More Information
Submitted: October 28, 2021 | Approved: January 31, 2022 | Published: February 01, 2022
How to cite this article: Wakjira H, Gobena T, Shore H. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected Hospitals in West Arsi Zone, Oromia Regional State, Ethiopia. J Cardiol Cardiovasc Med. 2022; 7: 006-012.
DOI: 10.29328/journal.jccm.1001124
Copyright License: © 2022 Wakjira H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Lifestyle modification; Hypertension; Practices; Ethiopia
Abbreviations: AOR: Adjusted Odd Ratio; BP: Blood Pressure; HELM: Hypertension Evaluation of Lifestyle and Management Scale; CVD: Cardiovascular Disease; DALY: Disability-Adjusted Life Years; DASH: Diet Allowance to Stop Hypertension; DBP: Diastolic Blood Pressure; ETB: Ethiopian Birr; FMO: Federal Ministry of Health; HELM: Hypertension Evaluation of Lifestyle and Management Scale; JNC7: 7the Joined National Committee; NCD: Noncommunicable Disease; SBP: Systolic Blood Pressure
Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected Hospitals in West Arsi Zone, Oromia Regional State, Ethiopia
Hika Wakjira1,2*, Tesfaye Gobena1 and Hirbo Shore1
1College Health and Medical Science, Haramaya University, Harar, Ethiopia
2Shala District Health Office West Arsi Zone, Oromia, Ethiopia
*Address for Correspondence: Hika Wakjira, College Health and Medical science, Haramaya University, Harar, Ethiopia, Email: [email protected]
Background: Globally 1.13 billion people were living with hypertension, Out of this two-thirds of them were living in low and middle-income countries. In Ethiopia, Non-Communicable Disease deaths are estimated at around 42%. However, it remains widely undetected and poorly controlled. To resolve these, lifestyle modification approaches that are often overlooked are the cornerstone of the prevention and management of hypertension.
Objective: To assess lifestyle modification practice and associated factors among hypertensive patients in selected hospitals in West Arsi Zone, Oromia Regional, Ethiopia December 7 to 21, 2019.
Method: Hospital-based cross-sectional study was conducted in the selected public hospital among 299 hypertensive patients. Systemic random sampling methods were used to select the study participants. Data were collected by face-to-face interviews using a structured questionnaire by trained data collectors. Data were analyzed using descriptive statistics and multivariate logistic regression method to identify predictors of the outcome (p < 0.05).
Results: Of the total participants, only 25.2% (95% CI: 18.8-32.9) of the patients were practiced recommended lifestyle modifications. Patients Age older than 65 years (AOR = 2.9, 95% CI: 1.17 - 7.0), the patients with 2-5 years’ time since diagnosed hypertension (AOR = 0.26, 95% CI: 0.07 - 0.9), multiple co-morbidity (AOR = 2.7, 95% CI: 1.25 - 5.8,) and their knowledge on hypertension management (AOR = 14.6, 95% CI: 4.6 - 45.9) have an independently associated with recommended lifestyle modification.
Conclusion: Lifestyle modification practices among hypertensive patients were low in this study. Age, comorbidity, time since diagnoses of hypertension, and knowledge of lifestyle were identified as predictors of the outcome.
Hypertension is defined as when increased blood pressure, the force of blood flowing through blood vessels is consistently too high. Which occurs when systolic blood pressure is greater than or equals to 140 mmHg or diastolic blood pressure greater than or equals to 90 mmHg. So, hypertension is when blood pressure is reading 140/90 mmHg [1]. High blood pressure, also known as hypertension, is a major contributor to the global disease burden and was responsible for 17.9 million deaths each year globally. However, it remains widely undetected, undertreated, and poorly controlled. Globally 1.13 billion people were living with hypertension, which means 1 in 4 men and 1 in 5 women had hypertension. Out of this two-thirds of them were living in low and middle-income countries [2].
The prevention and management of hypertension are major public health challenges [3]. For example, globally only fewer than 1 in 5 people with hypertension have the problem under control. This is due to the sharing of four major risk factors: tobacco use, unhealthy diets, harmful use of alcohol, and physical inactivity. To address this World Health Organization (WHO) developed an action plan to help translate these commitments into action. This global action plan for prevention and control of NCDs for 2013-2020 emphasizes addressing population-based risk factors and the integrated management of NCDs at the primary healthcare level which recommended lifestyle modification for hypertensive patients [4]. As a member state of the WHO, Ethiopia adopted the global strategy and developed the national NCD strategy for 10 years [5].
But fewer are known about magnitude health lifestyles since many of the studies were conducted on NCD especially Hypertension in Ethiopia where focuses on the pharmacological management of hypertension and its prevalence but not on non-pharmacological management (lifestyles modification). That means there are only a few studies done on the practice of lifestyles modification and associated factors of hypertension to show the gap and magnitude of the problem in this study area.
