More Information
Submitted: April 10, 2023 | Approved: August 22, 2023 | Published: August 23, 2023
How to cite this article: Elisabeth D, Anne S, Alexandra D. Pneumopericardium: A Rare Complication of Antireflux Surgery. J Cardiol Cardiovasc Med. 2023; 8: 104-107.
DOI: 10.29328/journal.jccm.1001161
Copyright License: © 2023 Elisabeth D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pneumopericardium; Gastro pericardial fistula; Nissen fundoplication
Pneumopericardium: A Rare Complication of Antireflux Surgery
Diquas Elisabeth1, Druez Anne2 and Dili Alexandra1*
1Department of Surgery, University Hospital of UCLouvain-Namur, Site of Godinne, Yvoir, Belgium
2Department of Gastroenterology, University Hospital of UCLouvain-Namur, Site of Godinne, Yvoir, Belgium
*Address for Correspondence: Dili Alexandra, Department of Surgery, University Hospital of UCLouvain-Namur, Site of Godinne, Avenue G. Therasse 1, 5530 Yvoir, Belgium, Email: [email protected]
Pneumopericardium is a rare clinical entity, occurring in the setting of thoracic trauma, malignancies, or mechanical ventilation. Very few cases report pneumopericardium as a complication of gastrointestinal tract surgery. Signs and symptoms may be frustrating, ranging from asymptomatic to chest pain, sepsis, hemodynamic instability, pericarditis, or even cardiac tamponade. Clinical pathognomonic signs of pneumopericardium include pericardial metallic tinkling friction rub and mill wheel murmur. Diagnostic work-up includes electrocardiogram, chest radiography, and, computed tomography imaging. A gastro pericardial fistula should be considered a rare differential diagnosis for acute chest pain in patients with a history of gastroesophageal surgery. Rapid recognition and treatment avoid life-threatening complications. The successful outcome of gastro pericardial fistula treatment depends on both emergency and definitive surgical management. The survival rate with conservative management is poor.
We present the case of a 78-year-old patient suffering from pneumopericardium and pericardial infusion, due to a fibrotic fistula between the Nissen’s valve, occurring 10 years after redo antireflux surgery. Treatment included broad-spectrum antibiotics, and emergency surgery for pericardial drainage, biopsy of the valve’s defect, suture, and omentoplasty.
Pneumopericardium is defined as the presence of air in the pericardial cavity. Bricheteau first described this rare entity in 1844 [1-3]. He discovered a sign in a patient with hydro pneumopericardium that since then has been considered as pathognomonic of this entity, the bruit de moulin (mill wheel murmur), consisting of a fluctuating precordial sound, although it usually appears only in cases of complicated pneumopericardium [3].
The etiology of pneumopericardium is classified into two main groups: traumatic and non-traumatic. The causes of traumatic pneumopericardium are multiple and varied, with open or closed traumas presenting the highest incidence [3]. The most representative non-traumatic pneumopericardium causes include severe asthma, esophageal ulcers, neoplasms, and spontaneous esophageal rupture [3].
Few cases report pneumopericardium as a complication of gastrointestinal tract surgery.
Rapid recognition and treatment of this pathology are essential to avoid serious conditions. We present the case of pneumopericardium occurring 10 years after redo antireflux surgery.
