More Information
Submitted: January 19, 2022 | Approved: March 09, 2022 | Published: March 10, 2022
How to cite this article: Jani Y, Haxhirexha K, Haxhirexha F, Pocesta B, Rexhepi A, et al. Control of arterial hypertension and risk of new-onset of atrial fibrillation in patients with metabolic syndrome. J Cardiol Cardiovasc Med. 2022; 7: 017-022.
DOI: 10.29328/journal.jccm.1001126
Copyright License: © 2022 Jani Y, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Controlled blood pressure; Metabolic syndrome and atrial fibrillation
Abbreviations: MS: Metabolic Syndrome; BW: Bodyweight; BH: Body Height; BMI: Body Mass Index; BP: Blood Pressure; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; T2DM: Diabetes Mellitus Type 2; WCi: Waist Circumference; LDL.Chol.: Serum Low-Density Lipoprotein Cholesterol; HDL-C: Serum High-Density Lipoproteins Cholesterol; TG: Serum Triglycerides; AF: Atrial Fibrillation; LVEF: LV Ejection Fraction; LAVI: Left Atrial Volume Index; ESC: European Society of Cardiology; ASE: American Society of Echocardiography
Control of arterial hypertension and risk of new-onset of atrial fibrillation in patients with metabolic syndrome
Ylber Jani1*, Kastriot Haxhirexha1, Ferizat Haxhirexha1, Bekim Pocesta2, Atila Rexhepi1, Fatmir Ferati1, Ahmet Kamberi3, Agim Zeqiri4, Sotiraq Xhunga5, Artur Serani5 and Lutfi Zylbeari1
1Faculty of Medicine, Tetovo, Republic of North Macedonia
2Department of Cardiology, Faculty of Medicine, Ss. Cyril and Methodius University of Skopje, Republic of North Macedonia
3Department of Cardiology, Faculty of Medicine, M. Teresa Tirana, Republic of Albania
4Department of Internal Medicine, General Hospital “DR Ferit Murat” Gostivar, Republic of North Macedonia
5Department of Cardiology, Medical Center Dures, Republic of Albania
*Address for Correspondence: Ylber Jani, MD, PhD, Faculty of Medicine, Tetovo, Republic of North Macedonia, Email: [email protected]
Background: An association between Atrial Fibrillation (AF) and Metabolic Syndrome (MS) a constellation of abnormalities (high blood pressure, hyperglycemia, dyslipidemia, and abdominal obesity), has been demonstrated. There have been many studies that have shown that elevated blood pressure (BP), was significantly associated with an increased risk of AF. It is uncertain whether maintaining the optimal BP levels can prevent AF in the patients with MS categorized as ‘high-risk’ patients.
Objective: The aim of this study was to evaluate the influence of control of BP on the occurrence of new-onset atrial fibrillation in patients with Metabolic Syndrome.
Methods: Into this observational study, was enrolled 435 consecutive patients (210 males and 225 females) aged 45-79 years who fulfilled criteria for MS. Participants were selected among primary and secondary care patients, who were receiving ongoing care for arterial hypertension in the period from November 2018 till November 2021. The study was conducted at outpatients in 5 Health Care Clinics (3 Secondary Health Care Clinics and 2 Primary Health Clinics). Patient were categorized according to their BP levels as Group 1-patients with controlled BP, {(patients aged < 65 years Systolic Blood Pressure (SBP) of 120 - 130 mmHg, patients aged ≥ 65 years SBP of 130 - 139 mmHg)} and Diastolic Blood Pressure (DBP), {(patients aged < 65 years of < 80 mmHg. but not < 70 mmHg; patients aged ≥ 65 years of 85 - 89 mmHg)}, or Group 2-patients with uncontrolled BP(> 130/80 mmHg),and in patients aged ≥ 65 years BP (≥ 140/90 mmHg ).
Results: New-onset of AF, was more frequent in participants with uncontrolled BP, respectively (34.7% vs. 19.5%, p = 0.009).Patients with uncontrolled BP have more frequent persistent AF (15.2% vs. 0.04%) and permanent AF (0.08% vs. 0.02%), whereas there was not significant changes between groups in relation to frequency of paroxysmal AF, respectively (12.8% vs. 10.9%, p = 0.29). There was observed significant association of uncontrolled BP with: increased frequency of AF (OR = 2.193; 95% CI 1.390 - 3.439), persistent AF (OR = 3.931; 95% CI 1.771 - 8.084), permanent AF (OR = 4.138; 95% CI 1.383-12.381), LA. Dimension ≥ 2.2 cm/m2 (OR = 2.089, 95% CI 1.330 - 3.252), BMI (OR = 5.226, 95% CI 3.155 - 8.659) and 5-risk factors for MS, respectively (OR = 2.998, 95% CI 1.833 - 4.901).