So these study that considers the practice of lifestyles modification and associated factors will guide actions to initiate the greater practice of good lifestyle modification among hypertensive patients by providing evidence to understanding the magnitude of the problem. So this study was to assess adherence to lifestyle modification practice and its associated factors among diagnosed hypertensive patients in the study area.
Study area and period
The study was conducted in the West Arsi zone on selected public hospitals. West Arsi Zone found in Oromia regional state, Ethiopia. It is located 251 km from Addis Ababa. The zone has 13 rural woredas and 2 administrative towns with a total population of 2,696,430 male 1330 488 and female 1365942. Moreover, divided into three main agro-climatically zones, highland, midland, and lowland, which comprise 45.5%, 39.6%, and 14.9% respectively [6]. Data will be collected from December 7 to 21, 2019.
Study design: A hospital-based cross-sectional study was conducted.
Source population: All hypertensive patients who were on follow up at public hospitals in West Arsi Zone.
Study population: Randomly Selected Control group of hypertensive patients who were attending follow up the unit and fulfilled the inclusion criteria’s and were available during the time of data collection.
Inclusion and exclusion criteria: All hypertensive patients who are 18 years and older, and on medical treatment (antihypertensive) at least for 1 months period before commencement of the study were recruited were included and patients with cognitive impairment and those less than 18 years old were immediately excluded from the study.
Sample size determination: The sample size was calculated using a single population proportion formula by assuming that 23% proportion of the patients practiced lifestyle modifications [7] with a 95% confidence interval and 5% margin of error. Therefore, 272 + (272 x 10%) non response rate =299 hypertensive patients was included in the study.
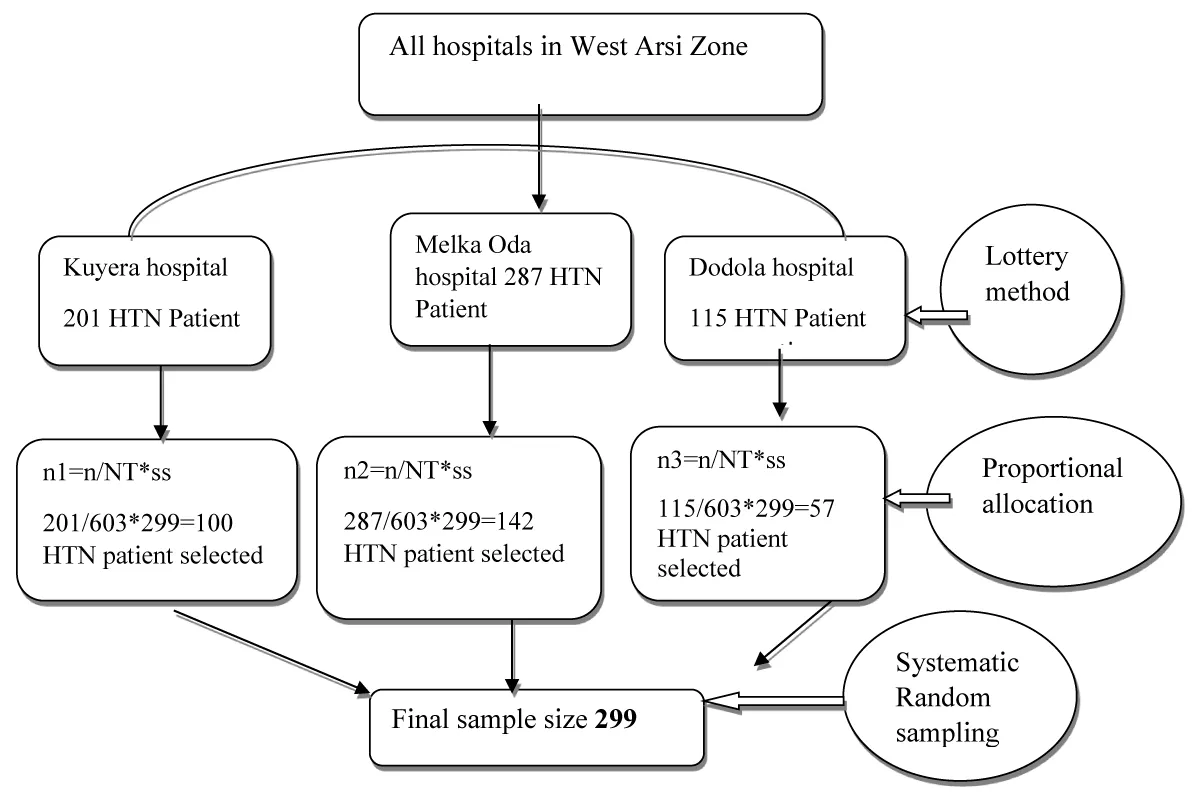
Sampling procedure: In the zone, there are 7 hospitals that offer chronic follow-up services. First, out of 7 public hospitals, three were selected by simple random sampling. Then, the sample size was allocated to three hospitals proportionally (based on the number of patients reporting per month). Study subjects were selected by using systematic random sampling method; every second hypertensive patient visiting the facilities at chronic follow-up departments who were known to be hypertensive (Figure 1).