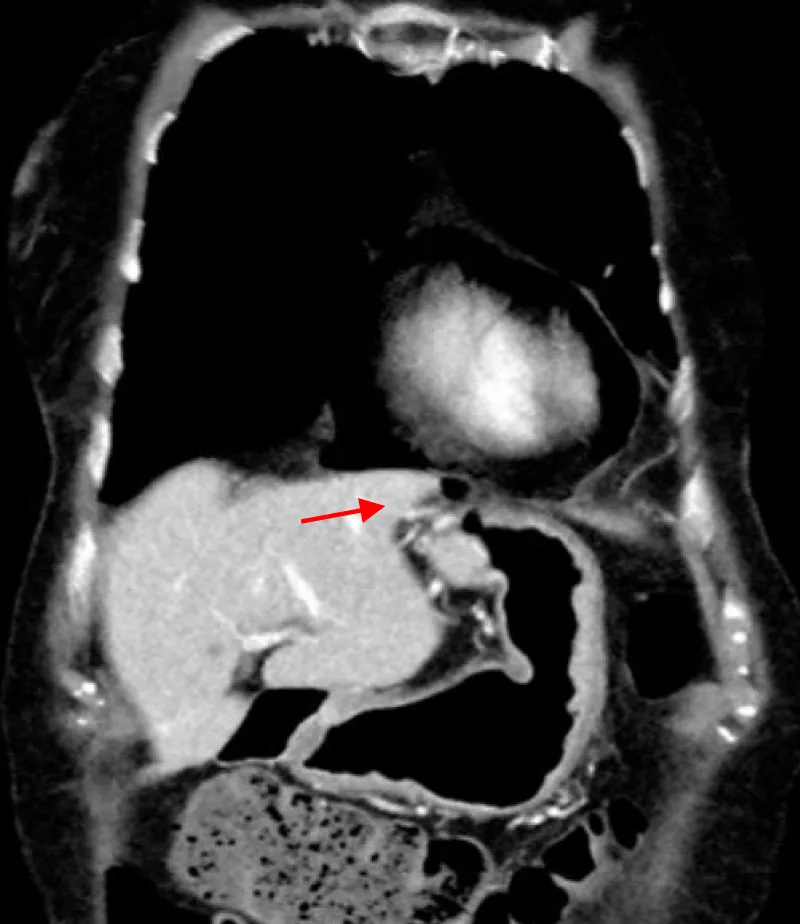
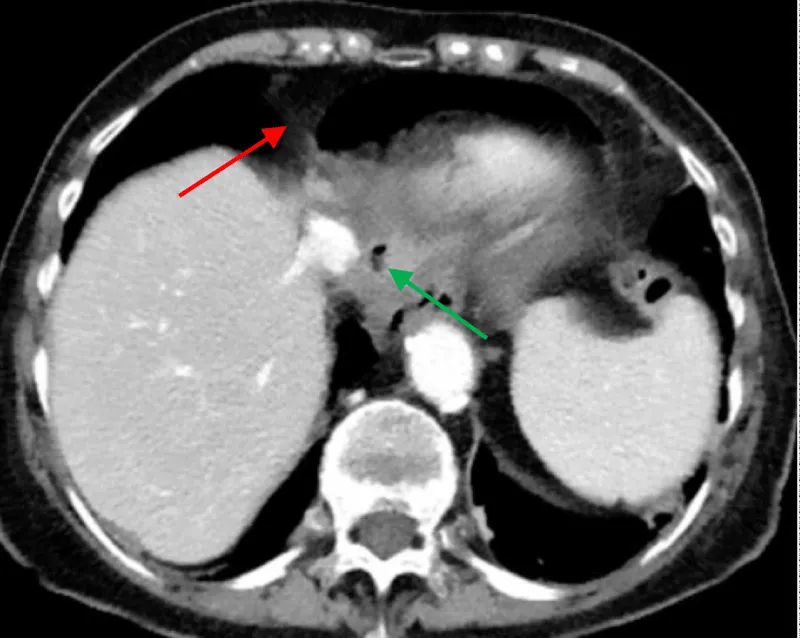
The approval of the hospital’s ethics committee was obtained to present the following case. A 78-year-old female patient was admitted to our hospital with complaints of recurring epigastric pain and diarrhea. The clinical workup revealed collagenous colitis. Upper GI endoscopy was normal. Her medical history included gastroesophageal reflux treated by Nissen fundoplication in 1980 with redo surgery in 2010. While hospitalized, she presented acute retrosternal and epigastric pain not responding to usual medication. Clinical evaluation revealed hemodynamic stability, pericardial metallic tinkling friction rub, mill wheel murmur, and no signs of peritonism. Blood analysis showed a slight inflammation while high-sensitive troponin dosage and leukocytosis were within normal range. Radiologic evaluation by CT scan revealed pneumopericardium associated with a fistula path going from the Nissen’s fundoplication valve towards the pericardial cavity (Figures 1,2).
