More Information
Submitted: November 24, 2022 | Approved: December 01, 2022 | Published: December 02, 2022
How to cite this article: Zaoui N, Boukabous A, Bachir N, Irid N, Terki A. How to manage balloon entrapment during percutaneous coronary intervention of a calcified lesion “Case report”. J Cardiol Cardiovasc Med. 2022; 7: 100-103.
DOI: 10.29328/journal.jccm.1001142
Copyright License: © 2022 Zaoui N, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Case report; Calcified lesion; PCI complication; Device entrapment; Undeflatable balloon; Balloon dysfunction
How to manage balloon entrapment during percutaneous coronary intervention of a calcified lesion “Case report”
Nassime Zaoui*, Amina Boukabous, Nadhir Bachir, Nabil Irid and Ali Terki
Cardiology Department, Omar Yacef Draa Ben Khedda Hospital, Tizi-Ouzou Medical University, Algeria
*Address for Correspondence: Nassime Zaoui, Cardiology Department, Omar Yacef Draa Ben Khedda Hospital, Tizi-Ouzou Medical University, Algeria, Email: [email protected]
Percutaneous coronary angioplasty is a minimally invasive procedure aimed at unclogging a coronary artery with a low complication rate (with a serious complication rate of 3% to 7% and a mortality rate of 1.2%). Device entrapment during PCI is a rare but life-threatening complication that occurs in < 1% of PCIs and balloon entrapment comes second after coronary guidewires. We present the case of 68-years-old man, smoker, hypertensive and type2 diabetic that presents angina with evidence of ischemia on myocardial tomoscintigraphy and in whom the radial coronary angiography reveals a tight calcified mid LAD stenosis. During his PCI and after dilatation with an NC balloon 2.5 × 12 the latter refuses to deflate and remains trapped in the lesion with the appearance of pain and ST-elevation despite several attempts to dilute the product in the inflator and to burst it by overexpansion. Traction on the balloon resulted in the deep intubation of the guiding-catheter, which comes in contact with the trapped balloon, and the rupture of the latter’s hypotube, which remains inflated at the site of the lesion and mounted on the 0.014 guidewire. We put a second 0.014 guidewire distally in the LAD and twisted with the distal part of the first guidewire, then we introduced a second balloon 2.0 × 20 over the second guidewire until the distal part of the guiding-catheter and inflated to trap the stucked balloon. We gradually removed this emergency assembly that allowed us to retrieve the trapped balloon. The control injection revealed a thrombotic occlusion of the LAD treated by thrombectomy and anti-GPIIbIIIa followed by a DES 2.75 × 28 placement. The patient was discharged 48 hours later with a good LVEF. The possible balloon entrapment mechanisms are an acute recoil of a highly calcified lesion with compression of the incompletely deflated balloon, which seems to be the case in our patient, strangulation of the proximal balloon end by the guiding-catheter if the balloon is removed before complete deflation and break or bend of the hypotube. The solutions in case of undeflatable balloon entrapment are to dilute the product in the inflator, to burst it by overexpansion, to pierce it through a stiff guidewire (or through its other end on a Microcatheter or OTW balloon), to cut its outer part and let it empty passively, to introduce a second guide-wire and perform a Buddy-Balloon or to transfer the patient to Surgery. Material entrapment remains a rare but life-threatening complication, its eviction requires the choice of material size and gentle manipulations (small balloons in the event of a calcified lesion) and its management uses different techniques, the choice of which depends on the clinical and anatomical situation.
CTO: Chronic Total Occlusion; DES: Drug Eluting Stent; ECG: Electrocardiogram; LAD: Left Anterior Descending; LVEF: Left Ventricle Ejection Fraction; NC: Non-Compliant; OTW: Over The Wire; PCI: Percutaneous Coronary Intervention; RCA: Right Coronary Artery
Percutaneous coronary angioplasty is a minimally invasive procedure aimed at unclogging a coronary artery with most often the placement of an endoprosthesis, this technique was born in 1977 in Zurich between Dr. Andreas Grüntzig hands [1].