Conclusion: Optimal BP levels, can reduce the frequency of new-onset AF in patients with MS categorized as ‘high-risk’ patients. Uncontrolled BP was associated with an increased risk of both subtypes of AF (persistent and permanent) in the patients with MS categorized as ‘high-risk’ patients.
Atrial fibrillation (AF), the most common arrhythmia, is a medical problem of increasing prevalence often associated with multiple comorbidities and adverse outcomes [1]. An association between AF and Metabolic Syndrome (MS) a constellation of abnormalities (high blood pressure, hyperglycemia, dyslipidemia, and abdominal obesity), has been demonstrated [2-4]. AF appears to be more closely related to a specific component of MS compared with others [5]. There have been many studies that have shown that elevated BP was significantly associated with an increased risk of AF [6]. According to new findings [7], strong evidence of a causal relationship between blood pressure (BP) and AF has been found. High BP can directly lead to AF, establishing that elevated BP causes AF, provides further impetus for public health strategies aimed at improving BP control [7]. It is not clear whether the risk of AF increases linearly with BP or whether there is a BP threshold above which the risk of this condition definitely increases [8], also it is uncertain whether maintaining the optimal BP levels can prevent AF in the patients with MS [9,10] categorized as ‘high-risk’ patients. We sought to test the hypothesis that: optimal BP levels can reduce the frequency of new-onset AF in the patients with MS categorized as ‘high-risk’ patients.
Objective
The aim of this study was to evaluate the influence of control of blood pressure on the occurrence of new-onset atrial fibrillation in patients with Metabolic Syndrome.
Into this observational study, was enrolled 435 consecutive patients (210 males and 225 females) aged 45-79 years who fulfilled the criteria for MS [11]. Participants were selected among primary and secondary care patients, who were receiving ongoing care for arterial hypertension in the period from November 2018 till November 2021. The study was conducted at outpatients in 5 Health Care Clinics (3 Secondary Health Care Clinics and 2 Primary Health Clinics).
Subjects with: AF and other cardiac arrhythmias at baseline, secondary hypertension, those on hemodialysis, congenital and acquired valvular heart disease, left/right bundle branch block, pre-excitation syndrome, patients with a pacemaker, patients treated with drugs that prolong QT- interval, were excluded.
All the patients underwent medical history, clinical and anthropometric evaluation, the survey obtained data on age, gender, and calculated body mass index (BMI) as weight (kg) divided by the square of the height (m2). Weight was measured with weight balance scales and height with a stadiometer. Waist circumference (WCi) was reported in cm. All participants in the study were subjected to a resting external electrocardiogram (ECG with Lab. version 3.0). Routine laboratory tests from blood samples the value of glycemia, creatinine, electrolyte (Na+, K+, Ca+), lipid status: total cholesterol (TC), LDL-cholesterol, HDL-cholesterol, Triglycerides (TG), in the morning post 12-hour fasting period were determined.
Metabolic Syndrome, was defined according to the harmonized definition of the International Diabetes Federation and other organizations [12]. On the basis of the baseline examination, the metabolic syndrome was diagnosed when at least 3 of the following criteria were met.
(1) Central adiposity {Waist circumference (WC)} > 102 cm in men and > 88 cm in women);
(2) Serum HDL-C < 50 mg/dL in women or < 40 mg/dL in men;
(3) Serum triglyceride levels > 150 mg/dL;
(4) Arterial hypertension or use of antihypertensive drugs;
(5) The presence of diabetes mellitus (DM) or use of anti-diabetic drugs [13].
Office BP measurements, Measuring of blood pressure according to standard protocol [14]. Clinic systolic (SBP) and diastolic (DBP), were recorded by a physician using a mercury sphygmomanometer and appropriate-sized cuffs. The BP was determined with the individual sitting for at least 5 min. The individuals had not smoked or taken any coffee, tea, or alcohol for at least 3 h, nor had they undertaken any physical exercise for half an hour before the BP measurements were taken. Measurements were performed in triplicate, 2 min apart, and the mean value was used as the BP for the visit. The mean SBP and mean (DBP) recorded during the study period were calculated. According to guidelines of ESC/ESH [14], SBP was target to (120 - 130 mmHg) and in older patients (aged ≥ 65 years aged) to target 130 – 139 mmHg), to target the DBP (< 80 mm Hg. but not < 70 mmHg).
Patients were categorized according to their BP levels as Group 1-patients with controlled BP (SBP of 120-130 mmHg, patients aged ≥ 65 years SBP of 130 - 139 mmHg and DBP of < 80 mmHg. but not < 70 mmHg; aged ≥ 65 years of 85 – 89 mmHg), or Group 2-patients with uncontrolled BP (>130/80 mmHg).and in patients aged ≥ 65 years BP (≥ 140/90 mmHg).
