More Information
Submitted: October 10, 2022 | Approved: October 26, 2022 | Published: October 27, 2022
How to cite this article: Tsougos E, Giallafos E, Paraskevaidis I. Atrial fibrillation in elite athletes. What is missing? J Cardiol Cardiovasc Med. 2022; 7: 085-092.
DOI: 10.29328/journal.jccm.1001139
Copyright License: © 2022 Tsougos E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Atrial fibrillation in elite athletes. What is missing?
E Tsougos, E Giallafos * and I Paraskevaidis
* and I Paraskevaidis
1st Department of Neurology, University of Athens, Hygeia Hospital, Erithrou Stavrou 4 & Kifisias Avenue, 151 23 Marousi, Athens, Greece
*Address for Correspondence: E Giallafos, 1st Department of Neurology, University of Athens, Hygeia Hospital, Erithrou Stavrou 4 & Kifisias Avenue, 151 23 Marousi, Athens, Greece, Email: [email protected]
Although the beneficial effect of physical activity in the general population is well established, in elite athletes under vigorous physical activity, the effect on the electrical system of the heart is controversial. Indeed, several studies have shown an increased rate of atrial fibrillation among athletes, whereas others suggest that improved exercise capacity with training reduces atrial fibrillation recurrence. The pathophysiologic explanation of that discrepancy is missing, although several underlying mechanisms have been proposed. Taking into account the current knowledge, it seems that, although the beneficial effects of exercise are well recognized, there are conflicting data regarding the relation of the occurrence - the rate of atrial fibrillation to high-volume exercise and too long-term training. Its significance on the quality of life especially in highly trained athletes remains to be elucidated. Therefore, this short review will try to discuss this discrepancy and hopefully underlie the arising arguments.
In the general population as well as in patients with cardiovascular disease, several reports strongly recommend physical activity in order to increase cardiorespiratory capacity and fitness [1,2]. In keeping with these studies, exercise training seems to improve endothelial dysfunction, attenuate atherosclerotic plaque vulnerability and ameliorate functional capacity and muscle strength [3,4]. Additionally, exercise tends to normalize several cardiovascular risk factors such as hypertension and cardio-metabolic disorders. Hence reducing morbidity and mortality [5-7]. Therefore, physical activity is highly recommended in a diseased and healthy population [8]. However, it is unclear whether the amount of exercise is associated with beneficial effects. Of note, it has been proposed that 15 min per day or 90 min per week of moderate-intensity exercise is beneficial [9], whereas marathon runners performing a prolonged vigorous activity show biochemical and echocardiographic evidence of cardiac dysfunction and injury [10]. Notably, although the beneficial effect of normal physical activity in the general population is well established, in elite athletes under vigorous physical activity the effect on the electrical system of the heart is controversial. Indeed, several studies suggest an increased rate of atrial fibrillation among athletes [11-13], as well as in the normal population caused by the high volume of exercise effort [14,15]. On the contrary, other studies suggest ‘that both greater exercise capacity and increases in exercise capacity with exercise training reduce atrial fibrillation recurrence change [16]. However, it is noteworthy that athletes performing rigorous training are dealing with a high workload that is much greater than that proposed for heart disease prevention [17,18]. The pathophysiologic explanation of this discrepancy is still missing, likely proposed causes include sympathetic/parasympathetic tone unbalance, left atrial and/or left ventricular dilatation, and hypertrophy [19-24].
Atrial fibrillation (AF) is a very common cardiac arrhythmia with the incidence in adults ranging between 0.5% - 15% with linear relation to age [25,26]. Its association with cardiovascular mortality is well established. Its etiology is multifactorial, including non-modifiable causes such as increased age, sex, and genetic factors, as well as modifiable ones such as hypertension, diabetes mellitus, heart failure, and coronary artery disease [27]. According to current knowledge, although the beneficial effects of exercise physical activity are well recognized, there are conflicting data regarding the relationship between the occurrence - the rate of atrial fibrillation and high volume or prolonged exercise. Its effect on the quality of life especially in highly trained athletes remains to be elucidated. Therefore, this short review will try to discuss this discrepancy and hopefully underlie the arising arguments.
Define an ‘Athlete’
Until recently different definitions existed in an attempt to identify the truly-active athlete. This has led to confusion, complicating published results interpretation. In 2016 a working definition for an athlete was suggested for medical and health sciences research proposing four criteria: 1, training in sports aiming to improve his/her performance/results; 2, actively participating in sports competitions; 3, formally registered in a local, regional, or national sports federation; 4, sports training and competition being the main activity (way of living) or focus of personal interest, devoting several hours in all or most of the days, exceeding the time allocated to other types of professional or leisure activities [28]. The latest European Society of Cardiology Guidelines on sports cardiology suggested that the definition of “athlete” has to depend on the degree of exercise. Thus, 3 categories were proposed according to to exercise volume; ‘elite’ athletes, who generally exercise ≥ 10 h/week ‘competitive’ athletes who exercise ≥ 6 h/week, and ‘recreational’ athletes who exercise ≥ 4 h/week. However, as the authors state, this distinction is arbitrary [29].
The lack of a clear definition and classification leads to confusion in the studies’ results interpretation. Some studies enroll different subjects with different profiles and levels of competition or subjects that do not fulfill all the criteria of the ‘athlete’ definition. This highlights the need for a universally accepted definition of ‘athlete’.