Figure 1: Schematic presentation of sampling techniques used to select study subjects from public health hospitals in West Arsi Zone, 2019.
Variables
Dependent variable: The practice of lifestyles modifications.
Independent variables:
Socio-Economic variables: Age, sex, income, marital status, educational status, religion, occupation, ethnicity, residence.
Health profile of the patients: Time since diagnosis, presence of co-morbidity, family history of hypertension.
Individual factors: Knowledge of lifestyle modification practice.
Data collection method
Data were collected using a standardized pre-tested interviewer-administered questionnaire. Which was adapted from hypertension self-care practice questions recommended by the joint national committee (JNC 8) and WHO STEPS questionnaires [8]. The questionnaire was translated into Afan Oromo and back to English by language experts to ensure its consistency. The interview was conducted by eight BSc Nurse by using face-to-face interview method and two health officer supervisor was assigned to each hospital. The socio-demographic, health profiles of participants, Physical characteristics (height and weight) were measured. The weight and height of the patients were measured and BMI was calculated and classified using WHO guidelines as normal weight, overweight and obese. Weight and height measurements were taken during data collection. In addition, the patient medical record was reviewed to collect data of co-morbidity and time since diagnosis of hypertension.
Operational definition
Lifestyle modification is a practice which was recommended by JNC 8 as non-pharmacological managements of hypertension measured using physical exercise, low salt diet, and moderation of alcohol intake, stop smoking, and maintaining health weight.
Adherence to lifestyle modifications practice: Were Measured based on respondents who adhere to (DASH) diet they usually or always consumed a diet rich in vegetables, grains, and fruits; rarely or never consumed salt at least 3 times per week, aerobic exercise for > 30 minutes per day; at least three times per week, stop smoking, and Keep daily alcohol intake below 30 mL net Alcohol According to JNC 8 recommendations. In this study, the respondents who adhere to all these five healthy lifestyles were considered as adherent unless non-adherent.
Co-morbidity: Respondents with one or more other medical conditions in addition to hypertension.
Diet-related adherence: Who usually or always consu-med a diet rich in vegetables, fibers wholegrain, protein, and fruits; rarely or never consumed salt; at least 3 times per week.
Exercise-related adherence: Such as running, riding a bicycle, swimming, and other aerobic exercises for >30 minutes per day; at least five times per week.
Smoking-related adherence: Respondents who self-reported, they either never smoked or stopped smoking before 12 months.
Salt-related Adherence: The daily consumption of salt less than 5 g or 1 teaspoon or never.
Consume per food palate
Alcohol-related adherence: Either never consumed alcohol or Keep daily alcohol intake below 30 mL net Alcohol.
Body mass index: calculated from the weight and height (kg/m2) normal weight (18.5 ≤ BMI < 24), overweight (24 ≤ BMI < 28), an n d obese (BMI ≥ 28) [8].
Knowledge of healthy lifestyle: Respondents with a score above the mean value on hypertension evaluation of lifestyle and management (HELM) scale were taken as having good knowledge about lifestyle modification.
Data quality assurance
Both the data collectors and supervisors were trained for two days on the objective and methodology of the research, the data collection approach. The questionnaire was translated to Afaan Oromo language and back-translated into English by another person to check for consistency. A pretest was conducted in 15(5%) of the samples in a health care institution that was not included in the final study. The data collection instruments were assessed for completeness, consistency, and applicability and were ratified accordingly. Double data entry was done by two data clerks and consistency was checked. Finally, multivariate analysis was done to control all possible confounders. The study procedure was to protect the patient’s privacy by allowing anonymous and voluntary participation.
Data processing and analysis
Data were coded, checked, cleaned, and entered into Epidata version 3.1 software, then exported to SPSS version 24.0 software for analysis. Data were checked for incomplete and inconsistent before analysis. Bivariate analysis was used to check associations between independent and dependent variables to identify factors that were associated with the outcome variable. Those variables which were found to have an association (p < 0.25) with the outcome variable were entered into a multivariate logistic regression to test for independent association. The association between the different independent variables in relation to dependent was measured using odds ratios and 95% confidence interval (CI) and p values below 0.05 were considered to be statistically significant.
Ethical consideration
Ethical clearance was obtained from Institutional Health Research Ethics Review Committee (Ref. No. IHRERC/119/2020) of the College of Health and Medical Science Harar Campus and an official letter was sent to the selected public hospitals. After getting permission from the hospitals to participate in the study, informed, voluntary, written, and signed consent was obtained for the willingness of both heads of hospitals and patients to participate. The patients' privacy was maintained by conducting the interview in a private place and they will be informed that there won’t be any incentive or harm for their participation in this study. Finally, participants' identity was kept anonymous throughout the data collection and analysis process.
