More Information
Submitted: January 09, 2021 | Approved: April 15, 2021 | Published: April 16, 2021
How to cite this article: Das A, Planek MIC, Attanasio S. pVAD-assisted left main DK-Crush Bifurcation PCI Post-ViV TAVR. J Cardiol Cardiovasc Med. 2021; 6: 029-032.
DOI: 10.29328/journal.jccm.1001114
Copyright License: © 2021 Das A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abbreviations: CABG: Coronary Artery Bypass Grafting; DK-Crush: Double Kissing Crush: iFR: Instantaneous Wave Free-Ratio; IVUS: Intravascular Ultrasound; LM: Left Main; NSTEMI: Non-ST Elevation Myocardial Infarction; PCI: Percutaneous Coronary Intervention; PVAD: Percutaneous Left Ventricular Assist Device; SAVR: Surgical Aortic Valve Replacement; TAVR: Transcatheter Aortic Valve Replacement; ViV: Valve-in-Valve
pVAD-assisted left main DK-Crush Bifurcation PCI Post-ViV TAVR
Anshuman Das1, Maria Isabel Camara Planek2 and Steve Attanasio3*
1Division of Cardiology & Interventional Cardiology, Porter Regional Hospital, Valparaiso, IN, Valparaiso, USA
2Department of Internal Medicine, Rush University Medical Center, Chicago, IL 60612, USA
3Assistant Professor, Division of Cardiology & Interventional Cardiology, Rush University Medical Center, Chicago, IL, USA
*Address for Correspondence: Steve Attanasio, Assistant Professor of Medicine, Rush University Medical Center, 1725 W. Harrison St., Chicago, IL 60612, USA, Tel: (312) 942-5020; Fax: (312) 942-4039; Email: [email protected]
We describe successful percutaneous coronary intervention (PCI) of significantly diseased ostial left main (LM) and distal LM bifurcation (Medina 1,1,1) in a patient with a reduced left ventricular ejection fraction and a recent valve-in-valve balloon-expandable TAVR using the DK-Crush technique with the support of a percutaneous left ventricular assist device.
History of presentation and past medical history
A 74-year-old male with past medical history of coronary artery bypass grafting (CABG) and bioprosthetic surgical aortic valve replacement (SAVR, 19 mm St. Jude Biocor) in 2007 presented to our referring hospital in 2015 with a non-ST elevation myocardial infarction (NSTEMI) complicated by cardiogenic shock requiring an intra-aortic balloon pump. The patient was found to have severe, diffuse multivessel disease and occluded vein grafts with only mild disease of the left main at that time. He was referred for redo-CABG and redo-AVR given moderate bioprosthetic aortic valve stenosis and left ventricular (LV) dysfunction with an LV ejection fraction (EF) of 25%. Given a porcelain aorta and acutely decompensated state, the patient was deemed extremely high risk for surgery. After a Heart Team discussion, multivessel percutaneous coronary intervention (PCI) was performed. The patient underwent successful PCI to the proximal left anterior descending (LAD, D1), the proximal left circumflex (LCX), and rotational atherectomy and stent placement to the ostial RCA. He did well for many years with normalization of his LVEF.
Several years later, the patient developed progressive, severe, symptomatic aortic stenosis of his SAVR. As a result, he underwent valve-in-valve (ViV) transcatheter aortic valve replacement (TAVR; Edwards Sapien S3, 20 mm) at our institution. Pre-procedure angiogram showed patent stents with unchanged ostial left main and left main bifurcation mild disease. Post TAVR course was unremarkable.