Pathophysiology - approach of adverse outcome in Athletes
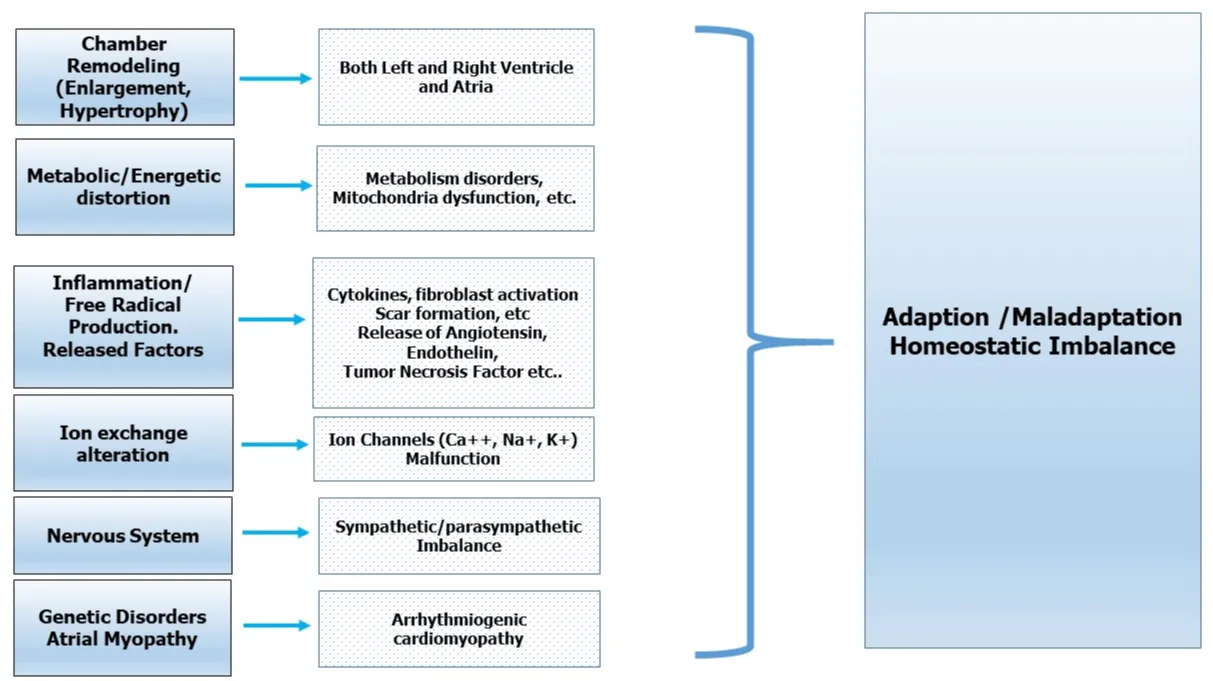
During high-volume exercise, there is a cardiovascular and peripheral (skeletal muscle) adaptation characterized by the increase of pre- and after-load, heart rate and cardiac output, enlargement of cardiac chambers, and increase in catecholamine production and oxygen demand (Figure 1). This adaptation in some cases (e.g. marathon runners) could be rather harmful, as suggested by the increase in cardiac biomarkers such as troponin, CK-MB, and BNP. Furthermore, free radical production, inflammation, and immune and fibroblast cell activation lead to a fibrotic process in the myocardium, creating a potentially arrhythmogenic substrate associated with all sorts of arrhythmias and sudden cardiac death [18,30-32]. Interestingly, the exercise-related cardiac remodeling noticed in most professional athletes is not restored in all cases after cessation of competitive activity [30,33-38] highlighting the need for methods and markers to allow identification of those individuals. Moreover, a hypothesis of a yet unrecognized structural remodeling, promoting a scarring process [39,40], or even ion exchange alteration has been suggested. Findings from studies on cardiac MRI are conflicting; some have reported patchy myocardial scarring in 12% or even 50% of marathon athletes [30,36,41] suggesting probably a source of myocardial electrical instability, while others showed a similar amount of fibrosis between athletes and controls [42,43]. Interestingly, studies in a small group of trainees have shown that a high volume of exercise may lead to right ventricular dysfunction and to myocardial fibrosis [30,32], with unknown consequences [18,30,32,44,45]. In any case, given the lack of data the speculated term exercise-induced arrhythmogenic cardiomyopathy is on the table [46].
Figure 1: Presumed mechanism of Atrial Fibrillation in Athletes.
Atrial fibrillation and physical activity
In the general population, atrial fibrillation might be the result of either a trigger effect caused by atrial ectopy or cardiac substrate modulation due to hypertension, coronary artery disease, valvular heart disease, myocarditis, and heart failure. However, this is not the case in young highly trained persons. In this particular population, the underlying mechanism of atrial fibrillation is rather speculative. Some studies indicate no relationship between physical activity and atrial fibrillation [8,47,48] whereas, others [49], suggest a close association between them. Keeping this discrepancy on the road there are published data that relate the time of exercise or the presumed AF treatment, with this superventricular arrhythmia [50,51]. On the other hand, there are reports with no relation between a high volume of exercise and risk for atrial fibrillation [52]. The latest guidelines on sports cardiology do not elaborate on the impact of atrial fibrillation and its relation to physical activity. Indeed, the authors underline their ignorance on this topic by stating that ‘The threshold lifetime sports activity for increasing the risk of developing AF is unknown. It is also unknown whether ongoing participation in vigorous exercise at the same intensity after successful AF ablation is associated with a higher risk of AF recurrence’ [29]. Thus, the etiology of AF in highly trained people has to be elucidated, although several mechanisms Figure 1, such as cardiac chamber remodeling, genetic predisposition, sympathetic/parasympathetic tone imbalance, fibrosis, and inflammation have been suggested. 18,20,23,24 Certain inherited gene defects might, under the presence of environmental factors like aging, obesity, systemic inflammation, arterial hypertension, and/or diabetes mellitus, promote chamber remodeling, alter the atrial electrophysiological properties, and finally establish atrial fibrillation [52A,52B]. Elite athlete’s remodeling can be caused by long-term high volume exercise which may trigger arrhythmogenesis [13,31,34,36,53,55-57], due to several factors including atrial wall fibrosis, a potential source of re-entry circuits [23,57]. Additionally, the injured myocardium in active highly trained athletes such as marathon runners may have created a very subtle substrate; cardiac fibrosis, or even Ca++, K+, Na+ channel alteration/dysregulation, that is a source and a consequence of electrical instability. Another suggested trigger mechanism for atrial fibrillation is increased nervous system activity which is common in highly trained people. However, the increased activity is countered by the functional sympatholysis [58-61] which creates a local rather than a global effect making the increased sympathetic activity as a trigger for atrial fibrillation less likely. Although parasympathetic activity might be a potential mechanism since triggers localized reentry, it seems that this is not the case unless there is an ectopic activity on pulmonary veins that is activated by the increased vagal tone that promotes a shortening of the atrial refractory period [11,23]. Thus, the sympathetic/parasympathetic ratio activity is less likely to be the main cause of atrial fibrillation induction [62].
Interestingly, it seems that long-term rigorous training may lead to left atrial remodeling which might be the source of atrial fibrillation [13,41,63,64]. Indeed, this has been proposed in an experimental model by showing an increased atrial fibrillation susceptibility due probably to a fibrosis process [41].
Atria and physical activity
Although in the general population there are convincing data showing the close relation between left atrial remodeling and atrial fibrillation, in the case of the highly trained population there are conflicting data. Indeed, several studies in athletes have suggested an association between left atrial remodeling and atrial fibrillation [23,65-69], whereas others doubt this concept by stating that ‘LA enlargement represents an innocent consequence of chronic and intensive exercise conditioning’ [70]. Accordingly, it has been shown that although the left atrial is enlarged in athletes, its function remains normal or even is improved [71,72]. Moreover, no relationship between left atrial enlargement and electrophysiologic remodeling has been clearly demonstrated [71,73]. Several pathophysiological changes occur in both atria occur during exercise. The heart is forced to augment the stroke volume in order to satisfy the metabolic needs of the body. The increased negative left ventricular early diastolic pressure leads to a larger downslope motion of both mitral and tricuspid annulus resulting in an increased atrial reservoir phase. [74-76]. Additionally, the atrial contraction phase is increased due to the high atrial pressure [77] along with the shortening of the conduit phase. Although the physiologic adaptation of both atria is well proven, it remains a fact that low to median exercise is beneficial whereas in highly trained athletes it could be detrimental. However, the latest is not the case for all highly trained athletes. Therefore, there must be a differentiation in both adaptive and maladaptive processes [78]. In fact, the capacity of the organism to overcome myocyte hypertrophy, inflammation, fibrosis, free radical production, released factors such as angiotensin, tumor growth factor, endothelin, etc [79-85], as well as the energetic and metabolic disturbances/maladaptation [86-88] is crucial and therefore we have to pay attention on this particular and very elegant topic (Figure 1). However, mechanisms related to energy and cellular metabolism are highly complicated and dependent on many intrinsic and extrinsic factors including specific high-energy food intake or even anabolic capture substances. For instance, an elite athlete’s performance is influenced by diet habit status during different religious beliefs (Christian fasting state, Ramadan for Muslims) which interfere with circadian rhythm. These mechanisms have a synergistic effect on the Autonomic Nervous System disturbance and promote the induction and/or persistence of AF [88A,88B].