Socio-demographic characteristics of study participants
A total of 299 hypertensive patients were included in the study with a response rate of 98%. The mean age ± standard deviation of the participant was 55 ± 13.3 years. More than half, 172(57.4%) of the study participants were male, and 213(71.3%) were married. Over 1 in five respondents had no formal education. Over one in five (21.8%) and 58(23.8%).
Participants were government employees and merchants, respectively. Over three-quarters (76.2%). Were Oromo Ethnicity and 121(40.6%) were Muslims (Table 1).
| Table 1: Socio-demographic characteristics of participants West Arsi Zone, Ethiopia, 2019. | ||
| Variables | Frequency | Percent (%) |
| Female 127; Male 172 | ||
| Age in year | ||
| (18 - 40 ) Early adulthood | 50 | 17 |
| (41 - 64 ) Middle Adulthood | 132 | 44 |
| ( ≥ 65 ) Late Adulthood | 117 | 39 |
| Sex | ||
| Marital status Single | 8 | 3 |
| Divorce | 39 | 13 |
| Widowed | 39 | 13 |
| Married | 213 | 71 |
| Educational status | ||
| Secondary | 46 | 15 |
| Primary | 47 | 16 |
| Able to read and write | 56 | 17 |
| No formal education | 63 | 21 |
| College and above | 87 | 29 |
| Employment status | ||
| Daily laborer | 27 | 9.4 |
| Housewife | 36 | 12 |
| Retired | 42 | 14 |
| Private employee | 58 | 19 |
| Government employee | 65 | 22 |
| Merchant | 71 | 24 |
| Religion | ||
| Other(wakefata,jovh) | 10 | 3.5 |
| Catholic | 19 | 6.4 |
| Protestant | 52 | 17 |
| Muslim | 121 | 41 |
| Orthodox | 97 | 32.6 |
| Ethnicity | ||
| Wolayita and Others | 28 | 9.4 |
| Amhara | 43 | 15 |
| Oromo | 228 | 76 |
| Average monthly income | ||
| < 999 ETB | 7 | 2.5 |
| 1000-1999ETB | 40 | 13.4 |
| No regular income | 61 | 20 |
| 2000-2999ETB | 86 | 28.7 |
| > 3000ETB | 105 | 35.1 |
Clinical characteristics of study participants
From participants, the majority 144(48%) of them were less than 2 years since when they are diagnosed as hypertensive patients, and 62(20.8%) patients were diagnosed before 6 years on treatments.