Echocardiography
Left atrial (LA) and left ventricular (LV) measurements and calculation of LV mass were made according to standardized methods [15]. LA diameter (cm) was indexed by body surface area (m2), and LA enlargement was defined as LA diameter/body surface area ≥ 2.2 cm/m2 [16]. LV ejection fraction was calculated using the Teichholz formula or the Simpson rule and defined as low when it was < 50% [15]. LV mass was indexed by height and LV hypertrophy was defined as LV mass/height > 50 g/m in men and > 47 g/m in women [17].
Follow-up
Subjects were followed-up in outpatient clinics. The occurrence of the event, that is AF, was recorded during follow-up visits. Data were collected by the authors of this study. Those reviewing the endpoint were blinded to other patients’ data. In this report, we evaluated the occurrence of new-onset AF, either paroxysmal, persistent, or permanent, in patients with baseline sinus rhythm. AF was documented by ECG performed at follow-up visits or the time of hospitalization. Each ECG was evaluated by two independent cardiologists. The incidence date of AF was defined as the date of the first ECG showing AF.
The study was conducted in agreement with the Declaration of Helsinki. Informed written consent was given by all participants before they were enrolled in the study.
Statistical analysis
A statistical software program ((SPSS 19.0), was applied for the statistical analysis. Results are expressed as mean and ± SD, or as a percentage. A simple descriptive analysis was performed for the general characterization of the sample and distribution of variables. The distribution of variables was tested for normality using the Kolmogorov-Smirnov test, and the heterogeneity of variances was evaluated by Levene’s test. To compare baseline characteristics and findings between groups, we used Student,s unpaired t - test for continuous data, Mann-Whitney U - test for continuous data with abnormal distribution, and X2 - test for categorical data. The association between variables was analyzed using logistic regression. Odds Ratio (OR) and 95% confidence interval (CI) were estimated by logistic regression. A p - value < 0.05 was considered statistically significant for a confidence interval of 95%.
According to control of Blood Pressure, in patients with MS, there were no significant changes in relation to baseline characteristics. Data are presented in Table 1. Echocardiographic data of cardiac structure and function according to control of BP, are presented in Table 1A. There were no significant changes between groups in relation to left ventricular dimensions and ejection fraction, however, in relation to LVMI, there was a significant difference. Participants who had uncontrolled BP had higher LVMI than participants with controlled BP, respectively (53.6 ± 12.1 vs. 49.1 ± 7.4, p = 0.03). Also participants with uncontrolled BP, have increased LA Dimension (LA ≥ 2.2 cm/m2): (36% vs. 20% p = 0.006).