Understanding the ambiguity
Several explanations might be proposed in order to justify our poor understanding. For instance, the existing variety of definitions of training as demonstrated by several studies that took into account both the amount [89-95] and the long-term physical activity must be taken into account. The U-shape relation between atrial fibrillation and the volume of exercise might be a reason [8,9,53,91,96], along with the lack of this relation in women [91]. Studies with a more homogeneous population as far as sex, the volume of exercise load, and duration of exercise shall be designed in order to reach a more reasonable conclusion. Moreover, many studies have enrolled veteran athletes which might have affected the results and consequently the conclusions. Several reports suffer from statistical heterogeneity suggesting conclusions of questionable significance. We do need to conduct studies methodologically and properly designed. Is it reasonable to enroll ‘athletes’ of different sex, age, type, frequency and volume of exercise, daily duration of exercise, or even weekly or annual duration? Is the sample size powered enough to give such conclusions? Are all the enrolled ‘athletes’ under the same regimen of their day-life habits? [15,50,56,96]. Of note, in an attempt to overpass these limitations a systematic review and meta-analysis have been recently published, but as the authors admit, their review is limited by the strict methodological criteria that they applied; excluding a high number of studies, indicating thus the need for performing larger and more accurately designed studies [98]. Surprisingly, there is also a lack of concrete data concerning the occurrence of atrial fibrillation. According to a study that comprise highly trained athletes [70], the occurrence - rate of atrial fibrillation is only 0.2-0.3% whereas others found a much higher incidence [14,15,53,56,70,96,99-107], reaching even 31%.
Although the distinction between physiological and abnormal response is more or less clear [78], it must be taken into account the capability of new well-designed studies to predict those who are prone to overpass the homeostatic balance.
In conclusion, atrial fibrillation is an arrhythmia that is present in a variable percentage of highly trained individuals with unknown so far etiology. The cause and the pathophysiologic background of this arrhythmogenic event remain to be elucidated. The scientific community should take into account the raised discrepancies and conduct a properly designed study. Importantly, we have to focus on those highly trained individuals who have the profile/characteristics to present not only this particular arrhythmia but any cardiac harmful event.
- Franklin BA, Lavie CJ, Squires RW, Milani RV. Exercise-based cardiac rehabilitation and improvements in cardiorespiratory fitness: implications regarding patient benefit. Mayo Clin Proc. 2013 May;88(5):431-7. doi: 10.1016/j.mayocp.2013.03.009. PMID: 23639495.
- Lavie CJ, Arena R, Swift DL, Johannsen NM, Sui X, Lee DC, Earnest CP, Church TS, O'Keefe JH, Milani RV, Blair SN. Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circ Res. 2015 Jul 3;117(2):207-19. doi: 10.1161/CIRCRESAHA.117.305205. PMID: 26139859; PMCID: PMC4493772.
- Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011 Aug 16;124(7):789-95. doi: 10.1161/CIRCULATIONAHA.110.010710. Epub 2011 Aug 1. PMID: 21810663; PMCID: PMC3158733.
- Fernández-Rubio H, Becerro-de-Bengoa-Vallejo R, Rodríguez-Sanz D, Calvo-Lobo C, Vicente-Campos D, Chicharro JL. Exercise Training and Interventions for Coronary Artery Disease. J Cardiovasc Dev Dis. 2022 Apr 25;9(5):131. doi: 10.3390/jcdd9050131. PMID: 35621842; PMCID: PMC9146277.
- Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, Berra K, Blair SN, Costa F, Franklin B, Fletcher GF, Gordon NF, Pate RR, Rodriguez BL, Yancey AK, Wenger NK; American Heart Association Council on Clinical Cardiology Subcommittee on Exercise, Rehabilitation, and Prevention; American Heart Association Council on Nutrition, Physical Activity, and Metabolism Subcommittee on Physical Activity. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation. 2003 Jun 24;107(24):3109-16. doi: 10.1161/01.CIR.0000075572.40158.77. PMID: 12821592.
- Mora S, Cook N, Buring JE, Ridker PM, Lee IM. Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms. Circulation. 2007 Nov 6;116(19):2110-8. doi: 10.1161/CIRCULATIONAHA.107.729939. Epub 2007 Oct 22. PMID: 17967770; PMCID: PMC2117381.
- Myint PK, Luben RN, Wareham NJ, Welch AA, Bingham SA, Khaw KT. Physical activity and fibrinogen concentrations in 23,201 men and women in the EPIC-Norfolk population-based study. Atherosclerosis. 2008 Jun;198(2):419-25. doi: 10.1016/j.atherosclerosis.2007.09.021. Epub 2007 Oct 30. PMID: 17977548.
- Kwok CS, Anderson SG, Myint PK, Mamas MA, Loke YK. Physical activity and incidence of atrial fibrillation: a systematic review and meta-analysis. Int J Cardiol. 2014 Dec 15;177(2):467-76. doi: 10.1016/j.ijcard.2014.09.104. Epub 2014 Sep 28. PMID: 25443248.
- Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, Chan HT, Tsao CK, Tsai SP, Wu X. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011 Oct 1;378(9798):1244-53. doi: 10.1016/S0140-6736(11)60749-6. Epub 2011 Aug 16. PMID: 21846575
- Neilan TG, Januzzi JL, Lee-Lewandrowski E, Ton-Nu TT, Yoerger DM, Jassal DS, Lewandrowski KB, Siegel AJ, Marshall JE, Douglas PS, Lawlor D, Picard MH, Wood MJ. Myocardial injury and ventricular dysfunction related to training levels among nonelite participants in the Boston marathon. Circulation. 2006 Nov 28;114(22):2325-33. doi: 10.1161/CIRCULATIONAHA.106.647461. Epub 2006 Nov 13. PMID: 17101848.
- Elosua R, Arquer A, Mont L, Sambola A, Molina L, García-Morán E, Brugada J, Marrugat J. Sport practice and the risk of lone atrial fibrillation: a case-control study. Int J Cardiol. 2006 Apr 14;108(3):332-7. doi: 10.1016/j.ijcard.2005.05.020. Epub 2005 Jun 16. Erratum in: Int J Cardiol. 2007 Dec 15;123(1):74. PMID: 15963583.
- Karjalainen J, Kujala UM, Kaprio J, Sarna S, Viitasalo M. Lone atrial fibrillation in vigorously exercising middle aged men: case-control study. BMJ. 1998 Jun 13;316(7147):1784-5. doi: 10.1136/bmj.316.7147.1784. PMID: 9624065; PMCID: PMC28577.
- Molina L, Mont L, Marrugat J, Berruezo A, Brugada J, Bruguera J, Rebato C, Elosua R. Long-term endurance sport practice increases the incidence of lone atrial fibrillation in men: a follow-up study. Europace. 2008 May;10(5):618-23. doi: 10.1093/europace/eun071. Epub 2008 Apr 4. PMID: 18390875.
- Everett BM, Conen D, Buring JE, Moorthy MV, Lee IM, Albert CM. Physical activity and the risk of incident atrial fibrillation in women. Circ Cardiovasc Qual Outcomes. 2011 May;4(3):321-7. doi: 10.1161/CIRCOUTCOMES.110.951442. Epub 2011 Apr 12. PMID: 21487092; PMCID: PMC3097307..