Thanks to the evolution of the technique, its diffusion and the improvement of the material, this technique has succeeded gradually in replacing the coronary artery bypass grafting, which is the gold standard technique in coronary pathology, at the cost of a low complication rate (with a total complication rate of 17% to 23% [2], a serious complication rate of 3% to 7% [3] and a mortality rate of 1.2% [4].
Device entrapment during PCI is a rare but life-threatening complication that occurs in less than 1% of PCIs and it concerns 1.5% of CTO PCI and consists of coronary guidewires in 0.5%, balloons in 0.2%, microcatheters in 0.2%, rotational atherectomy burrs in 0.4% and guiding catheter extension in 0.04% [5].
Complete device retrieval is achieved in 63.9% [5], the recommended sequence of steps to manage this entrapment are: pulling, trapping, snaring, plaque modification, telescoping, and surgery [6].
Patient information
De-identified patient specific information: We present the case of 68-years-old man, smoker, hypertensive and type 2 diabetic present angina with left ventricle ejection fraction (LVEF) at 59% and positive myocardial tomoscintigraphy (ischemia estimated at 20% - 25% in the anterior wall).
Clinical findings
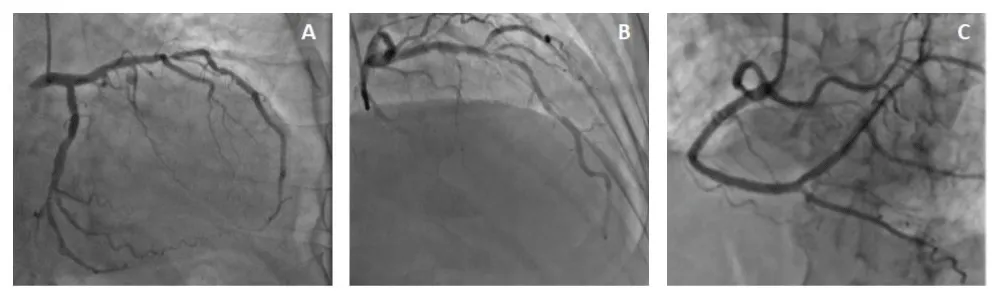
The angiography was performed by 6F right radial access, with Judkins left and right 5F diagnosis catheter. It revealed a tight calcified stenosis of the mid LAD taking the bifurcation with a small diagonal (Figure 1).
Figure 1: Angiographic finding (A: LAD stenosis in caudal view. B: LAD stenosis in cranial view. C: RCA).
Diagnostic assessment
Faced with a Syntax score of eight, we decided to perform PCI by radial access under dual antiplatelet therapy.
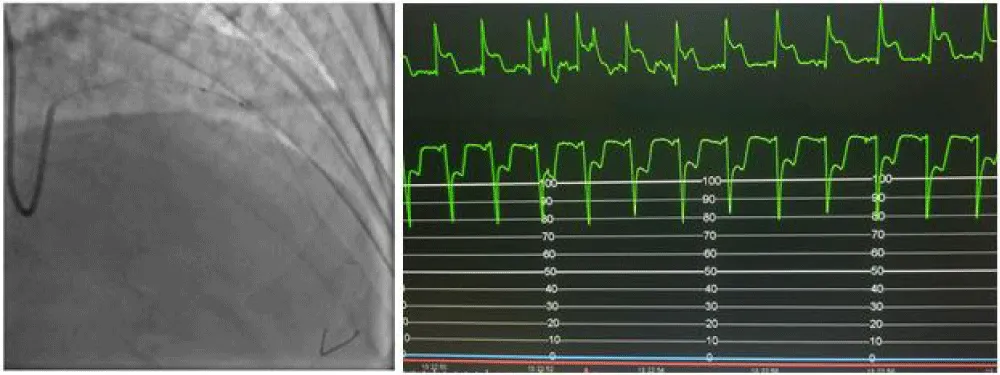
We started the procedure under 5000 UI of Heparin with an Extra Backup (EBU) 3.5 6 F guiding-catheter, we crossed the lesion with a floppy guidewire, however after dilatation with an NC balloon 2.5 × 12 the latter refuses to deflate and remains trapped in the lesion with the appearance of pain and an ST segment-elevation despite several attempts to dilute the product in the inflator and to burst it by overexpansion (Figure 2).
