More Information
Submitted: March 17, 2022 | Approved: May 04, 2022 | Published: May 05, 2022
How to cite this article: Le HP, Nguyen BG. Associations of arterial stiffness with left ventricular mass index and carotid intima-media thickness in the hypertensives. J Cardiol Cardiovasc Med. 2022; 7: 040-045.
DOI: 10.29328/journal.jccm.1001131
Copyright License: © 2022 Le HP, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Arterial stiffness; Pulse wave velocity; Ankle-brachial index; Left ventricular mass index; Carotid intima-media thickness
Associations of arterial stiffness with left ventricular mass index and carotid intima-media thickness in the hypertensives
Hoang P Le1* and Binh G Nguyen2
1Department of Internal Medicine, University of Medicine and Pharmacy, Hue University, Thua Thien Hue 491-20, Vietnam
2Department of Cardiology, University of Medicine and Pharmacy Hospital, Thua Thien Hue 491-20, Vietnam
*Address for Correspondence: Hoang P Le, Department of Internal Medicine, University of Medicine and Pharmacy, Hue University, Thua Thien Hue 491-20, Vietnam, Email: [email protected]
Background: Arterial stiffness has been considered an independent predictor of cardiovascular disease in addition to the traditionally known cardiovascular risk factors.
Objectives: This study aimed to investigate the associations between arterial stiffness with left ventricular mass index and carotid intima-media thickness in the hypertensives.
Methods: A descriptive cross-sectional study compared a control group in 210 study subjects (105 hypertensives and 105 normotensives). Measuring left ventricular mass index by echocardiography and carotid intima-media thickness by carotid doppler ultrasonography. Pulse wave velocity was measured using the Agedio B900 device and the Agedio K520 application. The manual method was measured by the ankle-brachial index.
Results: There was a statistically significant positive correlation between pulse wave velocity and age (r = 0.922, p < 0.001). The ankle-brachial index had a statistically significant positive correlation at a weak level with left ventricular mass index and carotid intima-media thickness, in which the coefficient r was equal to 0.219 (p < 0.05) and 0.250 (p < 0,001), respectively. Pulse wave velocity also had a statistically significant positive correlation at a weak level with left ventricular mass index and carotid intima-media thickness, in which the coefficient r was equal to 0.188 (p < 0.05) and 0.289 (p < 0,001), respectively. Pulse wave velocity had a multivariable linear correlation with gender, pulse, mean blood pressure, and ankle-brachial index with statistical significance; and they were written in the form of the following equation: Pulse wave velocity (R2: 41.3%) = 0.641*(Gender) – 0.027*(Pulse) + 0.043*(Mean blood pressure) + 8.378*(Ankle-brachial index) – 3.254.
Conclusion: Arterial stiffness was statistically correlated with left ventricular mass index and carotid intima-media thickness in the hypertensives. Through the above research results, we suggest that the hypertensives should be combined with the evaluation of hemodynamic parameters and arterial stiffness for contributing to the diagnosis and detection of cardiovascular complications, thereby improving the quality of monitoring and treatment in hypertensive patients.
Hypertension is the most common cardiovascular disease, known as the silent killer. Hypertension is increasing worldwide. According to the results of May Measure Month by the International Society of Hypertension in 2019 conducted on 1,508,130 people ≥ 18 years old, the global rate of hypertension was 34%; however, only 58.7% of patients were aware. On the other hand, up to 32% of the subjects had never had their blood pressure checked before [1]. As reported by the National Health and Nutrition Examination Survey from 2011 to 2014, although 84.1% of patients were aware and 76% of patients were being treated, only 54% of patients-controlled blood pressure < 140/90 mmHg [2]. According to the World Health Organization in 2014, the prevalence of hypertension in people over 18 years old was highest in Africa with nearly 30% and lowest in America with 18%; some other regions were as follows: Eastern Mediterranean (27%), Europe (23%), East and South Asia (24%), and Western Pacific (19%) [3].