- Frost L, Frost P, Vestergaard P. Work related physical activity and risk of a hospital discharge diagnosis of atrial fibrillation or flutter: the Danish Diet, Cancer, and Health Study. Occup Environ Med. 2005 Jan;62(1):49-53. doi: 10.1136/oem.2004.014266. PMID: 15613608; PMCID: PMC1740844.
- Pathak RK, Elliott A, Middeldorp ME, Meredith M, Mehta AB, Mahajan R, Hendriks JM, Twomey D, Kalman JM, Abhayaratna WP, Lau DH, Sanders P. Impact of CARDIOrespiratory FITness on Arrhythmia Recurrence in Obese Individuals With Atrial Fibrillation: The CARDIO-FIT Study. J Am Coll Cardiol. 2015 Sep 1;66(9):985-96. doi: 10.1016/j.jacc.2015.06.488. Epub 2015 Jun 22. PMID: 26113406.
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A; American College of Sports Medicine; American Heart Association. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007 Aug 28;116(9):1081-93. doi: 10.1161/CIRCULATIONAHA.107.185649. Epub 2007 Aug 1. PMID: 17671237.
- Sharma S, Zaidi A. Exercise-induced arrhythmogenic right ventricular cardiomyopathy: fact or fallacy? Eur Heart J. 2012 Apr;33(8):938-40. doi: 10.1093/eurheartj/ehr436. Epub 2011 Dec 6. PMID: 22160405.
- Aizer A, Gaziano JM, Cook NR, Manson JE, Buring JE, Albert CM. Relation of vigorous exercise to risk of atrial fibrillation. Am J Cardiol. 2009 Jun 1;103(11):1572-7. doi: 10.1016/j.amjcard.2009.01.374. Epub 2009 Apr 22. PMID: 19463518; PMCID: PMC2687527.
- O'Sullivan SE, Bell C. The effects of exercise and training on human cardiovascular reflex control. J Auton Nerv Syst. 2000 Jul 3;81(1-3):16-24. doi: 10.1016/s0165-1838(00)00148-x. PMID: 10869695.
- ALESSI R, NUSYNOWITZ M, ABILDSKOV JA, MOE GK. Nonuniform distribution of vagal effects on the atrial refractory period. Am J Physiol. 1958 Aug;194(2):406-10. doi: 10.1152/ajplegacy.1958.194.2.406. PMID: 13559489.
- HOFF HE, GEDDES LA. Cholinergic factor in auricular fibrillation. J Appl Physiol. 1955 Sep;8(2):177-92. doi: 10.1152/jappl.1955.8.2.177. PMID: 13263261.
- Mont L, Sambola A, Brugada J, Vacca M, Marrugat J, Elosua R, Paré C, Azqueta M, Sanz G. Long-lasting sport practice and lone atrial fibrillation. Eur Heart J. 2002 Mar;23(6):477-82. doi: 10.1053/euhj.2001.2802. PMID: 11863350.
- Heidbüchel H, Anné W, Willems R, Adriaenssens B, Van de Werf F, Ector H. Endurance sports is a risk factor for atrial fibrillation after ablation for atrial flutter. Int J Cardiol. 2006 Feb 8;107(1):67-72. doi: 10.1016/j.ijcard.2005.02.043. PMID: 16337500.
- Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJ. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014 Feb 25;129(8):837-47. doi: 10.1161/CIRCULATIONAHA.113.005119. Epub 2013 Dec 17. PMID: 24345399; PMCID: PMC4151302.
- Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med. 1995 Mar 13;155(5):469-73. PMID: 7864703.
- Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL; ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021 Feb 1;42(5):373-498. doi: 10.1093/eurheartj/ehaa612. Erratum in: Eur Heart J. 2021 Feb 1;42(5):507. Erratum in: Eur Heart J. 2021 Feb 1;42(5):546-547. Erratum in: Eur Heart J. 2021 Oct 21;42(40):4194. PMID: 32860505.
- Araújo CG, Scharhag J. Athlete: a working definition for medical and health sciences research. Scand J Med Sci Sports. 2016 Jan;26(1):4-7. doi: 10.1111/sms.12632. PMID: 26750158.
- Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, Collet JP, Corrado D, Drezner JA, Halle M, Hansen D, Heidbuchel H, Myers J, Niebauer J, Papadakis M, Piepoli MF, Prescott E, Roos-Hesselink JW, Graham Stuart A, Taylor RS, Thompson PD, Tiberi M, Vanhees L, Wilhelm M; ESC Scientific Document Group. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021 Jan 1;42(1):17-96. doi: 10.1093/eurheartj/ehaa605. Erratum in: Eur Heart J. 2021 Feb 1;42(5):548-549. PMID: 32860412.
- O'Keefe JH, Patil HR, Lavie CJ, Magalski A, Vogel RA, McCullough PA. Potential adverse cardiovascular effects from excessive endurance exercise. Mayo Clin Proc. 2012 Jun;87(6):587-95. doi: 10.1016/j.mayocp.2012.04.005. Erratum in: Mayo Clin Proc. 2012 Jul;87(7):704. PMID: 22677079; PMCID: PMC3538475.
- Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010 Mar 30;55(13):1318-27. doi: 10.1016/j.jacc.2009.10.061. PMID: 20338492.
- La Gerche A, Burns AT, Mooney DJ, Inder WJ, Taylor AJ, Bogaert J, Macisaac AI, Heidbüchel H, Prior DL. Exercise-induced right ventricular dysfunction and structural remodelling in endurance athletes. Eur Heart J. 2012 Apr;33(8):998-1006. doi: 10.1093/eurheartj/ehr397. Epub 2011 Dec 6. PMID: 22160404.
- Maron BJ, Pelliccia A, Spirito P. Cardiac disease in young trained athletes. Insights into methods for distinguishing athlete's heart from structural heart disease, with particular emphasis on hypertrophic cardiomyopathy. Circulation. 1995 Mar 1;91(5):1596-601. doi: 10.1161/01.cir.91.5.1596. PMID: 7867202.
- Ector J, Ganame J, van der Merwe N, Adriaenssens B, Pison L, Willems R, Gewillig M, Heidbüchel H. Reduced right ventricular ejection fraction in endurance athletes presenting with ventricular arrhythmias: a quantitative angiographic assessment. Eur Heart J. 2007 Feb;28(3):345-53. doi: 10.1093/eurheartj/ehl468. Epub 2007 Jan 22. PMID: 17242015.
- Möhlenkamp S, Lehmann N, Breuckmann F, Bröcker-Preuss M, Nassenstein K, Halle M, Budde T, Mann K, Barkhausen J, Heusch G, Jöckel KH, Erbel R; Marathon Study Investigators; Heinz Nixdorf Recall Study Investigators. Running: the risk of coronary events : Prevalence and prognostic relevance of coronary atherosclerosis in marathon runners. Eur Heart J. 2008 Aug;29(15):1903-10. doi: 10.1093/eurheartj/ehn163. Epub 2008 Apr 21. PMID: 18426850.
- Breuckmann F, Möhlenkamp S, Nassenstein K, Lehmann N, Ladd S, Schmermund A, Sievers B, Schlosser T, Jöckel KH, Heusch G, Erbel R, Barkhausen J. Myocardial late gadolinium enhancement: prevalence, pattern, and prognostic relevance in marathon runners. Radiology. 2009 Apr;251(1):50-7. doi: 10.1148/radiol.2511081118. PMID: 19332846.