Figure 1: CT scan showing fistula’s path (red arrow)./p>
Figure 2: CT scan showing pneumopericardium (red arrow) and pathologically edematous Nissen’s valve (green arrow).
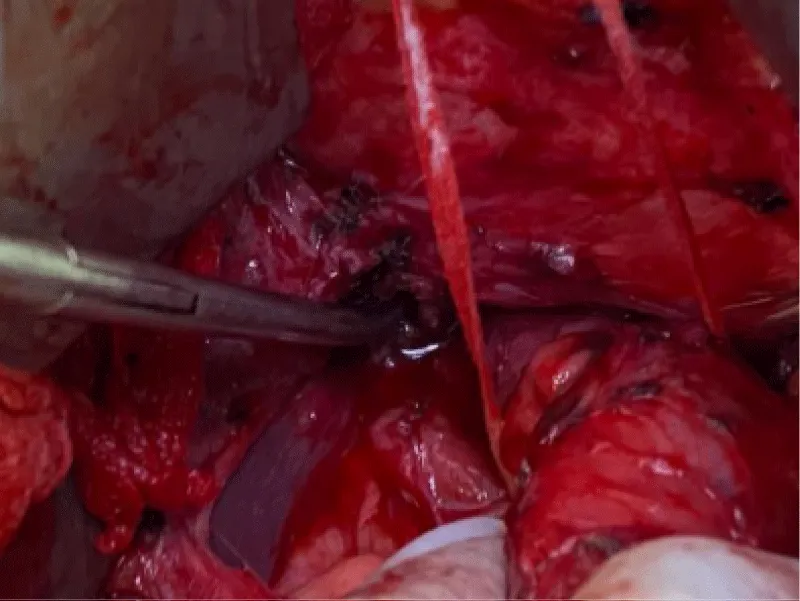
Broad-spectrum antibiotics were initiated, and the patient was quickly addressed to the operating room for surgical exploration. A fibrotic fistula between the Nissen’s valve and the pericardium, complicated with pericardial infusion, was observed. There was no ulcer macroscopically identified. Treatment included pericardial drainage, biopsy of the valve’s defect excluding ulcus and neoplasia, gastric suture, and omentoplasty. Post-operative recovery was marked by atrial fibrillation and early dysphagia linked to lower esophagus oedema resolved by the administration of glucocorticoids (Figure 3).
Figure 3: Perioperative view showing fistula’s path.
Gastropericardial fistula is a rare and highly morbid condition associated with high mortality rates of up to 50%, first described in 1844 by Bricheteau [1,2].
Operative management has contributed to a statistically significant reduction in mortality from 69 % in the pre-2000 era to 11% in the post-2000 era [4].
In a recent review, Hamid and co-authors identified 95 cases of gastro pericardial fistula (mean age 54 years, range 1-82). They observed that fistulas originated from the stomach (46%), oesophagus (38%), colon (11%), jejunum (2%), and duodenum (1%) [5].
Previous esophagogastric surgery is the most common risk factor accounting for 47% of all reported cases (including transthoracic esophagectomy, Roux-en-Y gastric bypass, and more commonly Nissen fundoplication) [2]. Antireflux surgery accounts for 14,7% of reported gastro pericardial fistulas [5].
The Pubmed database was searched for cases of gastro pericardial fistula with a history of Nissen fundoplication. The following terms have been used: “gastro pericardial” added with “fistula”; and “pneumopericardium added with “fundoplication”. In the first research, the results were too broad and cases non-presenting Nissen fundoplication in patient’s medical history were deleted. Following this search, twenty cases of gastro pericardial fistula occurring after Nissen fundoplication have been reported [1,2,8-23]. There were 10 men and 10 women. The mean age was 55 years old (ranging from 29 to 77 years old). The mean time of pneumopericardium occurrence after Nissen fundoplication is highly variable, from the 5th postoperative day to 16 years.