| Table 1: Baseline characteristics of patients with MS (n.435), according to control of Blood Pressure. | ||||||||
| Variables | MS (N.435) | p - value | ||||||
| Gr. with controlled B.P. (n- 179) | Gr. with uncontrolled B.P. (n. 256) | |||||||
| N. (%) | Mean | ± SD | N. (%) | Mean | ± SD | |||
| Gender. | Females | 79(42.2) | 146(57.8) | 0.1 | ||||
| Males | 100(57.8) | 240(42.2) | 0.1 | |||||
| Age (year) | 62.6 | ± 6.9 | 63.3 | ± 5.0 | 0.9 | |||
| Age (year) | > 65 | 99(55.3) | 157(61.0) | 0.5 | ||||
| < 65 | 80(44.6) | 99(38.6) | 0.4 | |||||
| BMI (kg/m2) | 26.6 | ± 3.7 | 26.85 | ± 4.6 | 0.6 | |||
| SBP (mmHg) | 128.1 | ± 6.2 | 155.4 | ± 7.3 | 0.000 | |||
| DBP (mmHg) | 81 | ± 4 | 98.7 | ± 2.9 | 0.000 | |||
| T2DM (presence) | 148(79.1) | 215(83.9) | 0.9 | |||||
| WCi (presence) | 140(78.2) | 205(88) | 0.8 | |||||
| HDL-chl (presence) | 136(75.9) | 189(73.8) | 0.7 | |||||
| TG (presence) | 125(69.8) | 185 (72.2) | 0.8 | |||||
| No. of measures BP. | 16.3 | ± 1 | 16.8 | ± 2 | 0.6 | |||
| Three MS risk factor | 75(41.8) | 80(31.2) | 0.1 | |||||
| Four MS risk factor | 65(36.3) | 132(51.5) | 0.05 | |||||
| Five MS risk factor | 40(22.3) | 45(17.5) | 0.3 | |||||
| SPB: Systolic Blood Pressure; DPB; Diastolic Blood Pressure; T2D: Diebetes Mellitus; WCi; Weist Circumference; HDL-Chol; High-Density Cholesterol; TG: Triglicerides; No BP: Number of Measures Blood Pressure during the followed period; MS risk factors: Number of a risk factor for Metabolic Syndrome; Three, Four, Five (risk factors for MS). | ||||||||
| Table 1A: Echocardiographic data of cardiac structure and function according to control of Blood Pressure. | |||
| Variables | Gr. with controlled B.P. (n-179) | Gr. with uncontrolled B.P. (n.256) | p - value |
| LA. Dimension (cm). | 2.1 ± 1.7 | 2.3 ± 3.0 | 0.7 |
| LA ≥ 2.2 cm/m2; (n;%) | 36(20) | 93(36) | 0.006 |
| LVEF,% | 65 ± 0.5 | 67 ± 0.8 | 0.4 |
| LVFS,% | 37 ± 2.3 | 38 ± 0.4 | 0.7 |
| EDD(cm) | 4.83 ± 0.4 | 4.86 ± 0.3 | 0.7 |
| ESD(cm) | 2.8 ± 0.3 | 2.9 ± 0.6 | 0.6 |
| THS(cm) | 1.2 ± 2.5 | 1.3 ± 2.7 | 0.05 |
| THPW(cm) | 1.1 ± 0.5 | 1.1 ± 0.2 | 0.9 |
| LVMI(g/m2) | 49.1 ± 7.4 | 53.6 ± 12.1 | 0.03 |
| LA: Dimension; LA ≥ 2.2 cm/m2 Dimension/m2; LVEF%: Left Ventricular Ejection Fraction; LVFS: Left Ventricular Fraction of Shortening; EDD: End Diastolic Dimension of Left Ventriculi; ESD: End Systolic Dimension of Left Ventriculi; THS: Thickening of the Septum; TPW: Thickening of the Posterior Wall; LVMI: Left Ventricular Mas/Index. | |||
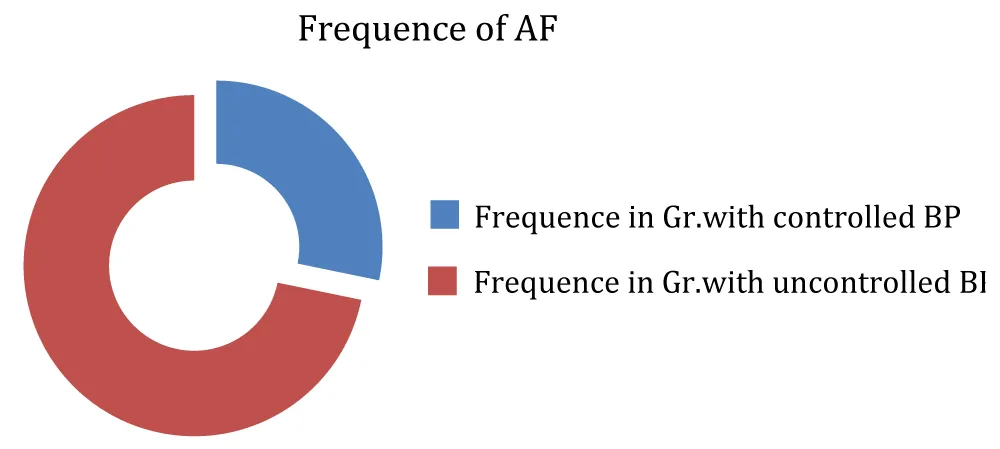
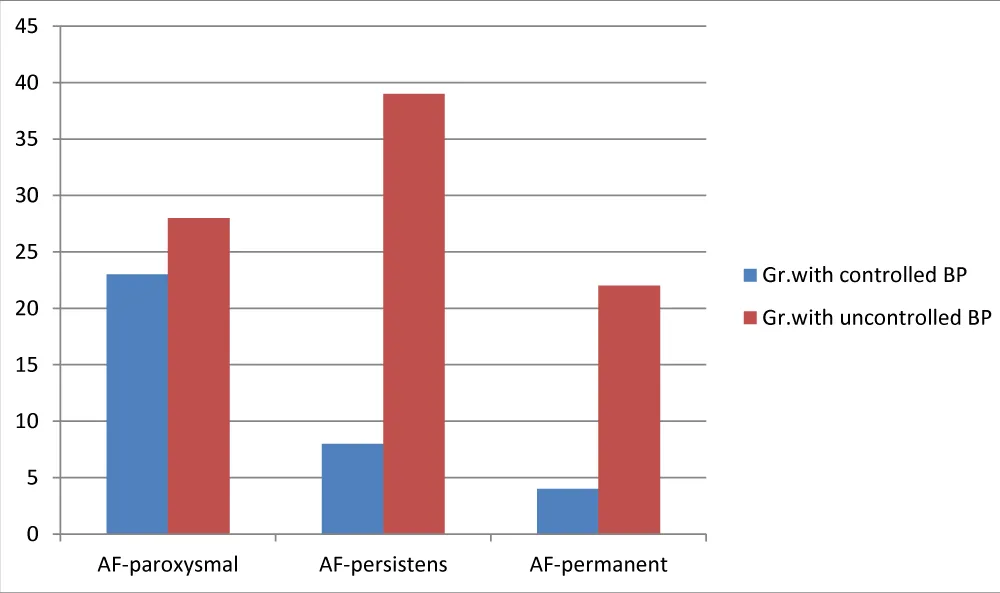
New-onset of AF, was more frequent in participans with uncontrolled BP, respectively (34.7% vs. 19.5%, p = 0.009). Patients with uncontrolled BP have more frequent persistent AF(15.2% vs. 0.04%) and permanent AF (0.08% vs. 0.02%), whereas there was not significant changes between groups in relation to frequency of paroxysmal AF, respectively {(12.8% vs. 10.9%, p = 0.29), (Table 2, Figures 1,2)}.