- Trivax JE, Franklin BA, Goldstein JA, Chinnaiyan KM, Gallagher MJ, deJong AT, Colar JM, Haines DE, McCullough PA. Acute cardiac effects of marathon running. J Appl Physiol (1985). 2010 May;108(5):1148-53. doi: 10.1152/japplphysiol.01151.2009. Epub 2010 Feb 11. PMID: 20150567.
- Pelliccia A, Maron BJ, De Luca R, Di Paolo FM, Spataro A, Culasso F. Remodeling of left ventricular hypertrophy in elite athletes after long-term deconditioning. Circulation. 2002 Feb 26;105(8):944-9. doi: 10.1161/hc0802.104534. PMID: 11864923.
- Schnell F, Claessen G, La Gerche A, Bogaert J, Lentz PA, Claus P, Mabo P, Carré F, Heidbuchel H. Subepicardial delayed gadolinium enhancement in asymptomatic athletes: let sleeping dogs lie? Br J Sports Med. 2016 Jan;50(2):111-7. doi: 10.1136/bjsports-2014-094546. Epub 2015 Jul 29. PMID: 26224114.
- Zorzi A, Perazzolo Marra M, Rigato I, De Lazzari M, Susana A, Niero A, Pilichou K, Migliore F, Rizzo S, Giorgi B, De Conti G, Sarto P, Serratosa L, Patrizi G, De Maria E, Pelliccia A, Basso C, Schiavon M, Bauce B, Iliceto S, Thiene G, Corrado D. Nonischemic Left Ventricular Scar as a Substrate of Life-Threatening Ventricular Arrhythmias and Sudden Cardiac Death in Competitive Athletes. Circ Arrhythm Electrophysiol. 2016 Jul;9(7):e004229. doi: 10.1161/CIRCEP.116.004229. PMID: 27390211; PMCID: PMC4956679.
- Benito B, Gay-Jordi G, Serrano-Mollar A, Guasch E, Shi Y, Tardif JC, Brugada J, Nattel S, Mont L. Cardiac arrhythmogenic remodeling in a rat model of long-term intensive exercise training. Circulation. 2011 Jan 4;123(1):13-22. doi: 10.1161/CIRCULATIONAHA.110.938282. Epub 2010 Dec 20. PMID: 21173356.
- D'Ascenzi F, Cameli M, Padeletti M, Lisi M, Zacà V, Natali B, Malandrino A, Alvino F, Morelli M, Vassallo GM, Meniconi C, Bonifazi M, Causarano A, Mondillo S. Characterization of right atrial function and dimension in top-level athletes: a speckle tracking study. Int J Cardiovasc Imaging. 2013 Jan;29(1):87-94. doi: 10.1007/s10554-012-0063-z. Epub 2012 May 16. PMID: 22588713.
- D'Ascenzi F, Pelliccia A, Natali BM, Zacà V, Cameli M, Alvino F, Malandrino A, Palmitesta P, Zorzi A, Corrado D, Bonifazi M, Mondillo S. Morphological and functional adaptation of left and right atria induced by training in highly trained female athletes. Circ Cardiovasc Imaging. 2014 Mar;7(2):222-9. doi: 10.1161/CIRCIMAGING.113.001345. Epub 2014 Jan 27. PMID: 24470314.
- Spirito P, Pelliccia A, Proschan MA, Granata M, Spataro A, Bellone P, Caselli G, Biffi A, Vecchio C, Maron BJ. Morphology of the "athlete's heart" assessed by echocardiography in 947 elite athletes representing 27 sports. Am J Cardiol. 1994 Oct 15;74(8):802-6. doi: 10.1016/0002-9149(94)90439-1. PMID: 7942554.
- Pelliccia A, Culasso F, Di Paolo FM, Maron BJ. Physiologic left ventricular cavity dilatation in elite athletes. Ann Intern Med. 1999 Jan 5;130(1):23-31. doi: 10.7326/0003-4819-130-1-199901050-00005. PMID: 9890846.
- La Gerche A. Exercise-Induced Arrhythmogenic (Right Ventricular) Cardiomyopathy Is Real…if you Consider it. JACC Cardiovasc Imaging. 2021 Jan;14(1):159-161. doi: 10.1016/j.jcmg.2020.09.014. Epub 2020 Nov 18. PMID: 33221208.
- Ofman P, Khawaja O, Rahilly-Tierney CR, Peralta A, Hoffmeister P, Reynolds MR, Gaziano JM, Djousse L. Regular physical activity and risk of atrial fibrillation: a systematic review and meta-analysis. Circ Arrhythm Electrophysiol. 2013 Apr;6(2):252-6. doi: 10.1161/CIRCEP.113.000147. Epub 2013 Mar 20. PMID: 23515264.
- Müller-Riemenschneider F, Andersohn F, Ernst S, Willich SN. Association of physical activity and atrial fibrillation. J Phys Act Health. 2012 Jul;9(5):605-16. doi: 10.1123/jpah.9.5.605. Epub 2011 Jul 29. PMID: 21946769.
- Nielsen JR, Wachtell K, Abdulla J. The Relationship Between Physical Activity and Risk of Atrial Fibrillation-A Systematic Review and Meta-Analysis. J Atr Fibrillation. 2013 Feb 12;5(5):789. doi: 10.4022/jafib.789. PMID: 28496815; PMCID: PMC5153110.
- Drca N, Wolk A, Jensen-Urstad M, Larsson SC. Atrial fibrillation is associated with different levels of physical activity levels at different ages in men. Heart. 2014 Jul;100(13):1037-42. doi: 10.1136/heartjnl-2013-305304. Epub 2014 May 14. PMID: 24829373.
- Thelle DS, Selmer R, Gjesdal K, Sakshaug S, Jugessur A, Graff-Iversen S, Tverdal A, Nystad W. Resting heart rate and physical activity as risk factors for lone atrial fibrillation: a prospective study of 309,540 men and women. Heart. 2013 Dec;99(23):1755-60. doi: 10.1136/heartjnl-2013-303825. Epub 2013 Jun 8. PMID: 23749790.
- Knuiman M, Briffa T, Divitini M, Chew D, Eikelboom J, McQuillan B, Hung J. A cohort study examination of established and emerging risk factors for atrial fibrillation: the Busselton Health Study. Eur J Epidemiol. 2014 Mar;29(3):181-90. doi: 10.1007/s10654-013-9875-y. Epub 2014 Jan 4. PMID: 24389686.
- 52. A. Otway R, Vandenberg JI, Guo G, Varghese A, Castro ML, Liu J, Zhao J, Bursill JA, Wyse KR, Crotty H, Baddeley O, Walker B, Kuchar D, Thorburn C, Fatkin D. Stretch-sensitive KCNQ1 mutation A link between genetic and environmental factors in the pathogenesis of atrial fibrillation? J Am Coll Cardiol. 2007 Feb 6;49(5):578-86. doi: 10.1016/j.jacc.2006.09.044. Epub 2007 Jan 22. PMID: 17276182.
- 52 B . Pretorius L, Du XJ, Woodcock EA, Kiriazis H, Lin RC, Marasco S, Medcalf RL, Ming Z, Head GA, Tan JW, Cemerlang N, Sadoshima J, Shioi T, Izumo S, Lukoshkova EV, Dart AM, Jennings GL, McMullen JR. Reduced phosphoinositide 3-kinase (p110alpha) activation increases the susceptibility to atrial fibrillation. Am J Pathol. 2009 Sep;175(3):998-1009. doi: 10.2353/ajpath.2009.090126. Epub 2009 Aug 13. PMID: 19679877; PMCID: PMC2731119.