Hypertension is one of the risk factors leading to plaque formation and progression to heart failure, coronary heart disease, stroke, etc [4]. Currently, cardiovascular associations worldwide have still recommended treatment goals for hypertension based on peripheral blood pressure because of its simplicity and ease of application in clinical practice [5,6]. Alternatively, arterial stiffness has been recently considered an independent predictor of cardiovascular disease in addition to the traditionally known cardiovascular risk factors [7-9].
We conducted the study to investigate the associations between arterial stiffness with the left ventricular mass index (LVMI) and carotid intima-media thickness (CIMT) in the hypertensives.
Study design
A cross-sectional descriptive study comparing the control group was conducted between July 2018 and July 2020 at Hue University of Medicine and Pharmacy Hospital, located in the Thua Thien Hue province, Vietnam.
Sample size and sampling
The consecutively convenient sampling technique was used to recruit patients from the Cardiovascular department. Data of 210 patients aged 40 years or above (including 105 hypertensives and 105 normotensives) were collected.
Data collection procedure
The doctors who were utilized as interviewers were trained in data collection by a senior researcher. A four-hour training session took place on the hospital campus. A weekly meeting was conducted in order to improve the quality of the data collected.
Patients visiting the Department of Internal Medicine, Hue University of Medicine, and Pharmacy Hospital were recruited for this study. The people selected were those who were aged 18 and above, did not have any emergency conditions or any mental health problems, and were able to listen and understand the local language or dialect. Patients who met the above criteria were divided into two groups: hypertensives and normotensives. Normotensive is defined as systolic blood pressure < 140 mmHg, diastolic blood pressure < 90 mmHg, or not on antihypertensive medication. Hypertensive is defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or antihypertensive medication [5]. Informed consent was achieved from all participants before taking the survey. After obtaining the consent form from each participant, a face-to-face interview and examination were conducted by the well-trained doctors using printed questionnaires.
Measurements
Personal characteristics: The following variables were also assessed: age, some risk factors for cardiovascular diseases such as smoking, diabetes, dyslipidemia, obesity, values of pulse, blood pressure parameters, lipid profile, and blood glucose level.
Left Ventricular Mass Index (LVMI): Using Philips Affiniti 70 Echocardiogram to perform M mode ultrasound to measure the following parameters: Left Ventricular End Diastolic Dimension (LVEDd), Left ventricular posterior wall diastolic (LVPWd), Interventricular Septal Diastolic (IVSd), from which LVMI was calculated according to the following formula:
LVMI (g/m2) = LVM (g) / BSA (m2)
where: LVM (g) = 0,8 x {1,04 x [(LVEDd + LVPWd + IVSd)3 – (LVEDd)3]} + 0,6;
BSA is the body surface area, calculated using patient’s weight and height;
LVMI > 95 g/m2 (female) or > 115 g/m2 (male) is defined as abnormal [10].
Carotid Intima-Media Thickness (CIMT): We determined the presence of atherosclerotic plaque by showing minimal plaque on both transverse and axial planes. The criteria for diagnosing atherosclerotic plaque are focal thickening of the arterial wall at least 50% of the medial intima – surrounding intima or focal thickening of the medial – medial coat more than 1.5 mm convex into the vascular side.
CIMT > 0.9 mm or atherosclerotic plaque is defined as abnormal [11].
Pulse Wave Velocity (PWV): We used the Agedio B900 device, version 1.3 (Germany), and the Agedio K520 application to analyze the results obtained from the Agedio B900 device via Bluetooth connection. Regulations for patients before and during measurement were similar to brachial blood pressure measurement.
Step 1: Open the Agedio K520 application and enter patient information.
Step 2: Wear the cuff that fits the patient’s wrist.
Step 3: Start the Agedio B900 and follow the measurement instructions.
Step 4: Finish and read the result.
High PWV is defined as more than or equal to 10 m/s [6].
Ankle–Brachial Index (ABI): The manual ABI was performed by measuring the systolic blood pressure from brachial and ankle arteries. An ABI was calculated for each leg. The ABI value was determined by taking the higher pressure of the two arteries at the ankle, divided by the higher of the two brachial arterial systolic pressure. The higher ABI of the two-leg would be chosen for this research. ABI higher than 1.4 is defined as arterial stiffness [12].