Of the twenty patients, 18 survived and were discharged, two died three weeks after surgery. The last two patient’s survival is unknown.
Of the twenty patients, none received conservative treatment. Three of the twenty cases benefited from initial pericardial drainage, followed by surgery (three days later for one, ten days later for the other two) [17,21].
In the majority of cases (17/20), the surgery consists of excision of the fistula, repair of the stomach, and drainage.
In two cases, due to the uncertainty of the success of a primary repair, a Malecote catheter was placed in the gastric perforation, which was closed tightly around the tube using interrupted sutures [15]. The catheter was then brought under the diaphragm and out the anterior abdominal wall as a controlled fistula similar to a gastrostomy [15]. This drain was removed 1 month after surgery [15].
Of the twenty cases, several different approaches were identified, the most common being thoracotomy (10/17), two of which were associated with laparotomy.
The pathophysiology of gastro pericardial fistula remains unclear [2]. Possible pathophysiologic mechanisms include previous gastroesophageal surgery, peptic ulceration usually associated with hiatal hernia, trauma, infection, malignancy, presence of a foreign body both ingested and/or implanted, caustic agent ingestion, or a combination of the above.
In the context of anti-reflux surgery, postoperative scar tissue, gastric fundus abnormal adhesions, and disruption of the normal curvature of the stomach are pathologic conditions offering a pathway for benign ulcers to erode into the adjacent organ. Indeed, gastric ulcers, a slipped wrap, or a para esophageal/hiatal hernia are the most important risk factors reported [2].
Alkaline reflux, gastric distension, stitch abscess, and ischemia may be contributing factors [2].
Approximately 3% to 5% of open Nissen fundoplication procedures are complicated by gastric ulcerations and in most cases, the ulceration occurs high on the lesser curvature of the stomach, close to the fundoplication [2].
The clinical presentation of gastro pericardial fistula ranges from referred pain in the left shoulder due to diaphragmatic or pericardial irritation, heartburn, epigastric tenderness, dyspnea, vomiting, hematemesis, or melena to sepsis. Chest pain or left shoulder pain was a typical symptom in 66% of the cases [6]. Other patients suffered from dyspnea, fever, shock, and even cardiac arrest due to cardiac tamponade [6]. In the case of paucisymptomatic patients these symptoms may be present months or years earlier [6].
Clinical pathognomonic signs of pneumopericardium include pericardial metallic tinkling friction rub and mill wheel murmur [3]. Occasionally, cardiac tamponade will present with Beck’s triad (hypotension, jugular venous distension, and muffled heart sounds), associated with hypovolemic shock [7].
The diagnostic work-up should include an electro-cardiogram showing repolarization disorders such as widespread ST-segment elevation probably due to pericardial irritation. Chest radiography classically shows pneumopericardium, while computed tomography imaging reveals hydro pneumopericardium and the origin of the fistula path. Exceptionally, a water-soluble swallow study can be used, or even esophagogastroduodenoscopy, although controversial due to the potential risk of tension pneumopericardium after gastric insufflation [4].
Clinicians treating patients who have had previous oesophagogastric or diaphragmatic surgery need to be aware that symptoms of atypical chest pain, hemorrhage, GI obstruction, or even shoulder tip pain may be a sign of enteric fistula formation and refer urgently to a surgeon familiar with these complications [5].
The successful outcome of gastro pericardial fistula treatment depends on both emergency and definitive management [1]. Emergency management includes early recognition of pneumopericardium and pericardial decompression [1]. Definitive management is resection of the fistula and repair of diaphragmatic hernia [1]. The treatment of gastro pericardial fistula includes antibacterial/antifungal therapy, fluid resuscitation, nutritional support, and surgery, even in multi-morbid patients [6]. Early surgical intervention to correct the gastro pericardial fistula and to drain the pericardium is highly recommended to control infection and prevent cardiac tamponade [6]. Survival rate with conservative management is reported to be only 6% [6]. However, current advances in diagnosis and early treatment of surgical procedures and perioperative care may radically improve postoperative survival.