- Aizer A, Gaziano JM, Cook NR, Manson JE, Buring JE, Albert CM. Relation of vigorous exercise to risk of atrial fibrillation. Am J Cardiol. 2009 Jun 1;103(11):1572-7. doi: 10.1016/j.amjcard.2009.01.374. Epub 2009 Apr 22. PMID: 19463518; PMCID: PMC2687527.
- ALESSI R, NUSYNOWITZ M, ABILDSKOV JA, MOE GK. Nonuniform distribution of vagal effects on the atrial refractory period. Am J Physiol. 1958 Aug;194(2):406-10. doi: 10.1152/ajplegacy.1958.194.2.406. PMID: 13559489.
- Goel R, Majeed F, Vogel R, Corretti MC, Weir M, Mangano C, White C, Plotnick GD, Miller M. Exercise-induced hypertension, endothelial dysfunction, and coronary artery disease in a marathon runner. Am J Cardiol. 2007 Mar 1;99(5):743-4. doi: 10.1016/j.amjcard.2006.09.127. Epub 2007 Jan 11. PMID: 17317385.
- Mont L, Tamborero D, Elosua R, Molina I, Coll-Vinent B, Sitges M, Vidal B, Scalise A, Tejeira A, Berruezo A, Brugada J; GIRAFA (Grup Integrat de Recerca en Fibril-lació Auricular) Investigators. Physical activity, height, and left atrial size are independent risk factors for lone atrial fibrillation in middle-aged healthy individuals. Europace. 2008 Jan;10(1):15-20. doi: 10.1093/europace/eum263. Epub 2008 Jan 4. PMID: 18178694.
- Kirchhof P, Lip GY, Van Gelder IC, Bax J, Hylek E, Kaab S, Schotten U, Wegscheider K, Boriani G, Brandes A, Ezekowitz M, Diener H, Haegeli L, Heidbuchel H, Lane D, Mont L, Willems S, Dorian P, Aunes-Jansson M, Blomstrom-Lundqvist C, Borentain M, Breitenstein S, Brueckmann M, Cater N, Clemens A, Dobrev D, Dubner S, Edvardsson NG, Friberg L, Goette A, Gulizia M, Hatala R, Horwood J, Szumowski L, Kappenberger L, Kautzner J, Leute A, Lobban T, Meyer R, Millerhagen J, Morgan J, Muenzel F, Nabauer M, Baertels C, Oeff M, Paar D, Polifka J, Ravens U, Rosin L, Stegink W, Steinbeck G, Vardas P, Vincent A, Walter M, Breithardt G, Camm AJ. Comprehensive risk reduction in patients with atrial fibrillation: emerging diagnostic and therapeutic options--a report from the 3rd Atrial Fibrillation Competence NETwork/European Heart Rhythm Association consensus conference. Europace. 2012 Jan;14(1):8-27. doi: 10.1093/europace/eur241. Epub 2011 Jul 26. PMID: 21791573; PMCID: PMC3236658.
- Vongpatanasin W, Wang Z, Arbique D, Arbique G, Adams-Huet B, Mitchell JH, Victor RG, Thomas GD. Functional sympatholysis is impaired in hypertensive humans. J Physiol. 2011 Mar 1;589(Pt 5):1209-20. doi: 10.1113/jphysiol.2010.203026. Epub 2011 Jan 4. PMID: 21224235; PMCID: PMC3060597.
- REMENSNYDER JP, MITCHELL JH, SARNOFF SJ. Functional sympatholysis during muscular activity. Observations on influence of carotid sinus on oxygen uptake. Circ Res. 1962 Sep;11:370-80. doi: 10.1161/01.res.11.3.370. PMID: 13981593.
- Hansen J, Thomas GD, Harris SA, Parsons WJ, Victor RG. Differential sympathetic neural control of oxygenation in resting and exercising human skeletal muscle. J Clin Invest. 1996 Jul 15;98(2):584-96. doi: 10.1172/JCI118826. PMID: 8755671; PMCID: PMC507464.
- Hellsten Y, Nyberg M. Cardiovascular Adaptations to Exercise Training. Compr Physiol. 2015 Dec 15;6(1):1-32. doi: 10.1002/cphy.c140080. PMID: 26756625.
- Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circ Res. 2017 Apr 28;120(9):1501-1517. doi: 10.1161/CIRCRESAHA.117.309732. PMID: 28450367; PMCID: PMC5500874.
- D'Andrea A, Riegler L, Cocchia R, Scarafile R, Salerno G, Gravino R, Golia E, Vriz O, Citro R, Limongelli G, Calabrò P, Di Salvo G, Caso P, Russo MG, Bossone E, Calabrò R. Left atrial volume index in highly trained athletes. Am Heart J. 2010 Jun;159(6):1155-61. doi: 10.1016/j.ahj.2010.03.036. PMID: 20569734.
- Hoogsteen J, Hoogeveen A, Schaffers H, Wijn PF, van der Wall EE. Left atrial and ventricular dimensions in highly trained cyclists. Int J Cardiovasc Imaging. 2003 Jun;19(3):211-7. doi: 10.1023/a:1023684430671. PMID: 12834157.
- Coumel P. Autonomic influences in atrial tachyarrhythmias. J Cardiovasc Electrophysiol. 1996 Oct;7(10):999-1007. doi: 10.1111/j.1540-8167.1996.tb00474.x. PMID: 8894942.
- Furlanello F, Bertoldi A, Dallago M, Galassi A, Fernando F, Biffi A, Mazzone P, Pappone C, Chierchia S. Atrial fibrillation in elite athletes. J Cardiovasc Electrophysiol. 1998 Aug;9(8 Suppl):S63-8. PMID: 9727678.
- Estes NA 3rd, Link MS, Cannom D, Naccarelli GV, Prystowsky EN, Maron BJ, Olshansky B; Expert Consensus Conference on Arrhythmias in the Athlete of the North American Society of Pacing and Electrophysiololgy. Report of the NASPE policy conference on arrhythmias and the athlete. J Cardiovasc Electrophysiol. 2001 Oct;12(10):1208-19. doi: 10.1046/j.1540-8167.2001.01208.x. PMID: 11699538.
- Coumel P. Atrial fibrillation: one more sporting inconvenience? Eur Heart J. 2002 Mar;23(6):431-3. doi: 10.1053/euhj.2001.3019. PMID: 11863343.
- Hoogsteen J, Schep G, Van Hemel NM, Van Der Wall EE. Paroxysmal atrial fibrillation in male endurance athletes. A 9-year follow up. Europace. 2004 May;6(3):222-8. doi: 10.1016/j.eupc.2004.01.004. PMID: 15121075.
- Pelliccia A, Maron BJ, Di Paolo FM, Biffi A, Quattrini FM, Pisicchio C, Roselli A, Caselli S, Culasso F. Prevalence and clinical significance of left atrial remodeling in competitive athletes. J Am Coll Cardiol. 2005 Aug 16;46(4):690-6. doi: 10.1016/j.jacc.2005.04.052. PMID: 16098437.
