More Information
Submitted: December 30, 2022 | Approved: January 05, 2023 | Published: January 06, 2023
How to cite this article: Bisignani A, Madeo A, De Bonis S, Vico R, Bisignani G. Isolated multiple pericardial hydatid cysts in an asymptomatic patient: Role of the CMR. J Cardiol Cardiovasc Med. 2023; 8: 001-003.
DOI: 10.29328/journal.jccm.1001146
Copyright License: © 2023 Bisignani A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Isolated multiple pericardial hydatid cysts in an asymptomatic patient: Role of the CMR
Antonio Bisignani1, Andrea Madeo2* , Silvana De Bonis3, Riccardo Vico2 and Giovanni Bisignani2
, Silvana De Bonis3, Riccardo Vico2 and Giovanni Bisignani2
1Arrhythmology Unit, Fatebenefratelli Isola Tiberina, Gemelli Isola, Rome, Italy
2Department of Cardiology-ICU-Interventional Cardiology PO “Ferrari” Castrovillari (ASP Cosenza), Italy
3Department of Cardiology, PO “Giannettasio”, Rossano (ASP Cosenza), Italy
*Address for Correspondence: Andrea Madeo, Department of Cardiology-ICU-Interventional Cardiology PO “Ferrari” Castrovillari (ASP Cosenza), Italy, Email: [email protected]
Hydatid cysts primarily affect the liver and secondary involvement may be seen in almost any anatomic location.
We describe the unusual pericardial location of the Echinococcus cysts in an asymptomatic patient with suggestive cardiac magnetic resonance imaging.
Hydatid disease, caused by Echinococcus granulosus larvae, primarily affects the liver and typically demonstrates characteristic imaging findings. Furthermore, secondary involvement due to hematogenous dissemination may be seen in almost any anatomic location [1].
Cardiac hydatid cyst disease is uncommon, occurring in approximately 0.5% to 2% of patients with hydatid disease [2,3].
The most common cardiac location is myocardial, particularly the interventricular septum and left ventricular free wall, and pericardial localization is extremely unusual [4,5].
The clinical findings of pericardial hydatid cysts are nonspecific or patients may remain asymptomatic for many years, exposing patients to life-threatening complications.
In this case report we present the case of an asymptomatic patient with isolated multiple pericardial hydatid cysts and discuss the role of cardiac magnetic resonance (CMR) in the incidental diagnosis of this condition.
A 70-year-old female, farmer and asymptomatic patient underwent a routine medical check.
She was asymptomatic and her physical examination routine blood tests were unremarkable.
Electrocardiogram was normal while transthoracic echocardiography displayed roundish contiguous formations, placed on the side wall of the left ventricle.
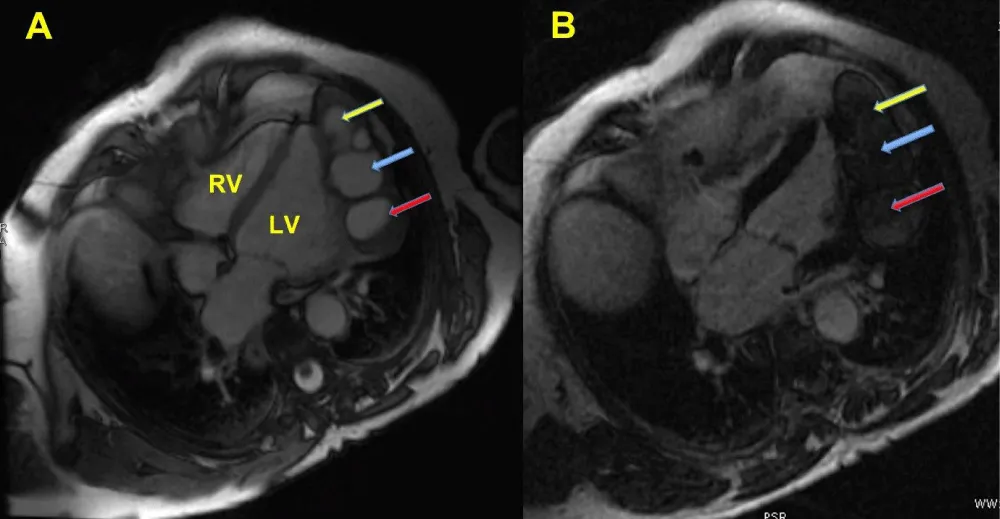
Considering the patient’s case history (farmer), it was suspected the presence of hydatid cysts. Consequently, the serologic test (hydatid cyst antibody), and enzyme-linked immunosorbent assay (ELISA) were also unremarkable and we decide to perform cardiac magnet resonance (CMR). CMR imaging evidenced three large pericardial cysts along with a smaller cyst, respectively placed on the side wall of the left ventricle (Figure 1A, Clip 1). Cysts were adherent to the pericardial visceral layer and they slightly influenced the heart sidewall movement.