Ethical approval
This study was approved by the Ethical Review Committee of Hue University of Medicine and Pharmacy, Vietnam (IRB no. H2018/374). All participants were asked for their permission and signed consent forms before their participation.
Statistical analysis
Data were analyzed using the SPSS Version 20.0. The significance level was set at a p - value < 0.05. Using the Chi-square test on independence to find out the relationship between qualitative variables, the Chi-square test on homogeneity to compare two ratios. Using independent t-test, Mann-Whitney U test to compare two mean values. We checked the correlation between quantitative variables using Spearman correlation coefficients. The correlation coefficient r has a value from -1 to +1. Multivariable linear regression model: y = a + β1*x1 + β2*x2 +…+ βi*xi + e.
Patients’ characteristics
There were statistically significant age differences; the percentage of risk factors such as smoking, diabetes; ABI; PWV; LVMI, and CIMT between the two groups normotensives and hypertensives. Mean values of pulse, blood pressure, lipid profile, and blood glucose level of the two groups were also described in Table 1.
| Table 1: Characteristics of patients (N = 210). | |||
| Variables | Normotensives (N = 105) | Hypertensives (N = 105) | p - value |
| Age* | 65.07 ± 12.80 | 70.49 ± 11.31 | < 0.05 |
| Smoking (in %) | 21.9 | 46.7 | < 0.05 |
| Diabetes (in %) | 5.7 | 24.8 | < 0.05 |
| Dyslipidemia (in %) | 48.9 | 51.1 | > 0.05 |
| Obesity (in %) | 14.3 | 17.1 | > 0.05 |
| Pulse (beat/min)* | 70.35 ± 9.17 | 75.67 ± 11.36 | - |
| Systolic blood pressure (mmHg)* | 116.90 ± 7.55 | 153.51 ± 12.51 | - |
| Diastolic blood pressure (mmHg)* | 74.51 ± 3.35 | 96.13 ± 7.82 | - |
| Mean blood pressure (mmHg)* | 88.64 ± 3.79 | 115.28 ± 8.01 | - |
| Total Cholesterol (mmol/L)** | 5.04 (4.53 – 5.82) | 4.99 (3.98 – 5.75) | > 0.05 |
| Triglyceride (mmol/L)** | 1.56 (1.08 – 2.61) | 1.76 (1.17 – 2.28) | > 0.05 |
| HDL-Cholesterol (mmol/L)** | 1.21 (1.00 – 1.41) | 1.16 (1.01 – 1.45) | > 0.05 |
| LDL-Cholesterol (mmol/L)** | 3.46 (2.91 – 4.31) | 3.46 (2.28 – 3.89) | > 0.05 |