Figure 2: PCI and balloon trapping.
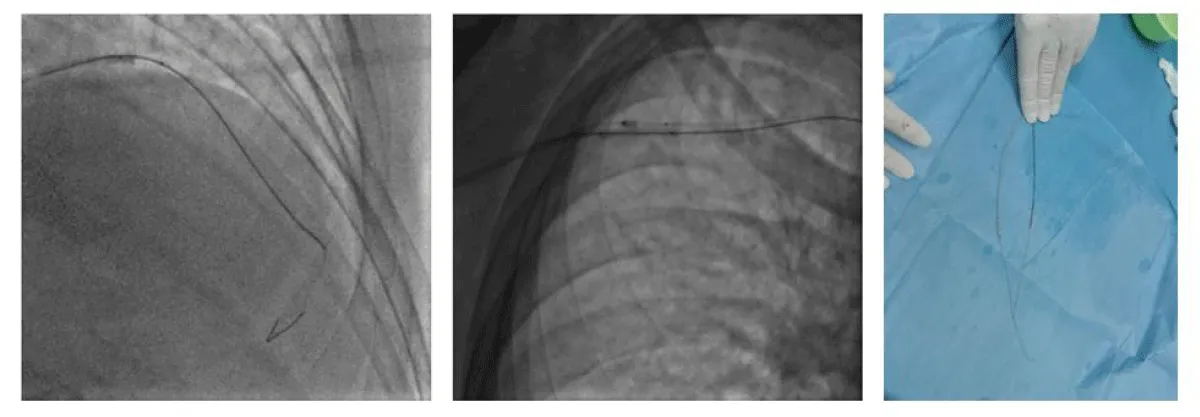
A traction on the balloon resulted in the deep intubation of the guiding-catheter which comes in contact with the trapped balloon and the rupture of the latter’s hypotube, which remains inflated at the site of the lesion partially in contact with the guiding-catheter and mounted on the 0.014 guidewire (Figure 3).
Figure 3: Rupture of the hypotube and guiding catheter deep intubation.
Therapeutic intervention
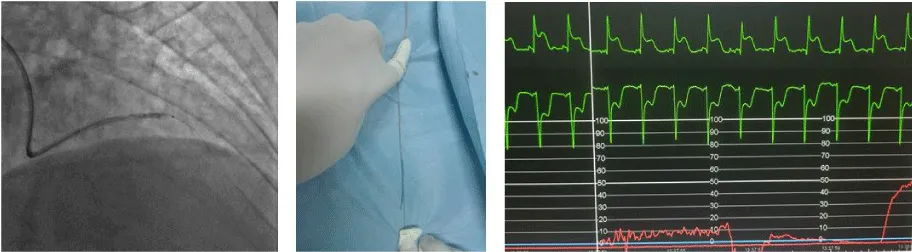
After having lost all external contact with the trapped balloon following the total rupture of its stem, we decided to introduce a second 0.014 guidewire in the LAD by taking the precaution to keep the guiding-catheter deeply intubated and in contact with the balloon.
The only guidewire that has agreed to cross between the trapped balloon and the calcified lesion was a Miracle 3 from Asahi (failure to cross with a floppy then a hydrophilic guidewire).