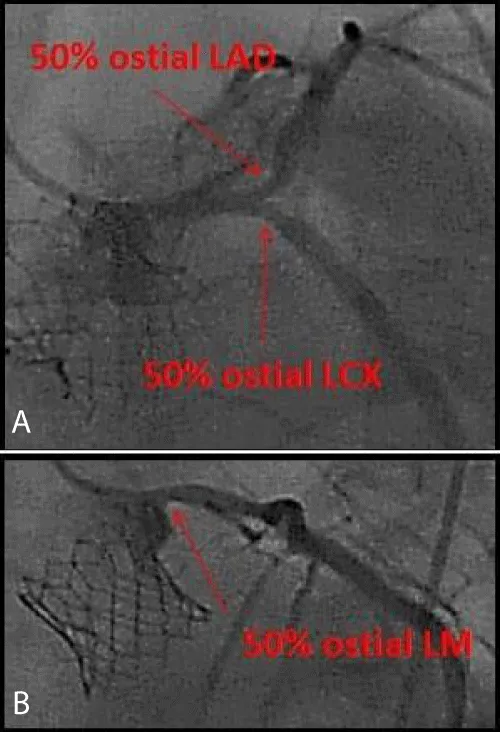
Unfortunately, the patient presented to our institution approximately 1 month later with a NSTEMI. LVEF by echocardiogram was now 30% - 35% (previously 50%). Repeat angiography revealed progression of ostial left main (LM) disease as well as progression of ostial LAD and ostial LCX disease. Instantaneous wave free-ratio (iFR) evaluation of the ostial LAD, ostial LCX, and ostial LM suggested that all three lesions were clinically significant (Figure 1).
Figure 1: Coronary angiogram, Post-TAVR NSTEMI Presentation. (A) LM-bifurcation lesion. (B) Ostial LM lesion.
Differential diagnosis
Considering prior PCIs, residual SYNTAX score was 22. He was initially medically managed in an effort to facilitate adequate recovery post-TAVR. Due to symptomatic, medication-refractory angina, our Heart Team recommended PCI of his ostial LM and LM bifurcation (Medina 1,1,1) with percutaneous left ventricular assist device (pVAD, Impella CP) support.
Investigations
Pre-TAVR CT data was used to select the femoral access most appropriate for Impella placement. The DK-Crush bifurcation PCI strategy was employed.
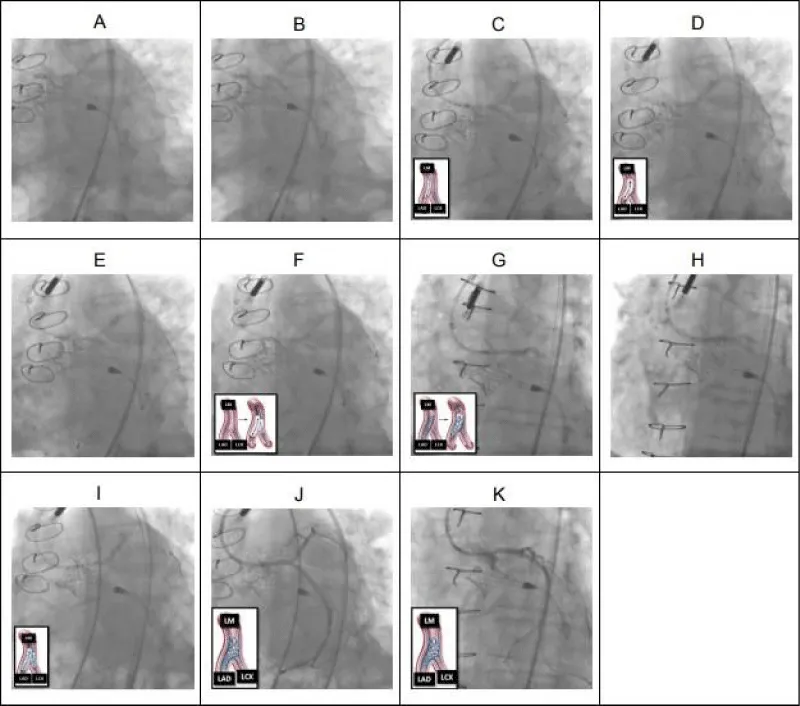
Details of this intervention are described here (Figure 2).