On T1W1 images, the lesion appeared hypo- to iso-intense and it had no post-contrast enhancement. After the gadolinium injection, it had been displayed both the pericardial cysts’ location (without perfusion) and the mild interference on the left ventricular wall movement (Figure 1B, Clip 2).
Figure 1: A: the CMR imaging shows the pericardial location of the cysts (blu arrow) at the level of left ventricular lateral wall. CMR well depicted three large cysts and one smaller cyst (Clip 1). B: LGE shows no uptake of pericardial cysts (arrows), close to left ventricular lateral wall (Clip 2). Pericardial cysts characteristically do not enhance with administration of gadolinium.LV: Left Ventricle; RV: Right Ventricle; CMR: Cardiac Magnetic Resonance; LGE: Late Gadolinium Enhancement.
Even though the patient was asymptomatic, the cardiac hydatid cyst represented a medical emergency, due to its potential rupture especially when a pericardial location is present.
For this reason, the patient underwent successful heart surgery to remove cysts. The examination of the surgical findings confirmed the diagnosis of hydatic cysts.
The reported case is interesting because it shows multiple cysts of the pericardium, a very rare event, and because it highlights how echinococcus cysts can remain undetected and asymptomatic for years.
Hydatid disease is a parasitic infestation caused by Echinococcus granulosus larvae [6].
The infection is more frequent in some areas of the world, usually caused by the larval or cyst stage of the tapeworm Echinococcus granulosus [7].
The most frequent locations of hydatid cysts are the liver (> 65% of cases), lungs (25%) and renal (1% - 5%), but they can be seen in any location including pericardium [8].
Cardiac hydatid cyst involves particularly the interventri-cular septum and left ventricular free wall (50% - 70% of cases). Only a few cases have been reported on isolated cardiac hydatid cysts, even rarer are multiple cysts of the pericardium [9,10].
Clinical presentation of cardiac hydatid cysts depends on the location, size, number of cysts and presence of complications [1,11].
There are no age limits to the presentation and such cysts can cause obstruction in the outflow tract, valves, and chambers of the heart, and can induce conduction disturbances such as atrioventricular nodal blocks, ventricular tachycardia, fibrillation, or cardiac tamponade, or can be completely asymptomatic [12].
The cyst perforation is retained as the most dangerous complication deriving from cardiac echinococcosis (CE).
After cyst perforation, three-quarters of patients normally die of septic shock or embolic complications [13].