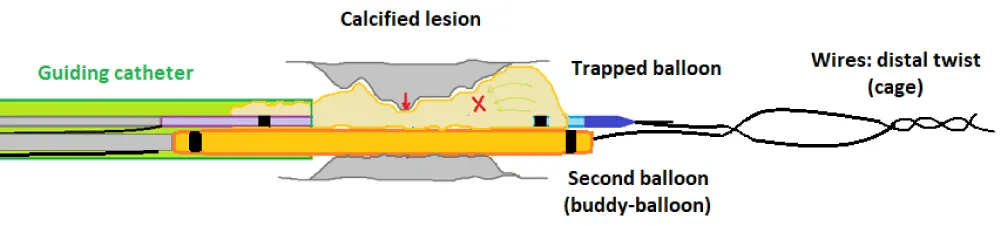
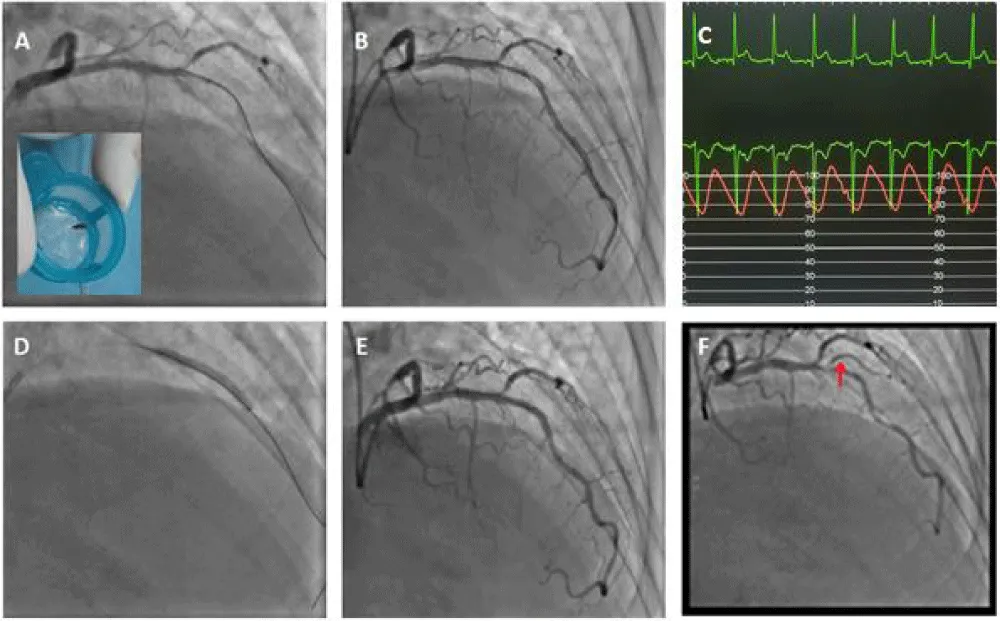
We put the second 0.014 guidewire distally in the LAD and twisted it with the distal part of the first guidewire, then we introduced a second balloon 2.0 × 20 over the second guidewire until the distal part of the guiding-catheter and inflated it between the guiding-catheter and the lesion to trap the stucked balloon between the second balloon and the guiding-catheter and to modify the lesion (to create a Cage and Buddy-balloon) (Figure 4).
Figure 4: Cage and Buddy-balloon./p>
We gradually removed this emergency assembly that allowed us to release and retrieve the trapped balloon (Figure 5). The control injection revealed a thrombotic occlusion of the LAD treated by thrombectomy and anti-GPIIbIIIa followed by a DES 2.75% 28 placement that allows a TIMI III flow in the LAD at the cost of losing the small diagonal artery that we could not recross (Figure 6).
Figure 5: Trapped balloon retrieval.
Figure 6: Management of the thrombotic occlusion of the LAD and result (A: Thrombectomy and balloon. B: result. C: ST regression. D: Stenting DES 2.75x28. E: Final result. F: Diagonal before PCI).
The patient remained stable after the procedure with normalization of his ECG and LVEF at 58% and was discharged 48 hours later.
Our technique for this patient was to create, thanks to the second 0.014 guidewire twisted with the first, what we called a cage. Associated with a buddy-balloon, that has the dual purpose of modifying the plaque using the part of the balloon inflated in the lesion, but also to trap the stucked balloon in the guiding-catheter thanks to the part of the balloon inflated in the latter.