Figure 2: LM DK-Crush bifurcation PCI. (A) Pre-dilation (2.5 x 12 mm balloon) of ostial LAD. (B) Pre-dilation (2.5 x 12 mm balloon) of ostial LCX. (C) 3.0 x 12 mm drug-eluting stent (DES) deployed across LCX lesion with proximal portion of DES in the distal LM. (D) LCX wire removed and DES in LCX “crushed” with a 3.0 x 12 mm NC balloon extending from the LM to the LAD. (E) LCX rewired through “crushed” LCX stent and the struts of the “crushed” LCX stent were dilated with a 2.5 x 12 mm non-compliant balloon. (F) The first simultaneous kissing balloon inflation (SKBI) of the DK-Crush bifurcation PCI technique was performed using 3.0 x 12 mm and 2.5 x 12 mm non-compliant balloons in the LAD and LCX, respectively. The 3.0 x 12 mm non-compliant balloon was also used to pre-dilated the ostial LM (not shown). (G) Using IVUS-guidance, a 3.0 x 23 mm DES was positioned in multiple orthogonal views to span both the ostial LM and ostial LAD lesions before being deployed. The first proximal optimization technique (POT) was performed (not shown). (H) The proximal portion of the LM-LAD stent was flared with a 3.5 x 12 mm non-compliant balloon at high pressures. (I) After rewiring the LCX through the LM-LAD stent, 3.5 x 12 mm non-compliant balloons were positioned across both the LM-LAD and LM-LCX and the second SKBI was performed. A second POT was subsequently performed using the 3.5 x 12 mm non-compliant balloon (not shown). (J) Final result of the LM bifurcation (IVUS not shown but demonstrated excellent stent expansion and apposition without any evidence of edge dissection). (K) Final result of the ostial LM (IVUS not shown but demonstrated excellent stent expansion and apposition). (K) Final result of the ostial LM (IVUS not shown but demonstrated excellent stent expansion and apposition).
Management
Right and left femoral arterial access was obtained using the micropuncture technique with ultrasound and fluoroscopic guidance. A 7-French sheath was placed in the right femoral artery. Using the “pre-close” technique, two orthogonally positioned Perclose Proglide sutures were deployed at the left femoral access site. Heparin was administered and the activated clotting time was maintained > 250 for the entirety of the procedure. Using standard techniques, the Impella CP pVAD was appropriately positioned in the left ventricle and across the aortic valve. Pre-PCI intravascular ultrasound (IVUS) imaging had been performed at the time of the aforementioned iFR evaluation (where it was demonstrated that there was significant ostial LM, ostial LAD, and ostial LCX disease) and did not demonstrate significant calcium burden. As a result, the decision was made to not pursue adjunctive atherectomy.
Using a 7-French EBU 3.75 guide catheter via the right femoral arterial access, DK-Crush bifurcation PCI strategy was executed (Figure 2). Upon successful completion of the PCI, the guide catheter was removed. The Impella CP was weaned down and removed. The sutures at the “pre-closed” left femoral access site were secured and hemostasis was obtained. Hemostasis was achieved at the right femoral access site using an 8-French AngioSeal VIP. The patient was transferred in stable condition.
LM PCI post-TAVR is an uncommon occurrence but has been reported in the literature [1,2]. There are many strategies for addressing LM bifurcation lesions - research in this space is evolving. Based on a review of the current literature and Society of Cardiovascular Angiography and Interventions (SCAI) recommendations for complex left main bifurcation, the DK-Crush bifurcation strategy was chosen in our case [3-5]. LM PCI using a DK-Crush bifurcation strategy has never been described in a patient post-ViV TAVR. This complex, congested anatomy poses challenges in the execution of complex interventional coronary care, which can be mitigated with thorough case planning and preparation.
Secondly, Impella utilization post-TAVR has been described in case reports with no major complications noted [6]. However, a recent case describes the first presentation of cardiogenic shock post Evolut R TAVR complicated by Impella blade fracture from TAVR outlet strut interaction with Impella outlet, causing low flow [7]. Further data on Impella interaction with Evolut versus in our case, Edward Sapien valve is needed. Impella post-ViV TAVR has only been recently described, in the setting of bailout stenting coronary protection strategy immediately after TAVR [2]. The characteristics of the interaction between the Impella, the TAVR, and the SAVR is unknown; nonetheless, observer data would suggest that Impella use would be relatively low risk for ViV TAVR migration, embolization, or injury.