| Blood Glucose (mmol/L)** | 5.65 (5.22 – 7.23) | 6.39 (5.34 – 8.15) | > 0.05 |
| ABI* | 1.16 ± 0.10 | 1.24 ± 0.15 | < 0.001 |
| PWV (m/s) | 9.21 ± 1.99 | 11.12 ± 2.14 | < 0.001 |
| LVMI (g/m2) | 93.19 ± 21.96 | 119.15 ± 22.82 | < 0.001 |
| CIMT (mm) | 0.94 ± 0.24 | 1.09 ± 0.26 | < 0.001 |
| Note: * Mean ± SD, ** Median (P25 – P75). Abbreviation: ABI: Ankle-Brachial Index; PWV: Pulse Wave Velocity; LVMI: Left Ventricular Mass Index; CIMT: Carotid Intima-Media Thickness. |
|||
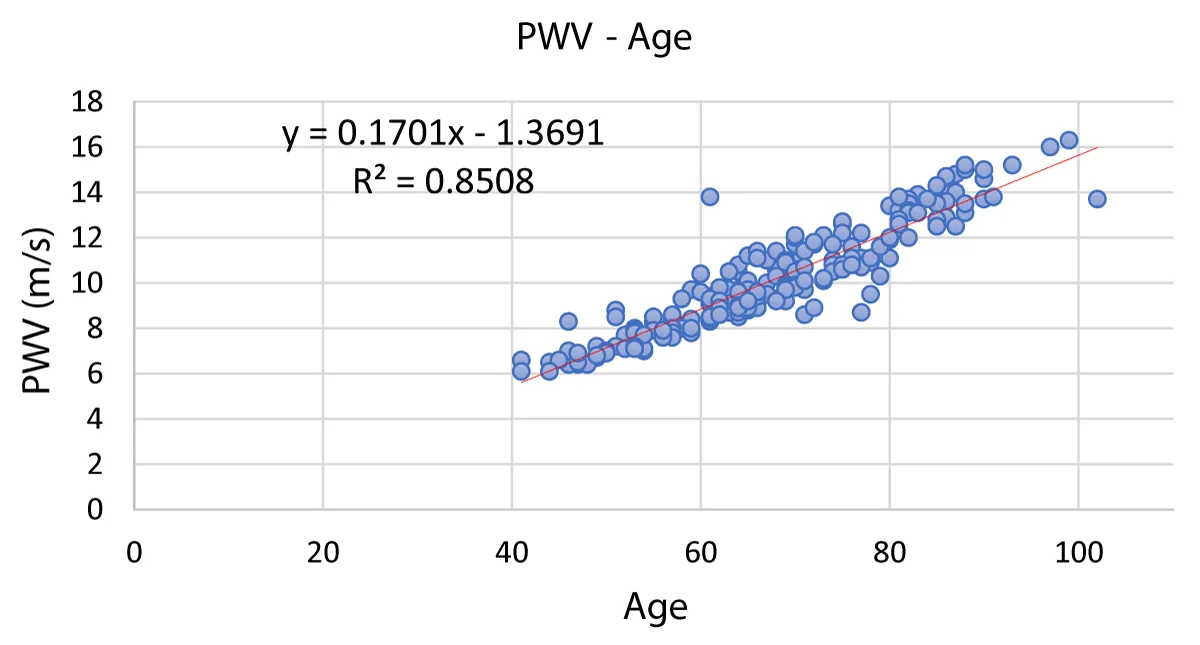
Correlation between pulse wave velocity with age
Figure 1 showed that there was a statistically significant positive correlation with a very strong level between pulse wave velocity and age (r = 0.922, p < 0.001).
Figure 1: Correlation between pulse wave velocity with age. Abbreviation: PWV: Pulse Wave Velocity
Correlation between arterial stiffness index with left ventricular mass index and carotid intima-media thickness
There was a statistically significant positive correlation at a weak level between ABI with LVMI and CIMT, in which the coefficient r was equal to 0.219 (p < 0.05) and 0.250 (p < 0,001) respectively (Table 2). Also, PWV had also a statistically significant positive correlation at a weak level with LVMI and CIMT, in which the coefficient r was equal to 0.188 (p < 0.05) and 0.289 (p < 0,001) respectively (Table 2).
| Table 2: Correlation between arterial stiffness index with left ventricular mass index and carotid intima-media thickness. | ||||
| LVMI (g/m2) | CIMT (mm) | |||
| r | p - value | r | p - value | |
| ABI | 0.219 | < 0.05 | 0.250 | < 0.001 |
| PWV (m/s) | 0.188 | < 0.05 | 0.289 | < 0.001 |
| Abbreviation: ABI: Ankle-Brachial Index; PWV: Pulse Wave Velocity; LVMI: Left Ventricular Mass Index; CIMT: Carotid Intima-Media Thickness. | ||||
Multivariate correlation of pulse wave velocity
This model did not have multicollinearity, adjusted R2 was 41.3%. All predictor variables were statistically significant (p < 0.05). The optimal model to predict left ventricular mass index was as follows: PWV = 0.641*(Gender) – 0.027*(Pulse) + 0.043*(Mean blood pressure) + 8.378*(ABI) – 3.254 (Table 3).