| Table 2: Frequency and type of Atrial Fibrillation according to control of Blood Pressure. | |||
| Study Groups. (N.435)` | p | ||
| Variables | Gr. with controlled B.P. (N. 179) | Gr. with uncontrolled B.P. (N. 256) | |
| AF(No; %) | 35(19.5) | 89(34.7) | 0.009 |
| AF-paroxysmal (No; %) | 23(12.8) | 28(10,9) | 0.29 |
| AF-persistens (No; %) | 8(0.04) | 39(15.2) | 0.001 |
| AF-permanent (No; %) | 4(51,4) | 22(30,9) | 0.009 |
| AF: Atrial Fibrillation; BP: Blood Pressure. | |||
Figure 1: Frequency of Atrial Fibrillation according to control of Blood Pressure.
Figure 2: Frequence of type of Atrial Fibrillation according to control of Blood Pressure.
Association of uncontrolled blood pressure with: Frequency of AF, Type of AF (persistens and permanent), assotiation of AF with features of cardiac structures (LA. Diemnsion, ≥ 2.2 cm/m2); BMI, number of risk factors for Metabolic Syndrome, are presented in Table 3. There was observed significant association of uncon-trolled BP with: increased frequency of AF (OR = 2.193; 95% CI 1.390 - 3.439), persistent AF (OR = 3.931; 95% CI 1.771 - 8.084), permanent AF (OR = 4.138; 95% CI 1.383 - 12.381), LA. Diemnsion ≥ 2.2 cm/m2 (OR = 2.089, 95% CI 1.330 - 3.252), BMI (OR =5.226, 95% CI 3.155 - 8.659) and 5-risk factors for MS, respectively (OR = 2.998, 95% CI 1.833 - 4.901).
| Table 3: Logistic Regression Model. Association of uncontrolled blood pressure with Frequency of AF, Type of AF (paroxysmal, persistent, and permanent). Association of AF with features of cardiac structures (LA. Dimension, ≥ 2.2 cm/m2). | ||||
| characteristics: uncontrolled BP |
OR | Significance | 95% CI for Exp (B) | |
| Lower | Upper | |||
| Frequence of AF | 2.193 | .000 | 1.390 | 3.439 |
| Persistent AF | 3.931 | .000 | 1.771 | 8.094 |
| Permanent AF | 4.138 | .000 | 1.383 | 12.381 |
| LA.Dimension | 2.089 | .000 | 1.330 | 3.252 |
| N.5-MS.RF | 2.998 | .000 | 1.833 | 4.901 |
| BMI | 5.226 | .000 | 3.155 | 8.659 |
In the present study, we demonstrated that the participants with MS and uncontrolled BP, have a 34,7% increase in the frequency of new-onset of AF. Frequence that is significantly higher than among participants with MS and controlled BP. Results that confirmed our hypothesis and highlight the importance of optimal BP control to prevent AF in participants with MS categorized as ‘high-risk’ patients.
The link between blood pressure and atrial fibrillation in a patient with MS is not simply, furthermore AF appears to be more closely related to specific components of MS compared with others, however, elevated blood pressure was the most important contributor [18]. Recently, Georgios Georgiopoulos and co-authors [19], found that elevated blood pressure was associated with a heightened risk of AF. When a patient’s systolic blood pressure rises just 1 mmHG, for instance, it was associated with a 1.8% relative increase of developing AF. The same increase in a patient’s diastolic blood pressure is associated with a 2.6% relative increase. In our study, the results indicated that the participants with MS and uncontrolled BP, have a 34.7% increased rate of incident AF. It was consistent with the previous study demonstrating the relationship between arterial hypertension and incidence of AF [18]. However, in the present study, we had a much shorter follow-up time (a median of 4 years) and participants were with MS, while the previous surveyes [18-20], had a much longer follow-up time, and participants were without MS.