Diagnostic work up
A first diagnostic hint for the presence of cardiac hydatid cysts is provided by the travel, origin, and social history of the patient. Origin from the Middle East, Southern (as our case) and Eastern Europe, as well as close contact with definitive (dogs) is highly suspicious. During most of the parasitosis increased serum immunoglobulin (Ig)E and Echinococcus-specific IgE are increased during most of the CE cases. In addition, eosinophilia is detectable in about 20% - 25% of patients that suffer from CE [13]. Those antibody screening tests are particularly successful when cyst content was already hematogenous. Nevertheless, both the ELISA test and the indirect haemagglutination test (IHT) have low specificity. In seronegative patients, cardiac imaging plays a key role in diagnosing and staging CE and is sufficient to justify a drug and surgical treatment. Transthoracic echocardiography (TTE) is the cornerstone for the diagnosis because is almost available everywhere, highly cost-effective, and is accurate to localize and depict the relationship of the cysts with cardiac structures. The disadvantages of TTE are the difficulty to reproduce the imaging results in follow-up studies, its dependency on the operator, and its less accuracy in tissue characterization of the cysts. Computed tomography (CT) is more useful to highlight calcified cysts while CMR seems to have slight advantages compared with conventional CT in case of cardiac manifestation of CE, due to the better depiction of liquid cysts components. In our case, the pericardial location of the cysts made CMR crucial in diagnosis and planning treatment strategy [14]. The role of CMR is discussed below.
The role of CMR
CMR is the ideal diagnostic tool for the assessment of the pericardium and pericardial masses. It improves the detection of cardiac masses, particularly paracardiac masses [15,16]. CMR provides multiplanar imaging with a wide field of view, high spatial and temporal resolutions, and high intrinsic soft tissue contrast without the need for ionizing radiation or iodinated contrast. Specific sequences allow for different tissue weightings and intravenous contrast can be applied for further insight into the internal composition of the mass [17]. On CMR imaging, pericardial cysts are seen as homogenous, thin-walled, well-outlined masses with characteristic low to intermediate signal intensity on T1-weighted sequences and high intensity on T2-weighted sequences [18,19]. However, cysts with a hemorrhagic component or elevated protein levels may show medium or high signal intensity on T1-weighted sequences [20]. Pericardial cysts characteristically do not enhance with the administration of gadolinium [21].
It may provide precise information for the surgeon with high precision and accuracy, especially for the internal structure of the pericardial lesions [22,23].
Our case demonstrates an unusual pericardial location of echinococcus cysts incidentally diagnosed by echo-cardiography in an asymptomatic patient. Although TTE is considered the first-line diagnostic tool, often it may not be well visualized pericardial masses or cysts. In this case, it showed roundish contiguous formations placed on the lateral wall of the left ventricle while CMR better delineate the exact site of the cysts and better depicted the interference on the cardiac function.
- Hecht F, Beals RK. "New" syndrome of congenital contractural arachnodactyly originally described by Marfan in 1896. Pediatrics. 1972 Apr;49(4):574-9. PMID: 4552107.
- Dietz HC, Cutting GR, Pyeritz RE, Maslen CL, Sakai LY, Corson GM, Puffenberger EG, Hamosh A, Nanthakumar EJ, Curristin SM, et al. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature. 1991 Jul 25;352(6333):337-9. doi: 10.1038/352337a0. PMID: 1852208.
- Dietz H, Francke U, Furthmayr H, Francomano C, De Paepe A, Devereux R, Ramirez F, Pyeritz R. The question of heterogeneity in Marfan syndrome. Nat Genet. 1995 Mar;9(3):228-31. doi: 10.1038/ng0395-228. PMID: 7773282.
- Faivre L, Collod-Beroud G, Adès L, Arbustini E, Child A, Callewaert BL, Loeys B, Binquet C, Gautier E, Mayer K, Arslan-Kirchner M, Grasso M, Beroud C, Hamroun D, Bonithon-Kopp C, Plauchu H, Robinson PN, De Backer J, Coucke P, Francke U, Bouchot O, Wolf JE, Stheneur C, Hanna N, Detaint D, De Paepe A, Boileau C, Jondeau G. The new Ghent criteria for Marfan syndrome: what do they change? Clin Genet. 2012 May;81(5):433-42. doi: 10.1111/j.1399-0004.2011.01703.x. Epub 2011 Jun 2. PMID: 21564093.