Of the total, 158(53%) patients were overweight whereas 30(9.9%) were Obese. Over Two-third (62.3%) of respondents had co-morbidity especially Diabetic Mellitus and 117(39.1%) has a family history of hypertension (Table 2).
| Table 2: Health profiles of respondents among hypertensive patients attending chronic follow up units of selected hospitals in West Arsi zone, Ethiopia, 2019. | |||
| Variables | Categories | Frequency | Percent (%) |
| Time since diagnosis | less than 2 years | 144 | 4 |
| 2 - 5 years | 93 | 318 | |
| Body mass index (kg/m2) | greater than 6 yNoearrsmal (18 - 24) | 62 111 |
.220 .837 |
| |
Overweight (24 - 28) Obe se (≥ 28) |
158 30 |
.15 93 |
| Multiple Comorbidities | present | 186 | 62. |
| Absent | 113 | 38.3 | |
| Family history of hypertension | Yes No |
117 182 |
39 60.1 |
Adherence to recommended lifestyle modification practices among hypertensive patients
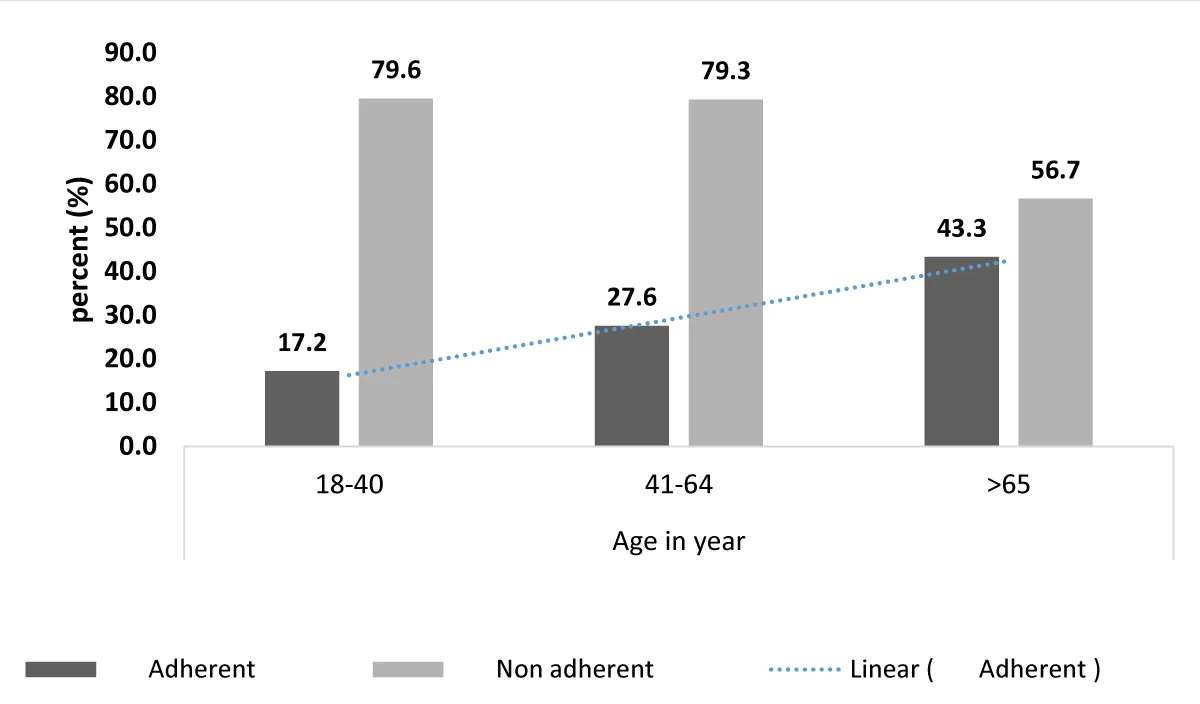
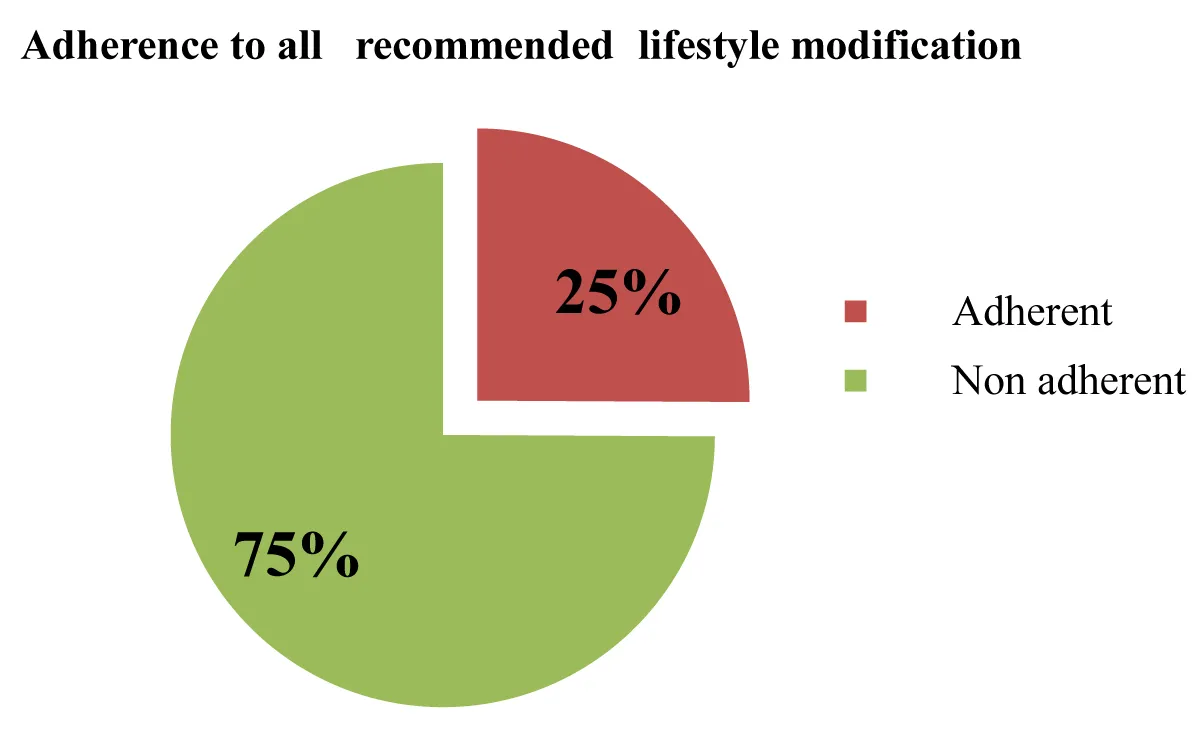
According to the finding of these studies, 25.2% (95% CI: 18.8 - 32.9) of patients practice all recommended lifestyle modifications. As age increased the adherence to healthy lifestyles were also increase (Figures 2,3). Of the total participants, 63.4% do not engage in regular physical exercise for at least 3 days of the week with a minimum of 30 min duration. One hundred forty-five (48.5%) of study subjects adhered to the limitation of alcohol intake and more than half (52.5%) of the practices recommended a low salt diet. Additionally, the majority of participants were not ever smoking 225(75.2%) and 10% of hypertensive patients were smoke cigarettes. Nearly half, 142(47.5%) of study participants were practicing recommended health weight management. Only 45% of the respondent has knowledge’s of recommended lifestyle modification practices (Table 3).