| Table 3. Multivariate correlation of left ventricular mass index. | |||||
| Variables | Beta | SD | CI 95% | p-value | R2 |
| Constant | -3.254 | 1.486 | -6.184 – -0.324 | <0.05 | 41.3% |
| Gender | 0.641 | 0.243 | 0.163 – 1.120 | <0.05 | |
| Pulse | -0.027 | 0.012 | -0.050 – -0.003 | <0.05 | |
| Mean blood pressure | 0.043 | 0.009 | 0.025 – 0.061 | <0.001 | |
| ABI | 8.378 | 0.998 | 6.411 – 10.346 | <0.001 | |
| Abbreviation: ABI: Ankle-Brachial Index; SD: Standard Deviation; CI: Confidence Interval | |||||
When blood is ejected into the aorta, a wave is generated and propagates along the arterial tree. Pulse wave velocity is the velocity of that wave propagation; It depends on these two factors: (i) the movement of blood along the axis of the vessel and (ii) the transverse movement of the vessel wall, meaning the stiffness of the vessel. The greater the vascular resistance is, the less time it takes for the wave to propagate horizontally, and thus, the higher the pulse wave velocity is [13]. This explains why pulse wave velocity is strongly correlated with age. Rosaria Del Giorno, et al. (2020) researched 1162 subjects ≥ 18 years old to compare two methods of measuring pulse wave velocity, tonometry, and oscillometry; the results showed that pulse wave velocity measured at the clinic by oscillometry method, similar to the method in our study, had a very strong positive correlation with age., r = 0.916, p ≤ 0.001), the same our results [14].
Intima media thickness is considered a parameter of structural change in atherosclerosis. In young people with elastic arteries, the reflected wave reaches the heart during diastole, raising the diastolic pressure and improving coronary perfusion. However, in the stiff arteries, pulse wave velocity increases; thus, that wave reaches the heart during systole, leading to increased systolic blood pressure, decreased diastolic blood pressure, and promoted vascular remodeling by excessive collagen production increase intima-media thickness [13]. Research by Jing Tian, et al. (2017) was conducted on 545 subjects to evaluate the correlation between brachial-ankle pulse wave velocity and carotid intima-media thickness in middle-aged people and elders. The results showed that brachial-ankle pulse wave velocity had a statistically significant positive correlation with the carotid intima-media thickness (r = 0.247, p < 0.0001), similar to our study. However, the measurement method between the two studies was different [15].
The left ventricular structure is also impacted by both aging and hypertension. In the elderly, the left ventricular structure is remodeled with an increase in relative wall thickness and, along with hypertension, may result in another geometric remodeling. Thus, arterial stiffness may have differential influences on the left ventricular structure concerned with atherosclerosis [16]. Theodore G. Papaioannou, et al. (2017) carried out a study on 226 subjects to evaluate the relationship between arterial elasticity and left ventricular hypertrophy; they showed that there was a statistically significant positive correlation between carotid-femoral pulse wave velocity and LVMI (r = 0.268, p < 0.001), which was similar to our study [17]. However, research by author Shikai Yu, et al. (2018) was proceeded on 1841 elders to evaluate the association of ABI with target organ damages of hypertension; showed that ABI did not correlate with LVMI and CIMT (r = 0.016 and -0.012, respectively, p > 0.05), which was different from our study. The reason was the difference in sample size and ABI characteristics between the two studies [18].
Through the research, we also found a multivariable correlation between pulse wave velocity and factors such as gender, pulse, mean blood pressure, and ABI. For example, Annelise MG Paiva, et al. (2020) evaluated the multivariable regression model of pulse wave velocity and found that pulse wave velocity had a multivariable correlation with age, male gender, and mean blood pressure; these variables were all statistically significant [19]. Similarly, Rosaria Del Giorno et al. (2020) also showed that pulse wave velocity had a multivariable correlation with age, systolic blood pressure, and heart rate, with statistical significance, R2 = 87.8% [14].