Follow up
Our patient did well immediately post-procedure and was discharged home the next day without short-term or long-term vascular complications. Post-procedure echocardiography demonstrated stable ViV TAVR without any evidence of leaflet trauma or dysfunction. He went on to have over 2 years free of angina and heart failure before passing away from recent metastatic malignancy.
Here, we describe the safe and successful execution of an Impella-assisted IVUS-guided LM bifurcation (Medina 1,1,1) PCI, facilitated by the DK-Crush strategy, in a patient recently post- ViV TAVR with unstable coronary artery disease and a reduced LVEF. We did not observe any adverse interaction between the Impella and the TAVR or the SAVR. There was no evidence of trauma, dysfunction, or injury of the leaflets of the TAVR. A Heart Team approach, careful planning, and thoughtful execution resulted in an excellent short- and long-term clinical result for this patient. This case thus highlights the potential role of Impella CP in complex PCI in a patient status post valve-in-valve TAVR, the role of DK-Crush bifurcation strategy for complex left main bifurcation in the setting of valve-in-valve TAVR, and the importance of the Heart Team approach.
Learning objectives
1. To recognize the potential role of Impella CP in complex PCI in a patient status post valve-in-valve TAVR.
2. To review the role of DK-Crush bifurcation strategy for complex left main bifurcation, in the setting of valve-in-valve TAVR.
3. To recognize the importance of careful strategy planning and execution of complex PCI, utilizing a Heart Team Approach.
Ethics statement
This case report conforms to the guidelines set forth in the “Recommendations for the Conduct, Reporting, Editing and Publication of Scholarly Work in Medical Journals”. Patient information has been de-identified.
This work was performed at Rush University Medical Center in Chi cago, IL.
- Chakravarty T, Sharma R, Abramowitz Y, Kapadia S, Latib A, et al. Outcomes in Patients with Transcatheter Aortic Valve Replacement and Left Main Stenting: The TAVR-LM Registry. J Am Coll Cardiol. 2016; 67: 951-960. PubMed: https://pubmed.ncbi.nlm.nih.gov/26916485/
- Dallan LAP, Young A, Bansal E, Gage A, Alaiti MA, et al. Predicted coronary occlusion and Impella salvage during valve-in-valve transcatheter aortic valve replacement. Cardiovasc Revasc Med. 2020; 21: 28-32. PubMed: https://pubmed.ncbi.nlm.nih.gov/30975579/
- Rab T, Sheiban I, Louvard Y, Sawaya FJ, Zhang JJ, et al. Current Interventions for the Left Main Bifurcation. JACC Cardiovasc Interv. 2017; 10: 849-865. PubMed: https://pubmed.ncbi.nlm.nih.gov/28473107/
- Sawaya FJ, Lefevre T, Chevalier B, Garot P, Hovasse T, et al. Contemporary Approach to Coronary Bifurcation Lesion Treatment. JACC Cardiovasc Interv. 2016; 9: 1861-1878. PubMed: https://pubmed.ncbi.nlm.nih.gov/27659563/
- Riley RF, Henry TD, Mahmud E, Kirtane AJ, Brilakis ES, et al. SCAI position statement on optimal percutaneous coronary interventional therapy for complex coronary artery disease. Catheter Cardiovasc Interv. 2020; 96: 346-362. PubMed: https://pubmed.ncbi.nlm.nih.gov/32406991
- Frisoli TM, Guerrero M, O'Neill WW. Mechanical circulatory support with impella to facilitate percutaneous coronary intervention for post-TAVI bilateral coronary obstruction. Catheter Cardiovasc Interv. 2016; 88: E34-37. PubMed: https://pubmed.ncbi.nlm.nih.gov/26104838/
- Sharma A, Bertog S, Mbai M. Impella Placement Across Transcatheter Aortic Valves: A Potential for Device-Device Interaction. JACC Cardiovasc Interv. 2020; 13: 2574-2575. PubMed: https://pubmed.ncbi.nlm.nih.gov/32861634/