Figure 2: Adherence to healthy lifestyle by age group among hypertensive patients attending chronic follow up units of selected hospitals in West Arsi zone, Ethiopia, 2019.
Figure 3: Adherence to healthy lifestyle among hypertensive patients attending chronic follow up units of selected hospitals in West Arsi zone, Ethiopia, 2019.
| Table 3: Adherence to recommended lifestyle modifications practice among hypertensive patients attending chronic follow up units of selected hospitals in West Arsi zone, Ethiopia, 2019. | ||
| Variables | Frequency | Percent (%) |
| Maintain a healthy weight | ||
| Good | 142 | 47 |
| Bad | 157 | 33 |
| Limit alcohol intake | ||
| Yes (daily net alcohol intake below 30 mL ) | 145 | 48 |
| No (daily net alcohol intake Above 30 mL) Perform recommended physical exercise (30 min/day) |
154 | 52 |
| Yes | 109 | 37 |
| No | 190 | 63 |
| Status of tobacco use | ||
| Ever not used | 225 | 75 |
| Still smoking | 30 | 10 |
| Stopped smoking Practice recommended low salt diet | 44 | 15 |
| Yes (about ≤ 1 tsp/day of table salt). | 157 | 52.5 |
| No (greater than 1 tsp/day of table salt). Adherence to all recommended healthy lifestyle |
142 | 47.5 |
| Adherent | 75 | 25 |
| Non adherent | 224 | 75 |
| Knowledgeable about healthy lifestyle | ||
| poor | 135 | 45 |
| good | 164 | 55 |
Factors associated with adherence to lifestyle modifications practices
The results of the bivariate analysis show that age, Co-morbidity, time since diagnosis of Hypertension, those who have formal education and knowledge of lifestyle modification became significant association with dependent Variables.
After controlling possible confounding effects of other covariates, age, time since diagnosis, co-morbidity, and knowledge about the disease were significantly affecting the adherence to healthy lifestyle modification among hypertensive patients. Patients older than 65 years were 3 times more likely to be adherent to recommended healthy lifestyle modification practices than patients younger than 64 years old (AOR = 2.9, 95% CI: 1.17 - 7.0). Those respondents who had good knowledge were 15 times more likely to be adherent (AOR = 14.6, 95% CI: 4.6 - 45.9) compared to the non- knowledgeable respondents. Additionally, the patients with 2-5 years since times of diagnosis were 74% times less likely to practice healthy lifestyle modification (AOR = 0.26, 95% CI: 0.07-0.9) as compared to those on treatment for greater than 6 years of treatment. Also, patients who were with Co-morbidity were 2.7 more likely to practice healthy lifestyle modification (AOR = 2.7, 95% CI: 1.25 - 5.8) as compared to those without comorbidity (Table 4).
| Table 4: Predictors of lifestyle modification practices among hypertensive patients attending chronic follow up units of selected hospitals in West Arsi zone, Ethiopia, 2019. | ||||
| Variables | Healthy Lifestyle adherence | |||
| Adherent N (%) | Non-adherent N (%) | COR(95% CI) | AOR(95% CI) | |
| Age in year | ||||
| 18 - 40 | 22(29.4) | 34(15.2) | 1 | |
| 41 - 64 | 19(25.5) | 92(41.1) | 0.59(0.4 - 3.6) | 1.4(0.4 - 4.6) |
| ≥65 | 34(45.1) | 98(43.7) | 1.6(1.01 - 4.97)* | 2.9(1.17-7.0)* |
| Sex | ||||
| Male | 35(47) | 90(40.3) | 1 | |
| Female | 40(53) | 134(59.6) | 0.764(0.70 -2.48) | 1.13(0.5 - 2.3) |
| Marital status | ||||
| Married | 59(78.4) | 154(68.8) | 1 | |
| Divorce | 10(13.7) | 34(15.2) | 0.76(0.40 - 2.67) | 0.9(0.36 - 2.6) |
| Widowed | 6(8) | 36(15.9) | 2.1(0.68 - 6.5) | 1.9(0.6 - 6.5) |
| Educational status | ||||
| No formal education | 6(7.8) | 56(25.1) | 1 | |
| Formal education | 69(92.1) | 168(74.8) | 3.8(1.15 - 9.57)* | 1.7(0.5 - 5.6) |
| Average monthly income | ||||
| no regular income | 10(13.7) | 50(22.5) | 1 | |
| 1000-1999ETB | 6(8) | 42(18.5) | 0.40(0.16 - 1.1) | 1(0.26 - 4.4) |
| 2000-2999ETB | 28(37.2) | 58(25.8) | 0.35(0.21 - 0.58) | 0.4(0.15 - 1.2) |
| > 3000ETB | 31(41) | 74(33) | 1.18(0.3 - 4.5) | 0.48(0.17 - 1.3) |
| Knowledgeable about healthy lifestyle | ||||
| Poor | 16(21.5) | 148(66.2) | 1 | |
| Good | 59(78.4) | 76(33.7) | 7.1(3.4 - 15.07)* | 14.6(4.6 - 45.9)** |
| Time since diagnosis | ||||
| less than 2 years | 44(58.8) | 99(44.3) | 1 | |
| 2 - 5 years | 19(25.5) | 74(33.1) | 0.57(0.074 - 0.85)* | 0.26(0.07 - 0.9)* |
| greater than 6 years | 12(15.6) | 50(22.5) | 0.86(0.272 - 2.76) | 0.4(0.1 - 1.45) |
| Multiple Comorbidities | ||||
| Absent | 25(31.6) | 126(58.6) | 1 | |
| Present | 54(68.3) | 89(41.3) | 3.05(1.771 - 5.28)* | 2.7(1.25 - 5.8)** |
| *AOR = Statistically Significant at p < 0.05, **AOR = Statistically Significant at p < 0.001. | ||||