- Opondo MA, Aiad N, Cain MA, Sarma S, Howden E, Stoller DA, Ng J, van Rijckevorsel P, Hieda M, Tarumi T, Palmer MD, Levine BD. Does High-Intensity Endurance Training Increase the Risk of Atrial Fibrillation? A Longitudinal Study of Left Atrial Structure and Function. Circ Arrhythm Electrophysiol. 2018 May;11(5):e005598. doi: 10.1161/CIRCEP.117.005598. PMID: 29748195; PMCID: PMC5951393.
- Gjerdalen GF, Hisdal J, Solberg EE, Andersen TE, Radunovic Z, Steine K. Atrial Size and Function in Athletes. Int J Sports Med. 2015 Dec;36(14):1170-6. doi: 10.1055/s-0035-1555780. Epub 2015 Oct 28. PMID: 26509381.
- Wilhelm M, Roten L, Tanner H, Wilhelm I, Schmid JP, Saner H. Atrial remodeling, autonomic tone, and lifetime training hours in nonelite athletes. Am J Cardiol. 2011 Aug 15;108(4):580-5. doi: 10.1016/j.amjcard.2011.03.086. Epub 2011 Jun 12. PMID: 21658663.
- Schnell F, Claessen G, La Gerche A, Claus P, Bogaert J, Delcroix M, Carré F, Heidbuchel H. Atrial volume and function during exercise in health and disease. J Cardiovasc Magn Reson. 2017 Dec 18;19(1):104. doi: 10.1186/s12968-017-0416-9. PMID: 29254488; PMCID: PMC5735907.
- Wright SP, Dawkins TG, Eves ND, Shave R, Tedford RJ, Mak S. Hemodynamic function of the right ventricular-pulmonary vascular-left atrial unit: normal responses to exercise in healthy adults. Am J Physiol Heart Circ Physiol. 2021 Mar 1;320(3):H923-H941. doi: 10.1152/ajpheart.00720.2020. Epub 2020 Dec 24. Erratum in: Am J Physiol Heart Circ Physiol. 2021 Oct 1;321(4):H735. PMID: 33356960.
- Bhatt A, Flink L, Lu DY, Fang Q, Bibby D, Schiller NB. Exercise physiology of the left atrium: quantity and timing of contribution to cardiac output. Am J Physiol Heart Circ Physiol. 2021 Feb 1;320(2):H575-H583. doi: 10.1152/ajpheart.00402.2020. Epub 2020 Dec 4. PMID: 33275524.
- Reeves JT, Groves BM, Cymerman A, Sutton JR, Wagner PD, Turkevich D, Houston CS. Operation Everest II: cardiac filling pressures during cycle exercise at sea level. Respir Physiol. 1990 May-Jun;80(2-3):147-54. doi: 10.1016/0034-5687(90)90078-d. PMID: 2218096.
- Chen YC, Voskoboinik A, Gerche A, Marwick TH, McMullen JR. Prevention of Pathological Atrial Remodeling and Atrial Fibrillation: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021 Jun 8;77(22):2846-2864. doi: 10.1016/j.jacc.2021.04.012. PMID: 34082914.
- Oláh A, Barta BA, Sayour AA, Ruppert M, Virág-Tulassay E, Novák J, Varga ZV, Ferdinandy P, Merkely B, Radovits T. Balanced Intense Exercise Training Induces Atrial Oxidative Stress Counterbalanced by the Antioxidant System and Atrial Hypertrophy That Is Not Associated with Pathological Remodeling or Arrhythmogenicity. Antioxidants (Basel). 2021 Mar 15;10(3):452. doi: 10.3390/antiox10030452. PMID: 33803975; PMCID: PMC7999710.
- Neri Serneri GG, Boddi M, Modesti PA, Cecioni I, Coppo M, Padeletti L, Michelucci A, Colella A, Galanti G. Increased cardiac sympathetic activity and insulin-like growth factor-I formation are associated with physiological hypertrophy in athletes. Circ Res. 2001 Nov 23;89(11):977-82. doi: 10.1161/hh2301.100982. PMID: 11717153.
- Bernardo BC, Ooi JYY, Weeks KL, Patterson NL, McMullen JR. Understanding Key Mechanisms of Exercise-Induced Cardiac Protection to Mitigate Disease: Current Knowledge and Emerging Concepts. Physiol Rev. 2018 Jan 1;98(1):419-475. doi: 10.1152/physrev.00043.2016. PMID: 29351515.
- Mihm MJ, Yu F, Carnes CA, Reiser PJ, McCarthy PM, Van Wagoner DR, Bauer JA. Impaired myofibrillar energetics and oxidative injury during human atrial fibrillation. Circulation. 2001 Jul 10;104(2):174-80. doi: 10.1161/01.cir.104.2.174. PMID: 11447082.
- Dudley SC Jr, Hoch NE, McCann LA, Honeycutt C, Diamandopoulos L, Fukai T, Harrison DG, Dikalov SI, Langberg J. Atrial fibrillation increases production of superoxide by the left atrium and left atrial appendage: role of the NADPH and xanthine oxidases. Circulation. 2005 Aug 30;112(9):1266-73. doi: 10.1161/CIRCULATIONAHA.105.538108. PMID: 16129811.
- Engelmann MD, Svendsen JH. Inflammation in the genesis and perpetuation of atrial fibrillation. Eur Heart J. 2005 Oct;26(20):2083-92. doi: 10.1093/eurheartj/ehi350. Epub 2005 Jun 23. PMID: 15975993.
- Thomas L, Abhayaratna WP. Left Atrial Reverse Remodeling: Mechanisms, Evaluation, and Clinical Significance. JACC Cardiovasc Imaging. 2017 Jan;10(1):65-77. doi: 10.1016/j.jcmg.2016.11.003. PMID: 28057220.
- Opacic D, van Bragt KA, Nasrallah HM, Schotten U, Verheule S. Atrial metabolism and tissue perfusion as determinants of electrical and structural remodelling in atrial fibrillation. Cardiovasc Res. 2016 Apr 1;109(4):527-41. doi: 10.1093/cvr/cvw007. Epub 2016 Jan 19. PMID: 26786160.
- Lenski M, Schleider G, Kohlhaas M, Adrian L, Adam O, Tian Q, Kaestner L, Lipp P, Lehrke M, Maack C, Böhm M, Laufs U. Arrhythmia causes lipid accumulation and reduced glucose uptake. Basic Res Cardiol. 2015;110(4):40. doi: 10.1007/s00395-015-0497-2. Epub 2015 May 28. PMID: 26018791.
- Sun DM, Yuan X, Wei H, Zhu SJ, Zhang P, Zhang SJ, Fan HG, Li Y, Zheng Z, Liu XC. Impaired myocardium energetics associated with the risk for new-onset atrial fibrillation after isolated coronary artery bypass graft surgery. Coron Artery Dis. 2014 May;25(3):224-9. doi: 10.1097/MCA.0000000000000081. PMID: 24463787.
- 88A. Lessan N, Ali T. Energy Metabolism and Intermittent Fasting: The Ramadan Perspective. Nutrients. 2019 May 27;11(5):1192. doi: 10.3390/nu11051192. PMID: 31137899; PMCID: PMC6566767.
- 88B. Shephard RJ. Physical performance and training response during Ramadan observance, with particular reference to protein metabolism. Br J Sports Med. 2012 Jun;46(7):477-84. doi: 10.1136/bjsports-2011-090849. Epub 2012 May 25. PMID: 22554842.