- Loeys BL, Dietz HC, Braverman AC, Callewaert BL, De Backer J, Devereux RB, Hilhorst-Hofstee Y, Jondeau G, Faivre L, Milewicz DM, Pyeritz RE, Sponseller PD, Wordsworth P, De Paepe AM. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010 Jul;47(7):476-85. doi: 10.1136/jmg.2009.072785. PMID: 20591885.
- Higurashi M, Oda M, Iijima K, Iijima S, Takeshita T, Watanabe N, Yoneyama K. Livebirth prevalence and follow-up of malformation syndromes in 27,472 newborns. Brain Dev. 1990;12(6):770-3. doi: 10.1016/s0387-7604(12)80004-0. PMID: 2092586.
- Grimes SJ, Acheson LS, Matthews AL, Wiesner GL. Clinical consult: Marfan syndrome. Prim Care. 2004 Sep;31(3):739-42, xii. doi: 10.1016/j.pop.2004.04.005. PMID: 15331256.
- Chan YC, Ting CW, Ho P, Poon JT, Cheung GC, Cheng SW. Ten-year epidemiological review of in-hospital patients with Marfan syndrome. Ann Vasc Surg. 2008 Sep;22(5):608-12. doi: 10.1016/j.avsg.2008.04.005. Epub 2008 Jun 17. PMID: 18562163.
- Nollen GJ, Groenink M, Tijssen JG, Van Der Wall EE, Mulder BJ. Aortic stiffness and diameter predict progressive aortic dilatation in patients with Marfan syndrome. Eur Heart J. 2004 Jul;25(13):1146-52. doi: 10.1016/j.ehj.2004.04.033. PMID: 15231373.
- Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax. 1968 Jul;23(4):338-9. doi: 10.1136/thx.23.4.338. PMID: 5664694; PMCID: PMC471799.
- Januzzi JL, Isselbacher EM, Fattori R, Cooper JV, Smith DE, Fang J, Eagle KA, Mehta RH, Nienaber CA, Pape LA; International Registry of Aortic Dissection (IRAD). Characterizing the young patient with aortic dissection: results from the International Registry of Aortic Dissection (IRAD). J Am Coll Cardiol. 2004 Feb 18;43(4):665-9. doi: 10.1016/j.jacc.2003.08.054. PMID: 14975480.
- Grimes SJ, Acheson LS, Matthews AL, Wiesner GL. Clinical consult: Marfan syndrome. Prim Care. 2004 Sep;31(3):739-42, xii. doi: 10.1016/j.pop.2004.04.005. PMID: 15331256.
- Silverman DI, Burton KJ, Gray J, Bosner MS, Kouchoukos NT, Roman MJ, Boxer M, Devereux RB, Tsipouras P. Life expectancy in the Marfan syndrome. Am J Cardiol. 1995 Jan 15;75(2):157-60. doi: 10.1016/s0002-9149(00)80066-1. PMID: 7810492.
- Pyeritz RE. Marfan syndrome: 30 years of research equals 30 years of additional life expectancy. Heart. 2009 Mar;95(3):173-5. doi: 10.1136/hrt.2008.160515. Epub 2008 Nov 10. PMID: 19001001.
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schäfers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012 Oct;33(19):2451-96. doi: 10.1093/eurheartj/ehs109. Epub 2012 Aug 24. PMID: 22922415.
- David TE, Feindel CM. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg. 1992 Apr;103(4):617-21; discussion 622. PMID: 1532219.
- Gao L, Zhou X, Zhang L, Wen D, Chang Q, Wu Y, Sun L, Hui R. Factors influencing prognosis in patients with marfan syndrome after aortic surgery. J Cardiothorac Vasc Anesth. 2011 Aug;25(4):625-31. doi: 10.1053/j.jvca.2010.11.019. Epub 2011 Jan 22. PMID: 21262573.
- Milewicz DM, Dietz HC, Miller DC. Treatment of aortic disease in patients with Marfan syndrome. Circulation. 2005 Mar 22;111(11):e150-7. doi: 10.1161/01.CIR.0000155243.70456.F4. PMID: 15781745.