Even though healthy lifestyle modification is one of the important hypertension management, poor adherence to a healthy lifestyle is one of the reasons for serious complications and uncontrolled Hypertension in addition to wastage of health care resources. So, Control of hypertension requires both pharmacological and non-pharmacological treatments. Since adherence to a healthy lifestyle and medication is the ultimate strategies to control hypertension, this study was aimed to assess lifestyle modification practices and associated factors among diagnosed hypertensive patients.
According to the Main intention results of these studies, only 75(25.2%) participants were practicing the recommended lifestyle modification. Nearly comparable results 27.3% Adherence were revealed according to a study conducted in Ethiopia in Durame and Nigist Elleni memorial hospital [9]. In contrast, the study conducted in the USA shows that 50% of participants were engaged in healthy lifestyle practices [6]. This might be due to the different educational backgrounds of patients and the level of awareness about lifestyle modification and its advantages. It also might be due to patients relying only on medication without considering the effects of healthy lifestyle modification on hypertension control.
Of the participants, three fourth of them were non-smokers, and half of them have abstained from any type of alcohol drinking or less than 30 mL net alcohol daily consumption. This is supported by study findings which are done in Malaysia and Ghanaian on hypertensive patients [10,11]. This could be due to social and cultural practices that discourage alcohol drinking and smoking.
In this study, less than half of the participants were adherent to Performing recommended physical exercise for 30 minutes per day. But similar studies results from India and Thailand found (53%) and (40%) respectively [12,13]. The possible explanation could be related to low awareness, socio-economic variation, and lack of organized set up in living areas in developing countries like Ethiopia.
Among lifestyle modification, two fourth of the participants practiced a limited salt diet ( ≤ 1 tsp/day of table salt) and nearly half of them were practicing maintaining a healthy weight using recommended diets (DASH) including more fruits, vegetables, grains, and beans in the diet and reading nutritional facts on food labels. A similar study finding from Saudi Arabia shows that the 79.3% of patients practice a low salt diet and 59.9% practice maintaining’s of a healthy weight [14]. The discrepancy between these studies and the study from Saudi Arabia could be due to the economic class, the difference in dietary habits, and easy access to recommended diets.
Older age respondents were found to be more adherent to a healthy lifestyle than younger age groups. The study from the kingdom of Sued Arabia supports this finding, in that age > 65 years old is more likely in practicing recommended lifestyle modification [15]. This could be due to older persons having more education and cognitive function and having more comorbidities which may make them visit health care providers more frequently. Another explanation might be younger patients were less likely eager to control their blood pressure by practicing lifestyle modification.
On the other hand, Knowledge is also significantly associated with adherence to healthy lifestyle modification. Knowledgeable hypertensive patients about healthy lifestyles were more adherent to recommended healthy lifestyle modifications. This is supported by the finding from the study in Ethiopia at the cardiac clinic of Ayder comprehensive specialized hospital and the USA, Maryland [6,16]. The explanation might be as knowledge status increases practice and motivation of lifestyle modification practice will also increase. It may be due to access to information sources like fosters, leaflets, and similar written material about hypertension management and controls.
A study conducted in Addis Ababa found that people with comorbidities were more likely to be adherent to healthy lifestyle recommendations [6,7]. Surprisingly the finding of these studies also depicts respondents having one or more comorbidity were found more likely to be adherent to all the healthy lifestyle recommendations. Patients with comorbidities visit health care providers more frequently and pay more attention to their health conditions, as this was evidenced by better adherence to lifestyle modifications.