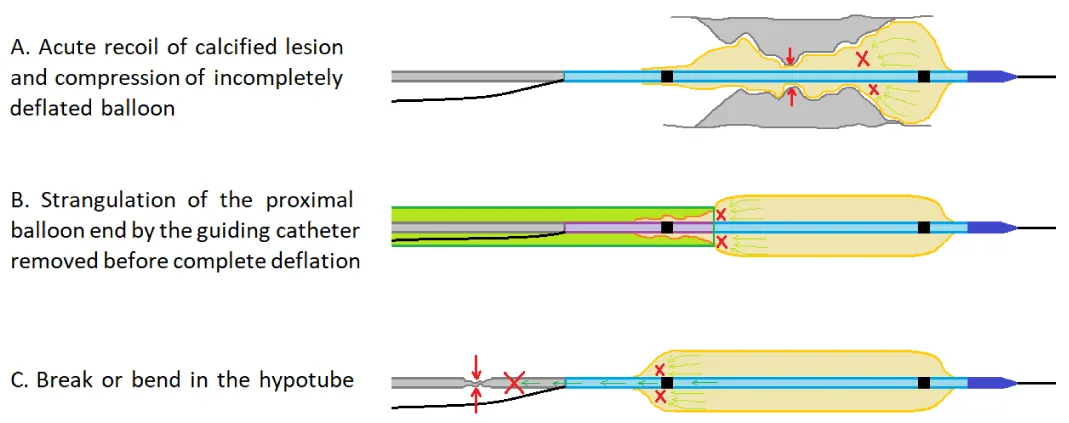
The possible balloon entrapment mechanisms are (Figure 7) [7]:
Figure 7: Balloon entrapment mechanisms.
- An acute recoil of a highly calcified lesion with compression of the incompletely deflated balloon, which seems to be the case with our patient.
- Strangulation of the proximal balloon end by the guiding-catheter if the balloon is removed before complete deflation.
- Break or bend in the hypotube.
The possible solutions in the case of undeflatable balloon entrapment are:
- To dilute the product in the inflator and redeflate.
- To burst it by overexpansion [8].
- To pierce it through a stiff guidewire (or through its other end on a Microcatheter or OTW balloon) [9].
- To cut its outer part and let it empty passively [10].
- To introduce a second guidewire and perform a Buddy-Balloon [11].
- To transfer the patient to Surgery [12].
Material entrapment remains a rare but life-threatening complication, its eviction requires the choice of material size and gentle manipulations (small balloons in the event of a calcified lesion) and its management uses different techniques, the choice of which depends on the clinical and anatomical situation.
The primary take-away lesson of this case and impact on daily practice
This case demonstrates that in-depth knowledge of the techniques and tools required can help maximize the likelihood of successful equipment retrieval and minimize complications.
It also demonstrates the interest of the technique that we have called Cage (and Buddy-wire) to recover a material from which all external contact is lost.
Learning objectives
- To know different techniques to manage balloon entrapment.
- To describe our new technique (cage) helping to retrieve any cardiac or vascular lost material.
Patient perspective
The patient says he is asymptomatic and satisfied with the impact of the angioplasty on his angina despite the painful episode during the procedure.
Informed consent
The patient consented to sharing and publishing his case and procedure images subject to anonymity.
Ethics approval and consent to participate
The patient consented to undergo the procedure.
Consent for publication>
The patient consented to the sharing and publication of data, images and results.
Availability of data and material
The images presented during this work are available from the corresponding author on reasonable request.
Authors’ contributions
NZ was responsible for realization of the percutaneous procedure and participated in the writing of the manuscript.
AB participated in the percutaneous procedure and the writing of the manuscript.
NB participated in the realization of echocardiography and in the writing of the manuscript.
AT participated in the realization of echocardiography and the follow-up of the patient during hospitalization.
NI participated in the follow-up of the patient after hospitalization.
All authors read and approved the final manuscript.
We thank our paramedics who participated in the percutaneous procedure.
Procedure videos are available on our YouTube channel: [Nassime ZAOUI].
http://www.youtube.com/channel/UCUps-8DbHFB8EN_ARUCpeZg.
- Pursnani S, Korley F, Gopaul R, Kanade P, Chandra N, Shaw RE, Bangalore S. Percutaneous coronary intervention versus optimal medical therapy in stable coronary artery disease: a systematic review and meta-analysis of randomized clinical trials. Circ Cardiovasc Interv. 2012 Aug 1;5(4):476-90. doi: 10.1161/CIRCINTERVENTIONS.112.970954. Epub 2012 Aug 7. PMID: 22872053.
