More Information
Submitted: 02 December 2019 | Approved: 13 December 2019 | Published: 16 December 2019
How to cite this article: Szabo S, Hoffmeister HM. Aortic dissection causing 2 myocardial infarctions. J Cardiol Cardiovasc Med. 2019; 4: 233-235.
DOI: 10.29328/journal.jccm.1001074
Copyright License: © 2019 Szabo S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Aortic dissection causing 2 myocardial infarctions
Sebastian Szabo1* and Hans Martin Hoffmeister2
1Kardiopraxis Langenfeld, Langenfeld, Germany
2Städtisches Klinikum, Department of Internal Medicine II, Solingen, Germany
*Address for Correspondence: Dr. med. Sebastian Szabo, MD, Kardiopraxis Langenfeld, Hitdorfer Str. 10c 40764 Langenfeld, Germany, Tel: +49 2173/71026; Fax: +49 2173/994070; Email: [email protected]
A 56-year-old man was admitted to our hospital because of sudden onset of right-sided thoracic pain. The ECG showed inferior ST segment elevations. He has been treated with aspirin, clopidogrel, unfractionated heparin and tenecteplase, and his symptoms resolved after 30 minutes. About half an hour later, the patient developed again left-sided thoracic pain and the signs of an anterior myocardial ST-segment elevation infarction. 90 minutes after receiving the initial medications, the performed coronary angiography revealed a long dissection of a large ramus circumflexus. Furthermore, the left anterior descending coronary artery was occluded at about the mid-level. The left ventriculography showed a reduced ventricular function and a Stanford type A aortic dissection. Immediate patient transfer for emergency surgical intervention was arranged. However, ventricular fibrillation occurred during transport and he required endotracheal intubation and prolonged cardiopulmonary resuscitation. Unfortunately, he died during further transport.
In a patient with massive thoracic pain of initially uncommon localization in combination with fluctuation of ST-segment elevations, aortic dissection should be seriously taken into the differential diagnosis as well as into therapeutic management decisions (in particular antiplatelet and thrombolytic therapy).
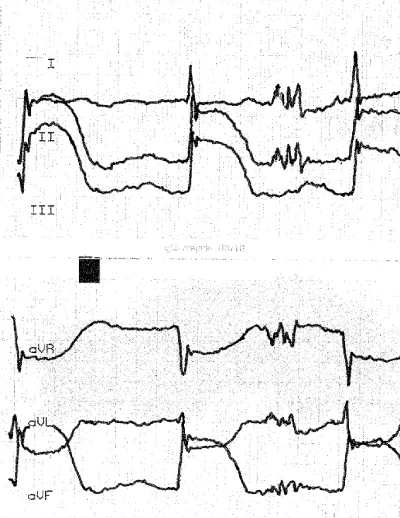
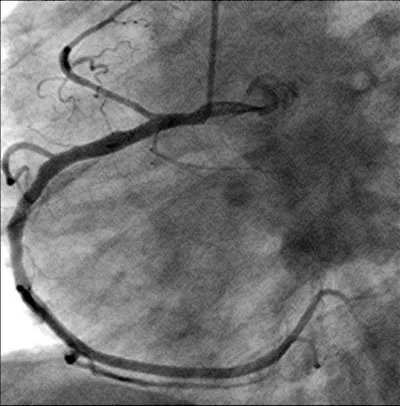
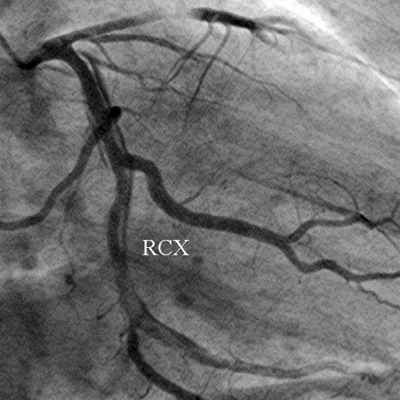
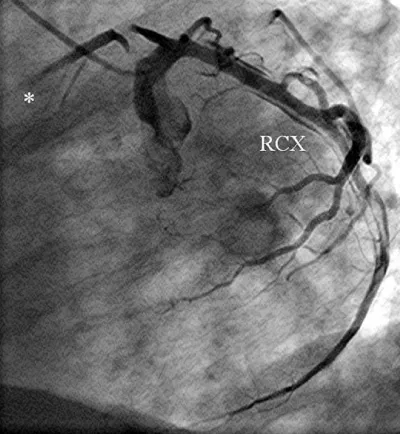
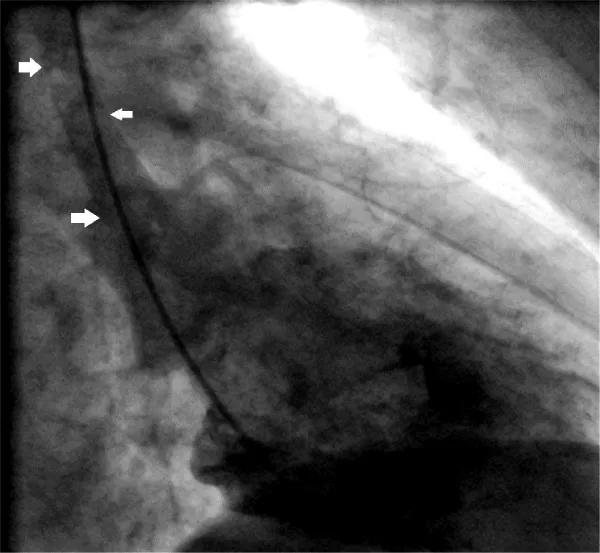
A 56-year-old obese man with a history of hypertension was admitted at night to the department of cardiology of our hospital because he had developed sudden onset right-sided thoracic pain with radiation into the right shoulder and right arm. He was sweating profusely and had massive nausea. The initially performed 12-lead ECG showed marked inferior ST segment elevations (Figure 1). Beside analgetics and oxygen, he was treated with aspirin, clopidogrel, heparin and the fibrin-specific thrombolytic tenecteplase. His symptoms resolved after 30 minutes. However, half an hour later, he developed left-sided thoracic pain, tachycardia, low blood pressure and the ECG signs of anterior ST-segment elevation myocardial infarction. The performed coronary angiography revealed a normal right coronary artery (Figure 2). The left coronary artery showed a long dissection of a large ramus circumflexus (RCX) (Figures 3,4). Additionally, the left anterior descending coronary artery (LAD) was occluded at about the mid-level (Figure 4, asterisk). Afterwards the left ventriculography revealed a reduced function and a Stanford type A aortic dissection with the intimal flap (Figure 5, arrows). Immediate patient transfer for emergency surgical intervention was arranged. During transport, ventricular fibrillation occurred, and he required endotracheal intubation as well as prolonged cardiopulmonary resuscitation. Unfortunately, he died due to a refractory cardiogenic shock during further transport.