Hypertensive Patients with greater than 6 years’ times since diagnoses were more likely to practice healthy lifestyle modification as compared to those on treatment for less 2 years treatment. This Finding is supported by different studies that show patients on longer duration of treatment had good lifestyle modification practice [9,17]. This might be due to continued counseling’ and health education.
The limitation is that the study didn’t include hypertensive patients who were attending follow-up in private health facilities in the study area. Also, research methodologies involving self-reported measures depend largely on individuals‟ memory, and recall bias may exist.
This study revealed lifestyle modification practice is low among hypertensive patients. Of the studied variables, age, duration of the hypertension diagnosis, knowledge about lifestyle, and comorbidity were factors significantly associated with healthy lifestyle modification practice. Out of these factors duration of the hypertension diagnosis (time since diagnosis) was negatively associated with lifestyle modification and the rest’s age, knowledge about healthy lifestyle, and comorbidity were positively associated with lifestyle modification.
Declaration
Author’s contributions: HW, TG, and HS made a substantial contribution to the conception design, acquisition, and interpretation of data. HW drafted the manuscript and carried out rigorous editorial work. All authors revised the paper critically for the intellectual contents. All authors read and approved the final manuscript.
Author’s information: HW1,2 Shala District health office West Arsi Zone, Oromia, Ethiopia. TG1, HS1 College Health, and Medical Science, Haramaya University, Harar, Ethiopia.
First of all, I am very grateful to God. Next, I would like to thank both my advisors Associate Professor Tesfaye Gobena and Mr. Hirbo Shore (MPH) for their unreserved guidance and constructive suggestions and comments, at each step of the research development. Next, I would like to thank the participants of this thesis for their cooperation and Hara may University for giving me this chance.
- American Heart Association. Guideline for the Prevention, detection, evaluation and management of high Blood Pressure in adults. 2017.
- WHO. Clinical guidelines for the management of hypertension. 2005.
- Joint TS. prevention, detection, evaluation, and treatment of high blood pressur. National Institutes of Health, U.S. Department of Health and Human Services. 2014.
- World Health Organization. A global brief on hypertension. 2013.
- FMOH. National strategic action plan for the prevention and control of NCDs in Ethiopia 2014 - 2016. 2014.
- Abu H, Aboumatar H, Carson K, Goldberg R, Cooper LA. Hypertension knowledge, heart healthy lifestyle practices and medication adherence among adults with hypertension. Eur J Pers Cent Healthc. 2018; 6: 108-114. PubMed: https://pubmed.ncbi.nlm.nih.gov/32405420/
- Mengistu D, Tibebu A. Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefere Adherence. 2017; 11: 323-330. PubMed: https://pubmed.ncbi.nlm.nih.gov/28280305/
- WHO. WHO STEP wise Approach to Chronic Disease Risk-Factor Surveillance. 2016.
- Siyum E, Kelbiso L, Olana R. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clin Hypertens. 2017; 23: 26. PubMed: https://pubmed.ncbi.nlm.nih.gov/29214054/
- Afia FAM, Owusu-Daaku FT, Addo MO, Saana II. Ghanaian hypertensive patients understanding of their medicines and life style modification for managing hypertension. Int J Pharm Pharmaceut Sci. 2014; 6: 165-170.
- Tahmina, Habib N, Kailash K, Rashid M. Lifestyle modification practice in rural community at Kedah in Malaysia. J Basic, Clin Appl Health Sci. 2018; 1: 19-26.
- Lipilekha P, Kalyan K, Sumitra P, Trilochan S. Lifestyle Pattern and Hypertension Related Knowledge, Attitude and Practices among Diagnosed Patients of Hypertension Attending a Tertiary Care Hospital. J Cardiovasc Dis Res. 2017; 8: 108-111.
- Zahid HM, Most L, Satya P, Marif. Knowledge, attitude and practice of life style modification in the management of hypertension. Obese Eat Disorder.2017; 3: 21.
- Lama A, Alshimaa A, Maradi A, Rana M. Awareness and Knowledge on Hypertension and its Self-Care Practices Among Hypertensive Patients in Saudi Arabia. Ann Int Med Dent Res. 2017; 3: 58-63.
- Abubaker E. Level of Adherence to Lifestyle Changes And Medications Among Male Hypertensive Patients In Two Hospitals In Taif; Kingdom Of Saudi Arabia. Int J Pharm Pharmaceut Sci. 2015; 7: 168-172.
- Yirga L, Seid I, Kassa TD, Asgedom SW. Practice and predictors of self-care behaviors among ambulatory patients with hypertension in Ethiopia. PLoS ONE. 2019; 14: 1-16. PubMed: https://pubmed.ncbi.nlm.nih.gov/31242265/
- Durai V, Rani MA. Knowledge and Practice on lifestyle modifications among males with hypertension. Indian J Commun Health. 2015 27: 143-149.