Previous studies demonstrate an epidemiological association between hypertension and increased risk of AF, however, it is not clear whether the risk of AF increases linearly with BP or whether there is a BP threshold above which the risk of this condition definitely increases [21,22]. Thus, the majority of clinical studies showed a direct and linear relation between BP levels and the risk of AF. Moreover, our aim was different, resulting in different patient classifications. Also, it is uncertain whether Standart (SBP < 140 mmHg) or intensive control of BP (SBP < 120 mmHg), reduces the risk of subsequent AF in hypertensive patients with MS, categorized as ‘high-risk’ patients. Thus, the most effective BP target in these patients is unknown. In the previous study by Verdecchia, and co-authors [9], demonstrate that the risk of new-onset AF was reduced in the intensive BP (SBP < 120 mmHg) lowering group, compared to the standard BP (SBP < 140 mmHg) lowering group with hypertension and diabetes [23]. Chen, and co-authors demonstrated that the intensive therapy group (target SBP < 120 mm Hg) did not show statistical significance with respect to the incidence of AF in patients with hypertension and diabetes [24]. Yet the current BP guidelines, including the recently released US guidelines [14,25], did not recommend more aggressive blood pressure targets for AF prevention. Based on epidemiological evidence, this suggestion might sound quite reasonable.
Previous studies have shown that hypertension promotes the progression from paroxysmal AF to more sustained forms of the disease [26]. Our study adds to this by showing the risk of developing different subtypes of AF in a population without AF at baseline. In our study, we found that the frequency of persistent and permanent subtypes of AF was significantly increased in participants with uncontrolled BP. Longitudinal studies examining the association between blood pressure and AF subtypes are sparse [27,28].
Several pathophysiologic mechanisms could explain the relationship between HT and AF. Chronic exposure of the heart to elevated blood pressure leads to mechanical and electrical changes in LA anatomy and function that, over time, promote AF through a variety of electrophysiological mechanisms, some of which are unclear [29]. In the present study, we found a significant association of increased dimension of LA, LVMI, and: frequency of AF and subtype of AF (persistent and permanent AF), in participants with uncontrolled BP. Similar results have been found by other authors [30-32]. A recent study by Larsson SC and co-authors reported that Arterial Hypertension and AF share the same pathogenic factors. Higher BMI and a particularly fat mass index were associated with an increased risk of both HT and AF [33]. In our study, we found a significant association between increased BMI and increased frequency of AF in a patient with uncontrolled BP.
Future directions: Arterial Hypertension is the most common modifiable risk factor for atrial fibrillation, this indicates that optimal BP control, could be an effective strategy to stop AF and its complications.
Limitations
There are several limitations to our study. First, the cross-sectional design precludes the assessment of causal relationships between control of BP and AF. In spite of this, based on the epidemiology data and Mendelian randomization causality research, we believe the causality to HT and AF.
Second, the ascertainment of AF is not perfect, It is identified by ECGs performed during the examination, so the true prevalence of AF is probably higher than that indicated by the present study because prolonged electrocardiographic monitoring may detect clinically silent AF in a variable proportion of subjects who present in sinus rhythm, it may miss the paroxysmal AF, resulting in a lower AF incidence in the present study.
Third, the partial ability of clinic BP to detect real BP status/control unlike ambulatory BP might be helpful in order to find the best strategy to prevent AF in a patient with MS and uncontrolled BP.
We proved the hypothesis that optimal BP levels can reduce the frequency of new-onset AF in the patients with MS categorized as ‘high-risk’ patients. Uncontrolled BP was associated with an increased risk of both subtypes of AF (persistent and permanent) in the patients with MS categorized as ‘high-risk’ patients. These findings should clinicians encourage and prioritize blood pressure control in patients at high risk for new-onset atrial fibrillation as an effective strategy to reduce this common arrhythmia.
Declarations
Consent to participate: All patients were written informed, consent was obtained from all participating patients before they were enrolled in the study.
A local ethics committee ruled that no formal ethics approval was required in this particular case.
Authorship contributions
Concept: Ylber Jani, Design–Bekim Pocesta; Supervision: Atila Rexhepi; Materials: Fatmir Ferati, Agim Zeqiri; Kastriot Haxhirexha; Data collection/processing: Ylber Jani, Sotiraq Xhunga, Artur Serani, Ferizat Haxhirexha; Analysis/interpretation: Ylber Jani, Atila Rexhepi, Ahmet Kamberi; Literature Search: Fatmir Ferati, Ylber Jani, Artur Serani; Critical Reviews: Ahmet Kamberi, Atila Rexhepi, Lutfi Izeiri.
All authors read and approved the final manuscript.