- 89. Heitmann KA, Løchen ML, Stylidis M, Hopstock LA, Schirmer H, Morseth B. Associations between physical activity, left atrial size and incident atrial fibrillation: the Tromsø Study 1994-2016. Open Heart. 2022 Jan;9(1):e001823. doi: 10.1136/openhrt-2021-001823. PMID: 35074937; PMCID: PMC8788327.
- Ricci C, Gervasi F, Gaeta M, Smuts CM, Schutte AE, Leitzmann MF. Physical activity volume in relation to risk of atrial fibrillation. A non-linear meta-regression analysis. Eur J Prev Cardiol. 2018 May;25(8):857-866. doi: 10.1177/2047487318768026. Epub 2018 Mar 29. PMID: 29591534.
- Andersen K, Farahmand B, Ahlbom A, Held C, Ljunghall S, Michaëlsson K, Sundström J. Risk of arrhythmias in 52 755 long-distance cross-country skiers: a cohort study. Eur Heart J. 2013 Dec;34(47):3624-31. doi: 10.1093/eurheartj/eht188. Epub 2013 Jun 11. PMID: 23756332..
- Abdulla J, Nielsen JR. Is the risk of atrial fibrillation higher in athletes than in the general population? A systematic review and meta-analysis. Europace. 2009 Sep;11(9):1156-9. doi: 10.1093/europace/eup197. Epub 2009 Jul 24. PMID: 19633305.
- Myrstad M, Løchen ML, Graff-Iversen S, Gulsvik AK, Thelle DS, Stigum H, Ranhoff AH. Increased risk of atrial fibrillation among elderly Norwegian men with a history of long-term endurance sport practice. Scand J Med Sci Sports. 2014 Aug;24(4):e238-44. doi: 10.1111/sms.12150. Epub 2013 Nov 21. PMID: 24256074; PMCID: PMC4282367.
- Elliott AD, Linz D, Mishima R, Kadhim K, Gallagher C, Middeldorp ME, Verdicchio CV, Hendriks JML, Lau DH, La Gerche A, Sanders P. Association between physical activity and risk of incident arrhythmias in 402 406 individuals: evidence from the UK Biobank cohort. Eur Heart J. 2020 Apr 14;41(15):1479-1486. doi: 10.1093/eurheartj/ehz897. PMID: 31951255.
- Arem H, Moore SC, Patel A, Hartge P, Berrington de Gonzalez A, Visvanathan K, Campbell PT, Freedman M, Weiderpass E, Adami HO, Linet MS, Lee IM, Matthews CE. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015 Jun;175(6):959-67. doi: 10.1001/jamainternmed.2015.0533. PMID: 25844730; PMCID: PMC4451435.
- Mozaffarian D, Furberg CD, Psaty BM, Siscovick D. Physical activity and incidence of atrial fibrillation in older adults: the cardiovascular health study. Circulation. 2008 Aug 19;118(8):800-7. doi: 10.1161/CIRCULATIONAHA.108.785626. Epub 2008 Aug 4. PMID: 18678768; PMCID: PMC3133958.
- La Gerche A, Schmied CM. Atrial fibrillation in athletes and the interplay between exercise and health. Eur Heart J. 2013 Dec;34(47):3599-602. doi: 10.1093/eurheartj/eht265. Epub 2013 Jul 24. PMID: 23884920.
- Valenzuela PL, Morales JS, Santos-Lozano A, Saco-Ledo G, Diaz-Gonzalez L, Boraita A, Lavie CJ, Lucia A. What do we really know about the association between physical activity, sports, and atrial fibrillation? A systematic review and meta-analysis from unbiased studies. Eur J Prev Cardiol. 2022 Mar 30;29(4):e143-e148. doi: 10.1093/eurjpc/zwab073. PMID: 33948641.
- Baldesberger S, Bauersfeld U, Candinas R, Seifert B, Zuber M, Ritter M, Jenni R, Oechslin E, Luthi P, Scharf C, Marti B, Attenhofer Jost CH. Sinus node disease and arrhythmias in the long-term follow-up of former professional cyclists. Eur Heart J. 2008 Jan;29(1):71-8. doi: 10.1093/eurheartj/ehm555. Epub 2007 Dec 7. PMID: 18065754.
- Bapat A, Zhang Y, Post WS, Guallar E, Soliman EZ, Heckbert SR, Lima J, Bertoni AG, Alonso A, Nazarian S. Relation of Physical Activity and Incident Atrial Fibrillation (from the Multi-Ethnic Study of Atherosclerosis). Am J Cardiol. 2015 Sep 15;116(6):883-8. doi: 10.1016/j.amjcard.2015.06.013. Epub 2015 Jun 24. PMID: 26189040; PMCID: PMC4554984.
- Grimsmo J, Grundvold I, Maehlum S, Arnesen H. High prevalence of atrial fibrillation in long-term endurance cross-country skiers: echocardiographic findings and possible predictors--a 28-30 years follow-up study. Eur J Cardiovasc Prev Rehabil. 2010 Feb;17(1):100-5. doi: 10.1097/HJR.0b013e32833226be. PMID: 20065854.
- Myrstad M, Nystad W, Graff-Iversen S, Thelle DS, Stigum H, Aarønæs M, Ranhoff AH. Effect of years of endurance exercise on risk of atrial fibrillation and atrial flutter. Am J Cardiol. 2014 Oct 15;114(8):1229-33. doi: 10.1016/j.amjcard.2014.07.047. Epub 2014 Jul 30. PMID: 25169984.
- Myrstad M, Aarønæs M, Graff-Iversen S, Nystad W, Ranhoff AH. Does endurance exercise cause atrial fibrillation in women? Int J Cardiol. 2015 Apr 1;184:431-432. doi: 10.1016/j.ijcard.2015.03.018. Epub 2015 Mar 3. PMID: 25755060.
- Myrstad M, Aarønæs M, Graff-Iversen S, Ariansen I, Nystad W, Ranhoff AH. Physical activity, symptoms, medication and subjective health among veteran endurance athletes with atrial fibrillation. Clin Res Cardiol. 2016 Feb;105(2):154-61. doi: 10.1007/s00392-015-0898-0. Epub 2015 Jul 26. PMID: 26210772.
- Schreiner AD, Keith BA, Abernathy KE, Zhang J, Brzezinski WA. Long-Term, Competitive Swimming and the Association with Atrial Fibrillation. Sports Med Open. 2016 Dec;2(1):42. doi: 10.1186/s40798-016-0066-8. Epub 2016 Oct 17. PMID: 27753048; PMCID: PMC5067262..
- Van Buuren F, Mellwig KP, Faber L, Prinz C, Fruend A, Dahm JB, Kottmann T, Bogunovic N, Horstkotte D, Butz T, Langer C. The occurrence of atrial fibrillation in former top-level handball players above the age of 50. Acta Cardiol. 2012 Apr;67(2):213-20. doi: 10.1080/ac.67.2.2154212. PMID: 22641979.
- Woodward A, Tin Tin S, Doughty RN, Ameratunga S. Atrial fibrillation and cycling: six year follow-up of the Taupo bicycle study. BMC Public Health. 2015 Jan 21;15:23. doi: 10.1186/s12889-014-1341-6. PMID: 25604001; PMCID: PMC4311486.