Figure 1: The initially performed ECG is showing acute inferior ST-segment elevation myocardial infarction (STEMI).
Figure 2: The right coronary artery is shown.
Figure 3: The left coronary artery is shown (right anterior oblique projection) with a long dissection of a large ramus circumflexus (RCX).
Figure 4: The left coronary artery shows an occlusion of the left anterior descending coronary artery (*) (left anterior oblique projection, RCX: ramus circumflexus).
Figure 5: This figure shows left ventriculography and the patient`s aortic dissection (Stanford type A) with the intimal flap (arrows) (right anterior oblique projection).
Acute aortic dissection in coincidence with coronary malperfusion is a relatively rare but devastating condition with high mortality. Diagnosis of acute thoracic aortic dissection is difficult to make and often missed. In this scenario, untreated coronary artery disease may complicate the clinical course of patients with Stanford type A acute aortic dissection. The role of coronary angiography for the assessment of coronary circulation in these patients is controversial and it is discussed, that this procedure is time consuming with a considerable delay to surgery thus increasing the risk of rupture. However, Kawahito, et al. [1] reported higher mortality rates in patients with type A aortic dissection having coronary malperfusion compared with patients without coronary malperfusion (33.3% vs. 8.2%, p = 0.019). Eden, et al. [2] reviewed their surgical results of a selected patient group with type A acute aortic dissection in combination with coronary artery dissection and demonstrated a hospital mortality rate of 21.4% in this group. Another report [3] of a selected group of patients with type A acute aortic dissection and coronary artery dissection over a 15-year period showed, that the left coronary artery was involved in about 46% of these patients with a hospital mortality of 20%. Therefore, aggressive coronary revascularization together with early aortic repair is essential in the management of these critically ill patients.
Spontaneous coronary artery dissection without type A aortic dissection is a very rare cause of acute myocardial infarction. Most previously reported cases were found in middle-aged women of whom a significant proportion presented during pregnancy or the postpartum period or those using oral contraceptives [4,5].
Our patient had both diagnoses. It seems to be likely, that the initial event was a type A aortic dissection causing first an inferior myocardial infarction by the dissection of the RCX. After a symptom-free time period, the dissection affected the left anterior descending artery and caused a massive anterior myocardial infarction with further complications and the patient´s demise from cardiogenic shock.
In patients presenting with chest pain it may be difficult to discriminate between myocardial infarction and aortic dissection only on the basis of clinical manifestations. Moreover, patients with type A dissection may have ECG changes caused by affection of the coronary flow. In a patient like the described one with massive thoracic pain of initially unusual localization combined with fluctuating ST-segment elevations, aortic dissection should be seriously taken into the differential diagnosis and into therapeutic management decisions (in particular antiplatelet and thrombolytic therapy). A prompt diagnosis remains the cornerstone of effective treatment of aortic dissection and it is the single most important determinant of survival in this patient population.
- Kawahito K, Adachi H, Murata S, Yamaguchi A, Ino T. Coronary malperfusion due to type A aortic dissection: mechanism and surgical management. Ann Thorac Surg. 2003; 76: 1471-1476. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/14602269
- Eren E, Toker ME, Tunçer A, Keles C, Erdogan HB, et al. Surgical management of coronary malperfusion due to type a aortic dissection. J Card Surg. 2007; 22: 2-6. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17239202
- Neri E, Toscano T, Papalia U, Frati G, Massetti M, Cet al. Proximal aortic dissection with coronary malperfusion: presentation, management, and outcome. J Thorac Cardiovasc Surg. 2001; 121: 552-560. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11241091
- Judkins DA, Miller SJ, Capone RJ, Houghton JL. Spontaneous multivessel coronary artery dissection: repeated presentation in a healthy postmenopausal woman. Clin Cardiol. 1999; 22: 677-680. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10526696
- Khan NU, Miller MJ, Babb JD, Ahmed S, Saha PK, et al. Spontaneous coronary artery dissection. Acute Card Care. 2006; 8: 162-171. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17012132