We thank Ahmet Kamberi Ph.D., Atila Rexhepi Ph.D., Fatmir Ferati Ph.D., Agim Zeqiri MD, Ferizat Haxhirexha Ph.D., Kastriot Haxhirexha Ph.D., Sotiraq Xhunga MD, Artur Xhunga MD, Lutfi Izeiri Ph.D., for their contributions to this study.
Conflict of interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- Lane DA, Skjoth F, Lip GYH, Larsen TB, Kotecha D. Temporal trends in incidence, prevalence, and mortality of atrial fibrillation in primary care. J Am Heart Assoc. 2017; 6: 116. e005155. PubMed: https://pubmed.ncbi.nlm.nih.gov/28455344/
- Ford ES. Prevalence of Metabolic Syndrome defined by the international Diabetes Federation among adult in the US. Diabetes Care. 2005; 28: 2745-2749. PubMed: https://pubmed.ncbi.nlm.nih.gov/16249550/
- Tanner RM, Baber U, Carson AP, Voeks J, Brown TM, et al. Association of the metabolic syndrome with atrial fibrillation among United States adults (from the REasons for Geographic and Racial Differences in Stroke [REGARDS] Study). Am J Cardiol. 2011; 108: 227–232. PubMed: https://pubmed.ncbi.nlm.nih.gov/21530935/
- Karantzopoulos P, Kokoris S, Papaionnides D. The association of metabolic syndrome with atrial fibrillation:an emerging epidemiological and patophysiologica hypothesis. Cardiology. 2005; 104: 148-149. PubMed: https://pubmed.ncbi.nlm.nih.gov/16118494/
- Arthur RM, Carl JL, James DN, James OK, Daniel PM, et al. Cardiometabolic Risk Factors and Atrial Fibrillation. Rev Cardiovasc Med. 2013; 14: 73-81. PubMed: https://pubmed.ncbi.nlm.nih.gov/24448257/
- Manolis AJ, Rosel FA, Coca A. Hypertension and Atrial Fibrillation:diagnostic approach,prevention and treatment.Position paper of the Working Group “Hypertension Arrhythmias and Thombosis” of the European Society of Hypertension. J Hypertens. 2012; 30: 239-252.
- Georgiopoulos G, Ntritsos G, Stamatelopoulos K, Tsioufis C, Aimo A, et al. The relationship between blood pressure and risk of atrial fibrillation: a Mendelian randomization study. Eur J Prev Cardiol. 2021; zwab005. PubMed: https://pubmed.ncbi.nlm.nih.gov/33556963/
- Paolo V, Fabio A, Gianpaolo R. Hypertension and Atrial Fibrillation: Doubts and Certainties From Basic and Clinical Studies. Circ Res. 2018; 122: 352-368. PubMed: https://pubmed.ncbi.nlm.nih.gov/29348255/
- Verdecchia P, Staessen JA, Angeli F, de Simone G, Achilli A, et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): An open-label randomised trial. Lancet. 2009; 374: 525–533. PubMed: https://pubmed.ncbi.nlm.nih.gov/19683638/
- Chen LY, Bigger JT, Hickey KT, Chen H, Lopez-Jimenez C, et al. Effect of Intensive Blood Pressure Lowering on Incident Atrial Fibrillation and P-Wave Indices in the ACCORD Blood Pressure Trial. Am J Hypertens. 2016; 29: 1276–1282. PubMed: https://pubmed.ncbi.nlm.nih.gov/26476086/
- Ford ES, Li C, Zhao G. Prevelence and correlates of Metabolic Synrome based on a harmonious definition among adults in the US. J Diabetes. 2010; 2: 180-1993. PubMed: https://pubmed.ncbi.nlm.nih.gov/20923483/
- Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for he Study of Obesity. Circulation. 2009; 120: 1640–1645. PubMed: https://pubmed.ncbi.nlm.nih.gov/19805654/
- American Diabetes Association. Standarts for Medical Care for Patients with Diabetes Mellitus. Diabetes Care. 2002; 25: 213-229. PubMed: https://pubmed.ncbi.nlm.nih.gov/12502618/
- Williams B, Mancia G, Spiering W, Agabiti E, Azii M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018; 39: 3021–3104. PubMed: https://pubmed.ncbi.nlm.nih.gov/30165516/
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2015; 16: 233–271. PubMed: https://pubmed.ncbi.nlm.nih.gov/25559473/
- Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016; 29: 277–314. PubMed: https://pubmed.ncbi.nlm.nih.gov/27037982/
- de Simone G, Daniel RS, Devereux RB, Meyer RA, Roman MJ, et al. Left ventricular mass and body size in normotensive children and adults:assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992; 20: 1251-1260. PubMed: https://pubmed.ncbi.nlm.nih.gov/1401629/