- Ferreira RM, de Souza E Silva NA, Salis LHA. Complications after elective percutaneous coronary interventions: A comparison between public and private hospitals. Indian Heart J. 2018 Jan-Feb;70(1):32-36. doi: 10.1016/j.ihj.2017.06.012. Epub 2017 Jun 27. PMID: 29455784; PMCID: PMC5902824.
- Aggarwal B, Ellis SG, Lincoff AM, Kapadia SR, Cacchione J, Raymond RE, Cho L, Bajzer C, Nair R, Franco I, Simpfendorfer C, Tuzcu EM, Whitlow PL, Shishehbor MH. Cause of death within 30 days of percutaneous coronary intervention in an era of mandatory outcome reporting. J Am Coll Cardiol. 2013 Jul 30;62(5):409-15. doi: 10.1016/j.jacc.2013.03.071. Epub 2013 May 9. PMID: 23665371.
- Movahed MR, Hashemzadeh M, Jamal MM, Ramaraj R. Decreasing in-hospital mortality of patients undergoing percutaneous coronary intervention with persistent higher mortality rates in women and minorities in the United States. J Invasive Cardiol. 2010 Feb;22(2):58-60. PMID: 20124588.
- Gasparini GL, Sanz-Sanchez J, Regazzoli D, Boccuzzi G, Oreglia JA, Gagnor A, Mazzarotto P, Belli G, Garbo R. Device entrapment during percutaneous coronary intervention of chronic total occlusions: incidence and management strategies. EuroIntervention. 2021 Jun 25;17(3):212-219. doi: 10.4244/EIJ-D-20-00781. PMID: 32894229.
- Sanz-Sánchez J, Mashayekhi K, Agostoni P, Egred M, Avran A, Kalyanasundaram A, Garbo R, Colombo A, Regazzoli D, Reimers B, Brilakis ES, Gasparini GL. Device entrapment during percutaneous coronary intervention. Catheter Cardiovasc Interv. 2022 May;99(6):1766-1777. doi: 10.1002/ccd.30160. Epub 2022 Mar 21. PMID: 35312151; PMCID: PMC9544850.
- Leibundgut G, Degen C, Riede F. Transcutaneous Puncture of an Undeflatable Coronary Angioplasty Balloon Catheter. Case Rep Cardiol. 2018 Sep 3;2018:6252809. doi: 10.1155/2018/6252809. PMID: 30250754; PMCID: PMC6140099.
- Hartzler GO, Rutherford BD, McConahay DR. Retained percutaneous transluminal coronary angioplasty equipment components and their management. Am J Cardiol. 1987 Dec 1;60(16):1260-4. doi: 10.1016/0002-9149(87)90604-7. PMID: 2961239.
- Leibundgut G, Degen C, Riede F. Transcutaneous Puncture of an Undeflatable Coronary Angioplasty Balloon Catheter. Case Rep Cardiol. 2018 Sep 3;2018:6252809. doi: 10.1155/2018/6252809. PMID: 30250754; PMCID: PMC6140099.
- Watt J, Khurana A, Ahmed JM, Purcell IF. Simple Solution for an Undeflatable Stent Balloon in the Left Main Stem. JACC Cardiovasc Interv. 2015 Dec 21;8(14):e245-6. doi: 10.1016/j.jcin.2015.07.033. Epub 2015 Nov 18. PMID: 26604055.
- Chang WT, Chen JY, Li YH, Tsai LM, Lee CH. A two-case series of entrapment of a ruptured balloon in the coronary artery: Avoidable complications and nonsurgical management. J Formos Med Assoc. 2015 Nov;114(11):1135-9. doi: 10.1016/j.jfma.2013.05.008. Epub 2013 Jun 18. PMID: 23791003.
- Desai CK, Petrasko M, Steffen K, Stys T, Stys A. Retained Coronary Balloon Requiring Emergent Open Surgical Retrieval: An Uncommon Complication Requiring Individualized Management Strategies. Methodist Debakey Cardiovasc J. 2019 Jan-Mar;15(1):81-85. doi: 10.14797/mdcj-15-1-81. PMID: 31049154; PMCID: PMC6489603.