gl/FbfUVC
- Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med. 2002; 20: 638-643. Ref.: https://goo.gl/q7ZhNQ
- Chatterjee K, Harris A, Davies G, Leatham A. Electrocardiographic changes subsequent to artificial ventricular depolarization. Br Heart J. 1969; 31: 770-779. Ref.: https://goo.gl/yGNn9z
- Gorgels AP, Vos MA, Mulleneers R, De Zwaan C, Bär FW, et al. Value of the electrocardiogram in diagnosing the number of severely narrowed coronary arteries in rest angina pectoris. Am J Cardiol. 1993; 72: 999-1003. Ref.: https://goo.gl/Piw9km
- Engelen DJ, Gorgels AP, Cheriex EC, De Muinck ED, Ophuis AJ, Dassen WR, et al. Value of the electrocardiogram in localizing the occlusion site in the left anterior descending coronary artery in acute anterior myocardial infarction. J Am CollCardiol. 1999; 34: 389-395. Ref.: https://goo.gl/n9EjpY
- Tamura A, Kataoka H, Mikuriya Y, Nasu M. Inferior ST segment depression as a useful marker for identifying proximal left anterior descending artery occlusion during acute anterior myocardial infarction. Eur Heart J. 1995; 16: 1795-1799. Ref.: https://goo.gl/bjJB7J
- Hassen GW, Costea A, Smith T, Carrazco C, Hussein H, et al. The neglected lead on electrocardiogram: T wave inversion in lead aVL, nonspecific finding or a sign for left anterior descending artery lesion? J Emerg Med. 2014; 46: 165-170. Ref.: https://goo.gl/CEaEid
- Farhan HL, Hassan KS, Al-Belushi A, Sallam M, Al-Zakwani I. Diagnostic Value of Electrocardiographic T Wave Inversion in Lead aVL in Diagnosing Coronary Artery Disease in Patients with Chronic Stable Angina.Oman Med J.2010; 25: 124-127. Ref.: https://goo.gl/kvJmjf
- Jukema JW, Vliegen HW, Bruschke AVG. Coronary angiography: principles, technique and interpretation. 1e druk, Leiden, the Netherlands, 2009. Chapter 3: 23-34.
- Zimetbaum PJ, Josephson ME. Use of the electrocardiogram in acute myocardial infarction. New England Journal of Medicine. 2003; 348: 933-940.
- Goldberger AL. Clinical Electrocardiography: A Simplified Approach, 7th ed. St. Louis, Mosby/Elsevier 2006.
- Quyyumi AA, Crake T, Rubens MB, Levy RD, Rickards AF, Fox KM. Importance of “reciprocal” electrocardiographic changes during occlusion of left anterior descending coronary artery. Studies during percutaneous transluminal coronary angioplasty. Lancet. 1986; 1: 347-350. Ref.: https://goo.gl/o7coq6
- Tamura A, Kataoka H, Mikuriya Y, Nasu M. Inferior ST segment depression as a useful marker for identifying proximal left anterior descending artery occlusion during acute anterior myocardial infarction. Eur Heart. J 1995; 16: 1795-1799. Ref.: https://goo.gl/dLcQpT
- Hanna EB, Glancy DL. ST-segment depression and T-wave inversion: classification, differential diagnosis, and caveats. Cleve Clin J Med. 2011; 78: 404-414. Ref.: https://goo.gl/mJZabJ
- Rashduni DL, Tannenbaum AK. Utility of ST segment depression in lead AVL in the diagnosis of right ventricular infarction. N J Med. 2003; 100: 35-37. Ref.: https://goo.gl/UJRU7T
- Turhan H, Yilmaz MB, Yetkin E, Atak R, Biyikoglu SF, et al. Diagnostic value of aVL derivation for right ventricular involvement in patients with acute inferior myocardial infarction. Ann Noninvasive Electrocardiol. 2003; 8: 185-188. Ref.: https://goo.gl/h6A56h
- GetawWorku Hassen, Ana Costea, Claire Carrazco, Tsion Frew, Anand Swaminathan, et al. Isolated T Wave Inversion in Lead aVL: An ECG Survey and a Case Report. Emerg Med Int. 2015. Ref.: https://goo.gl/AYsoem
- Getaw Worku Hassen, Soheila TalebiGeorge Fernaine, Hossein Kalantari. Lead aVL on electrocardiogram: emerging as important lead in early diagnosis of myocardial infarction? Am J Emerg Med. 2014; 32: 785-788. Ref.: https://goo.gl/iavH1S