- Huxley RR, Lopez FL, Folsom AR, Agarwal SK, Loehr LR, et al. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011; 123: 1501–1508. PubMed: https://pubmed.ncbi.nlm.nih.gov/21444879/
- Georgiopoulos G, Ntritsos G, Stamatelopoulos K, Tsioufis C, Aimo A, et al. The relationship between blood pressure and risk of atrial fibrillation: a Mendelian randomization study. Eur J Prev Cardiol. 2021. PubMed: https://pubmed.ncbi.nlm.nih.gov/33556963/
- Verdecchia PF. Angeli P, Reboldi G. Hypertension and Atrial Fibrillation. Circulat Res. 2018; 122: 352–368. PubMed: https://pubmed.ncbi.nlm.nih.gov/29348255/
- Alves-Cabratosa L, García-Gil M, Comas-Cufí M, Ponjoan A, Martí R, et al. Incident atrial fibrillation hazard in hypertensive population: a risk function from and for clinical practice. Hypertension. 2015; 65: 1180-1186. PubMed: https://pubmed.ncbi.nlm.nih.gov/25847950/
- Verdecchia P, Mazzotta G, Angeli F, Reboldi G. Above which blood pressure level does the risk of atrial fibrillation increase? Hypertension. 2012; 59:184–185. PubMed: https://pubmed.ncbi.nlm.nih.gov/22252400/
- Soliman EZ, Rahman AF, Zhang Z, Rodriguez CJ, Chang TI, et al. Effect of Intensive Blood Pressure Lowering on the Risk of Atrial Fibrillation. Hypertension. 2020; 75: 1491–1496. PubMed: https://pubmed.ncbi.nlm.nih.gov/32362229/
- Chen LY, Bigger JT, Hickey KT, Chen H, Lopez-Jimenez C, et al. Effect of Intensive Blood Pressure Lowering on the Risk of Atrial Fibrillation and P-Wave Indices in the ACCORD Blood Pressure Trial. Am J Hypertens. 2016; 29: 1276–1282. PubMed: https://pubmed.ncbi.nlm.nih.gov/26476086/
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/ NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018; 138: e484–e594. PubMed: https://pubmed.ncbi.nlm.nih.gov/29133354/
- de Vos CB, Pisters R, Nieuwlaat R, Prins MH, Tieleman RG, et al. Progression From Paroxysmal to Persistent Atrial Fibrillation. J Am Coll Cardiol. 2010; 55: 725–731. PubMed: https://pubmed.ncbi.nlm.nih.gov/20170808/
- Thomas MC, Dublin S, Kaplan RC, Glazer NL, Lumley T, et al. Blood Pressure Control and Risk of Incident Atrial Fibrillation. Am J Hypertens. 2008; 21: 1111–1116. PubMed: https://pubmed.ncbi.nlm.nih.gov/18756257/
- Sandhu RK, Conen D, Tedrow UB, Fitzgerald KC, Pradhan AD, et al. Predisposing Factors Associated With Development of Persistent Compared with Paroxysmal Atrial Fibrillation. J Am Heart Assoc. 2014; 3: e000916. PubMed: https://pubmed.ncbi.nlm.nih.gov/24786144/
- Healey JS, Connolly SJ. Atrial fibrillation: hypertension as a causative agent, risk factor for complications, and potential therapeutic target. Am J Cardiol. 2003; 91: 9G-14G. PubMed: https://pubmed.ncbi.nlm.nih.gov/12781903/
- Vaziri SM, Larson MG, Lauer MS, Benjamin EJ, Levy D. Influence of blood pressure on left atrial size. The Framingham Heart study.Hypertension. 1995; 25: 1155–1160. PubMed: https://pubmed.ncbi.nlm.nih.gov/7768556/
- Okin PM, Gerdts E, Wachtell K, Oikarinen L, Nieminen MS, et al. Relationship of left atrial enlargement to persistence or development of ECG left ventricular hypertrophy in hypertensive patients: implications for the development of new atrial fibrillation. J Hypertens. 2010; 28: 1534–1540. PubMed: https://pubmed.ncbi.nlm.nih.gov/20589977/
- Francesca C, Anna M, Pierdomenico U, Matteo De R, Andrea De L, et al. Ambulatory blood pressure and risk of new-onset atrial fibrillation in treated hypertensive patients. J Clin Hypertens (Greenwich). 2021; 23: 147-152. PubMed: https://pubmed.ncbi.nlm.nih.gov/33242233/
- Larsson SC, Back M, Rees J, Mason AM, Burgess S. Body mass index and body composition in relation to 14 cardiovascular conditions in UK Biobank: a Mendelian randomization study. Eur Heart J. 2020; 41: 221–226. PubMed: https://pubmed.ncbi.nlm.nih.gov/31195408/