In our case, the fistula path was observed between the Nissen’s valve and the pericardium without signs of the valve’s abnormal position (slipping Nissen), and without ulcus formation. Large-spectrum antibiotic therapy combined with laparotomy with fistula’s path resection, suture of the gastric wall, and transperitoneal pericardial drainage was performed, with favorable postoperative outcomes.
Here, we report a rare case of gastro pericardial fistula occurring without ulcer nor slipping of the wrap Nissen’s fundoplication, the most usual factor implicated in the pathophysiologiology of this rare condition. Treatment included surgical transabdominal pericardial drainage, biopsy of the valve’s defect, suture, and omentoplasty with a favorable postoperative course. The suspicion of gastro pericardial fistula should be considered a rare differential diagnosis for acute chest pain in patients with a history of gastroesophageal surgery, even if the surgery occurred years before. Pneumocardium, as a delayed complication of antireflux surgery, is rare, and probably unrecognized. Recommended treatment includes surgical fistula correction, as conservative management is associated with a worse prognosis.
- Grandhi TM, Rawlings D, Morran CG. Gastropericardial fistula: a case report and review of literature. Emerg Med J. 2004 Sep;21(5):644-5. doi: 10.1136/emj.2003.007765. PMID: 15333561; PMCID: PMC1726431.
- Liu W, Syngal S, Zellos L. Gastropericardial fistula-induced pericarditis: an unusual consequence of GERD. Medscape J Med. 2008;10(9):205. Epub 2008 Sep 2. PMID: 19008967; PMCID: PMC2580078.
- Bianchi Pintos DM, Bergoglio H, Dours JJ, Argazùa M, Vignau C, Polo S. Cardiac auscultation in the pneumopericardium. Argentine Journal of Cardiology. 2019; 87: 65-66. http://www.scielo.org.ar/pdf/rac/v88n1/en_1850-3748-rac-88-01-69.pdf
- Azzu V. Gastropericardial fistula: getting to the heart of the matter. BMC Gastroenterol. 2016 Aug 19;16(1):96. doi: 10.1186/s12876-016-0510-8. PMID: 27542946; PMCID: PMC4992300.
- Imran Hamid U, Booth K, McManus K. Is the way to a man's heart through his stomach? Enteropericardial fistula: case series and literature review. Dis Esophagus. 2013 Jul;26(5):457-64. doi: 10.1111/j.1442-2050.2012.01373.x. Epub 2012 Jun 7. PMID: 22676713.
- Ni B, Chen YL, Lin PC, Hou YT, Ho YT, Wu MY. Gastropericardial fistula induced acute purulent pericarditis. Am J Emerg Med. 2021 Aug;46:801.e1-801.e3. doi: 10.1016/j.ajem.2021.02.006. Epub 2021 Feb 10. PMID: 33608167.
- Anand R, Brooks Md Facs SE, Puckett Y, Richmond RE, Ronaghan CA. Pneumopericardium Resulting From Blunt Thoracic Trauma. Cureus. 2020 Nov 22;12(11):e11625. doi: 10.7759/cureus.11625. PMID: 33376639; PMCID: PMC7755601.
- Sihvo EI, Räsänen JV, Hynninen M, Rantanen TK, Salo JA. Gastropericardial fistula, purulent pericarditis, and cardiac tamponade after laparoscopic Nissen fundoplication. Ann Thorac Surg. 2006 Jan;81(1):356-8. doi: 10.1016/j.athoracsur.2004.08.048. PMID: 16368406.
- [9] Pop, D., Venissac, N., Rami, L., Mouroux, J. (2007) Gastropericardial fistula after laparoscopic surgery for gastroesophageal reflux disease. Journal of thoracic and cardiovascular surgery, 133 (6), 1676-1677. http://doi.org/10.1016/j.jtcvs.2007.02.009
- Farjah F, Komanapalli CB, Shen I, Sukumar MS. Gastropericardial fistula and Candida kruzei pericarditis following laparoscopic Nissen fundoplication (gastropericardial fistula). Thorac Cardiovasc Surg. 2005 Dec;53(6):365-7. doi: 10.1055/s-2005-837705. PMID: 16311974.