Some limitations of our study should be taken into consideration. One of the most significant limitations was the small sample size, which was insufficient to represent all hypertensive patients. Besides, the measurement of pulse wave velocity, ankle-brachial index, and cardiovascular event parameters such as LVMI and CIMT did not co-occur, which may lead to bias in the research results. Another thing that also needs to be mentioned was that we could not rule out the influence of cardiovascular risk factors such as smoking, obesity, diabetes, dyslipidemia, etc., presenting in study subjects to the relationship between pulse wave velocity and cardiovascular events.
Arterial stiffness measured through pulse wave velocity or ankle-brachial index had a statistically significant correlation with LVMI and CIMT. Through the above research results, we suggest that the hypertensives should be combined with the evaluation of hemodynamic parameters and arterial stiffness for contributing to the diagnosis and detection of cardiovascular complications, thereby improving the quality of monitoring and treatment in hypertensive patients.
Limitations
Some limitations of our study should be taken into consideration. One of the most important limitations was the small sample size, which was not enough to represent all hypertensive patients. Besides, the measurement of pulse wave velocity, ankle-brachial index, and cardiovascular event parameters such as left ventricular mass index and carotid intima-media thickness also did not occur at the same time, which may lead to bias in the research results. Another thing that also needs to be mentioned was that we could not rule out the influence of cardiovascular risk factors such as smoking, obesity, diabetes, dyslipidemia, etc… presenting in study subjects to the relationship between pulse wave velocity and cardiovascular events.
Funding: This research was funded by Hue University (No. 084 2343825866) and the Domestic Master/ Ph. D Scholarship Programme of Vingroup Innovation Foundation ([email protected]).
Institutional review board statement: The study was conducted by the Declaration of Helsinki, and approved by the Ethical Review Committee of Hue University of Medicine and Pharmacy, Vietnam (IRB no. H2018/374)
Informed consent statement: Informed consent was obtained from all subjects involved in the study.
Data availability statement: Not applicable.
Acknowledgments: The authors would like to thank the doctors and nurses who helped with data collection.
Conflicts of interest: The authors declare no conflict of interest.
- Beaney T, Schutte AE, Stergiou GS, Borghi C, Burger D, Charchar F, Cro S, Diaz A, Damasceno A, Espeche W, Jose AP, Khan N, Kokubo Y, Maheshwari A, Marin MJ, More A, Neupane D, Nilsson P, Patil M, Prabhakaran D, Ramirez A, Rodriguez P, Schlaich M, Steckelings UM, Tomaszewski M, Unger T, Wainford R, Wang J, Williams B, Poulter NR; MMM Investigators*. May Measurement Month 2019: The Global Blood Pressure Screening Campaign of the International Society of Hypertension. Hypertension. 2020 Aug;76(2):333-341. doi: 10.1161/HYPERTENSIONAHA.120.14874. Epub 2020 May 18. PMID: 32419505.
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017 Mar 7;135(10):e146-e603. doi: 10.1161/CIR.0000000000000485. Epub 2017 Jan 25. Erratum in: Circulation. 2017 Mar 7;135(10 ):e646. Erratum in: Circulation. 2017 Sep 5;136(10 ):e196. PMID: 28122885; PMCID: PMC5408160.
- Shanthi M. Global status report on noncommunicable diseases. World Health Organization. 2014; 67-9.
- Kjeldsen SE. Hypertension and cardiovascular risk: General aspects. Pharmacol Res. 2018;129:95-9.
- Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, Wainford RD, Williams B, Schutte AE. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020 Jun;75(6):1334-1357. doi: 10.1161/HYPERTENSIONAHA.120.15026. Epub 2020 May 6. PMID: 32370572.
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339. Erratum in: Eur Heart J. 2019 Feb 1;40(5):475. PMID: 30165516.
- Bruno RM, Cartoni G, Stea F, Armenia S, Bianchini E, Buralli S, Giannarelli C, Taddei S, Ghiadoni L. Carotid and aortic stiffness in essential hypertension and their relation with target organ damage: the CATOD study. J Hypertens. 2017 Feb;35(2):310-318. doi: 10.1097/HJH.0000000000001167. PMID: 27841779; PMCID: PMC5486968.
- Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Jun 24;129(25 Suppl 2):S49-73. doi: 10.1161/01.cir.0000437741.48606.98. Epub 2013 Nov 12. Erratum in: Circulation. 2014 Jun 24;129(25 Suppl 2):S74-5. PMID: 24222018.
- Vasan RS, Short MI, Niiranen TJ, Xanthakis V, DeCarli C, Cheng S, Seshadri S, Mitchell GF. Interrelations Between Arterial Stiffness, Target Organ Damage, and Cardiovascular Disease Outcomes. J Am Heart Assoc. 2019 Jul 16;8(14):e012141. doi: 10.1161/JAHA.119.012141. Epub 2019 Jul 13. PMID: 31303106; PMCID: PMC6662123.
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015 Jan;28(1):1-39.e14. doi: 10.1016/j.echo.2014.10.003. PMID: 25559473.
- Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F; Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013 Jul;31(7):1281-357. doi: 10.1097/01.hjh.0000431740.32696.cc. PMID: 23817082.
- Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FGR, Hamburg NM, Kinlay S, Lookstein R, Misra S, Mureebe L, Olin JW, Patel RAG, Regensteiner JG, Schanzer A, Shishehbor MH, Stewart KJ, Treat-Jacobson D, Walsh ME. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017 Mar 21;69(11):1465-1508. doi: 10.1016/j.jacc.2016.11.008. Epub 2016 Nov 13. Erratum in: J Am Coll Cardiol. 2017 Mar 21;69(11):1520. PMID: 27851991.
- Nichols WW, O’Rourke M. McDonald’s Blood Flow in Arteries; Theoretical, Experimental and Clinical Principles. Sixth ed. 2011;755.
- Del Giorno R, Troiani C, Gabutti S, Stefanelli K, Gabutti L. Comparing oscillometric and tonometric methods to assess pulse wave velocity: a population-based study. Ann Med. 2021 Dec;53(1):1-16. doi: 10.1080/07853890.2020.1794538. Epub 2020 Aug 13. PMID: 32729734; PMCID: PMC7877928.
- Tian Jea. Brachial-ankle pulse wave velocity is associated with carotid intima-media thickness in middle-aged and elderly. Int J Clin Exper Med. 2017;10:9364-9.
- Kim HL, Lim WH, Seo JB, Chung WY, Kim SH, Kim MA, Zo JH. Association between arterial stiffness and left ventricular diastolic function in relation to gender and age. Medicine (Baltimore). 2017 Jan;96(1):e5783. doi: 10.1097/MD.0000000000005783. PMID: 28072727; PMCID: PMC5228687.
- Papaioannou TG, Protogerou AD, Argyris A, Aissopou E, Georgiopoulos G, Nasothimiou E, Tountas C, Sfikakis PP, Stergiopulos N, Tousoulis D. Total arterial compliance, estimated by a novel method, is better related to left ventricular mass compared to aortic pulse wave velocity: The SAFAR study. Clin Exp Hypertens. 2017;39(3):271-276. doi: 10.1080/10641963.2016.1247165. PMID: 28448191.
- Yu S, Lu Y, Xiong J, Teliewubai J, Chi C, Ji H, Zhou Y, Fan X, Zhang J, Blacher J, Li J, Zhang Y, Xu Y. Comparison of ankle-brachial index and upstroke time in association with target organ damage: the Northern Shanghai Study. J Am Soc Hypertens. 2018 Oct;12(10):703-713. doi: 10.1016/j.jash.2018.06.014. Epub 2018 Jun 30. PMID: 30056134.
- Paiva AMG, Mota-Gomes MA, Brandão AA, Silveira FS, Silveira MS, Okawa RTP, Feitosa ADM, Sposito AC, Nadruz W Jr. Reference values of office central blood pressure, pulse wave velocity, and augmentation index recorded by means of the Mobil-O-Graph PWA monitor. Hypertens Res. 2020 Nov;43(11):1239-1248. doi: 10.1038/s41440-020-0490-5. Epub 2020 Jun 12. PMID: 32533101.