- Ataya A, Zellers P, Mitchell J, Alraies MC. An unusual cause of pneumopericardium. J Am Coll Cardiol. 2012 Oct 16;60(16):e29. doi: 10.1016/j.jacc.2012.03.082. PMID: 23058319.
- Lazopoulos G, Kalogerakos P, Kampitakis E, Pavlopoulos D, Kiparakis M, Chalkiadakis G. Tension hydropneumopericardium following laparoscopic Nissen fundoplication. J Card Surg. 2016 Sep;31(9):589. doi: 10.1111/jocs.12800. Epub 2016 Jul 8. PMID: 27389076.
- Murthy S, Looney J, Jaklitsch MT. Gastropericardial fistula after laparoscopic surgery for reflux disease. N Engl J Med. 2002 Jan 31;346(5):328-32. doi: 10.1056/NEJMoa010259. PMID: 11821509.
- Hauters P, de Canniere L, Collard JM, Buysschaert M, Michel LA. Gastrodiaphragmatic fistula after transabdominal Nissen fundoplication. An unusual complication. J Clin Gastroenterol. 1990 Jun;12(3):313-5. doi: 10.1097/00004836-199006000-00017. PMID: 2362102.
- Mansour KA, Sharma J. Delayed intrathoracic rupture of herniated Nissen fundoplication: report of two cases. Ann Thorac Surg. 2003 Jun;75(6):1957-9. doi: 10.1016/s0003-4975(02)04840-3. PMID: 12822646.
- Ikard RW, Jacobs JK. Gastropericardial fistula and pericardial abscess: unusual complications of subphrenic abscess following Nissen fundoplication. South Med J. 1974 Jan;67(1):17-9. doi: 10.1097/00007611-197401000-00006. PMID: 4808980.
- de Bruyne B, Dugernier T, Goncette L, Reynaert M, Otte JB, Col J. Hydropneumopericardium with tamponade as a late complication of surgical repair of hiatus hernia. Am Heart J. 1987 Aug;114(2):444-6. doi: 10.1016/0002-8703(87)90522-9. PMID: 3604908.
- Kalder J, Köster H, Hellinger A. Gastro-pericardial fistula as an early complication after surgery for combined paraesophageal and hiatal hernia. Thorac Cardiovasc Surg. 2006 Feb;54(1):67-9. doi: 10.1055/s-2005-865903. PMID: 16485195.
- Edwards JR, Humeniuk V. Gastropericardial fistula. Aust N Z J Surg. 1996 Apr;66(4):257-9. doi: 10.1111/j.1445-2197.1996.tb01176.x. PMID: 8611135.
- Kakarala K, Edriss H, Nugent K. Gastropericardial fistula as a delayed complication of a Nissen fundoplication. Proc (Bayl Univ Med Cent). 2015 Oct;28(4):478-81. doi: 10.1080/08998280.2015.11929314. PMID: 26424947; PMCID: PMC4569230.
- Chen JS, Hal HM, Tappouni RF. Radiologic evaluation of postoperative gastropericardial fistula. Radiol Case Rep. 2015 Nov 6;9(3):952. doi: 10.2484/rcr.v9i3.952. PMID: 27186253; PMCID: PMC4861863.
- Misenheimer JA, Liu Y, Means G, Kaul P, Yeung M. Tension Pneumopericardium Secondary to Gastropericardial Fistula Presenting as Acute Pericarditis With Cardiac Tamponade Physiology. JACC Cardiovasc Interv. 2016 Aug 22;9(16):1748-9. doi: 10.1016/j.jcin.2016.05.042. PMID: 27539697.
- Schneider F, Schenk M, Tempé JD, Thiry L. Spontaneous gastropericardial fistula. Ann Emerg Med. 1995 Sep;26(3):394. doi: 10.1016/s0196-0644(95)70100-1. PMID: 7661443.