More Information
Submitted: January 22, 2024 | Approved: February 02, 2024 | Published: February 05, 2024
How to cite this article: Andishmand A, Zolfeqari E, Namayandah MS, Ghaem HM. Impact of Chronic Kidney Disease on Major Adverse Cardiac Events in Patients with Acute Myocardial Infarction: A Retrospective Cohort Study. J Cardiol Cardiovasc Med. 2024; 9: 029-034.
DOI: 10.29328/journal.jccm.1001175
Copyright License: © 2024 Andishmand A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Major adverse cardiac event; Glomerular filtration rate; Acute myocardial infarction; Chronic kidney disease
Impact of Chronic Kidney Disease on Major Adverse Cardiac Events in Patients with Acute Myocardial Infarction: A Retrospective Cohort Study
Abbas Andishmand1, Ehsan Zolfeqari1* , Mahdiah Sadat Namayandah1 and Hossein Montazer Ghaem2
, Mahdiah Sadat Namayandah1 and Hossein Montazer Ghaem2
1Yazd Cardiovascular Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2Cardiovascular Research Center, Hormozgan University of Medical Science, Bandar Abbas, Iran
*Address for Correspondence: Ehsan Zolfeqari, MD, Yazd Cardiovascular Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran, Email: [email protected]
Background: Acute Myocardial Infarction (AMI) results in a reduction in patients’ life expectancy. Different risk factors affect the risk of Major Adverse Cardiac Events (MACE). Although the role of kidney dysfunction in patients with Chronic Kidney Disease (CKD) in cardiac events has been identified, many patients with AMI are unaware of their underlying kidney disease. This study aimed to compare the incidence of adverse cardiovascular events and identify predictors of major adverse cardiovascular events in the medium term among patients with and without renal dysfunction following AMI.
Methods: This retrospective cohort study was conducted on 1039 patients who were hospitalized for Acute Myocardial Infarction (AMI) between 2018 and 2019. The patient cohort comprised 314 women (mean age: 69.8 ± 13.2 years) and 725 men (mean age: 60.5 ± 13.8 years). Patient data were obtained from the registry of patients with acute myocardial infarction and the participants were followed up for a minimum of one year following hospital discharge to assess the incidence of MACE.
Results: The study found that patients with a Glomerular Filtration Rate (GFR) level below 60 had a significantly higher mortality rate than those with a GFR level of 60 or above (15.7% vs. 3.5%, p < 0.0001). The multivariate analysis showed that Diabetes Mellitus (DM), GFR, and Non-ST Elevation Myocardial Infarction (NSTEMI) are significant risk factors for cardiovascular events. (p = 0.016, p = 0.015, p = 0.006 respectively), while variables such as sex, age, and Hypertension (HTN) were not significant risk factors. There was a negative correlation between GFR and death (0.241 - = r, p < 0.0001)
Conclusion: This study highlights the importance of detecting kidney disease during an AMI and managing risk factors for cardiovascular disease to improve health outcomes and reduce the risk of mortality.
Acute Myocardial Infarction (AMI) is a significant public health concern, representing a leading cause of morbidity and mortality worldwide. Renal impairment commonly coexists in patients with cardiovascular disease, thereby increasing the risk of major adverse cardiovascular events [1-4]. The severity of renal dysfunction serves as a vital prognostic factor for subsequent cardiovascular events [5]. Early identification of renal dysfunction is of paramount importance for optimal management, as its presence can have a negative impact on diagnostic and therapeutic interventions during both the acute and long-term phases of AMI [6,7]. Notably, patients with Chronic Kidney Disease (CKD) who experience ST-elevation myocardial infarction (STEMI) face a particularly high risk of adverse outcomes, including death, hospitalization, and cardiovascular events [8-10].
The primary objective of this study is to conduct a comprehensive comparative analysis of adverse cardiovascular events in patients with and without renal dysfunction following acute myocardial infarction. Additionally, the secondary objective is to identify the predictors of such occurrences in the medium term. By examining the relationship between renal dysfunction and cardiovascular outcomes in AMI patients, this research aims to enhance our understanding of the impact of renal impairment on the prognosis of individuals with AMI. The findings from this study hold the potential to contribute to the development of improved strategies for risk stratification, early detection and management of renal dysfunction in AMI patients. Ultimately, this could lead to better patient outcomes and potentially alleviate the burden of cardiovascular events in this population.
This retrospective cohort study included a total of 1039 patients who were admitted to Afshar Hospital between 2018 and 2019 and diagnosed with Acute Myocardial Infarction (AMI). The sample size for the study was determined based on an assumed Major Adverse Cardiovascular Events (MACE) rate of approximately 4%. With a desired level of significance (α) of 0.05 and a power (1-β) of 0.80, the sample size of 1039 patients was estimated to be sufficient to detect significant differences in MACE rates.
The study followed ethical guidelines and principles set by the institutional review board at Azad Medical School of Yazd. Ethical approval was obtained from the review board before starting the research, based on the code of ethics (1400.315.IR.IAU.KHUISF.REC) provided by the ethics committee. Informed consent was obtained from all participants, and their privacy and confidentiality were safeguarded throughout the research process.
Patient data was extracted from a registry database that included myocardial infarction patients in Yazd province. The study included patients between 25 and 70 years old who had a confirmed diagnosis of myocardial infarction according to the fourth universal definition of MI. Patients with a history of heart failure before the myocardial infarction or those who did not provide consent were excluded from the study.
The collected patient data encompassed various demographic variables such as age, gender, weight, blood pressure, diabetes, smoking status, alcohol consumption, and high blood pressure. Additionally, information on laboratory test results, symptoms at the time of referral, type and severity of myocardial infarction, and details of the treatment received were recorded. The Glomerular Filtration Rate (GFR) was calculated for each patient using the Modification of Diet in Renal Disease (MDRD) formulas. The study aimed to evaluate the impact of renal dysfunction on adverse cardiovascular events following acute myocardial infarction by comparing patients with a GFR greater than 60cc/min to those with a GFR equal to or less than 60cc/min. This cutoff point allowed for a clear differentiation between patients with relatively normal kidney function and those with impaired kidney function.
Patients were followed up for at least one year, during which occurrences of death, hospitalization, and repeat revascularization were evaluated as Major Adverse Cardiovascular Events (MACE) in the study.
The collected data were analyzed using SPSS-18 software. Quantitative data were analyzed using t-tests and ANOVA tests, while qualitative variables were analyzed using the chi-square test. Post-hoc analysis using the Tukey test was conducted when necessary. A p - value less than 0.05 was considered statistically significant, indicating meaningful differences between the groups being compared.
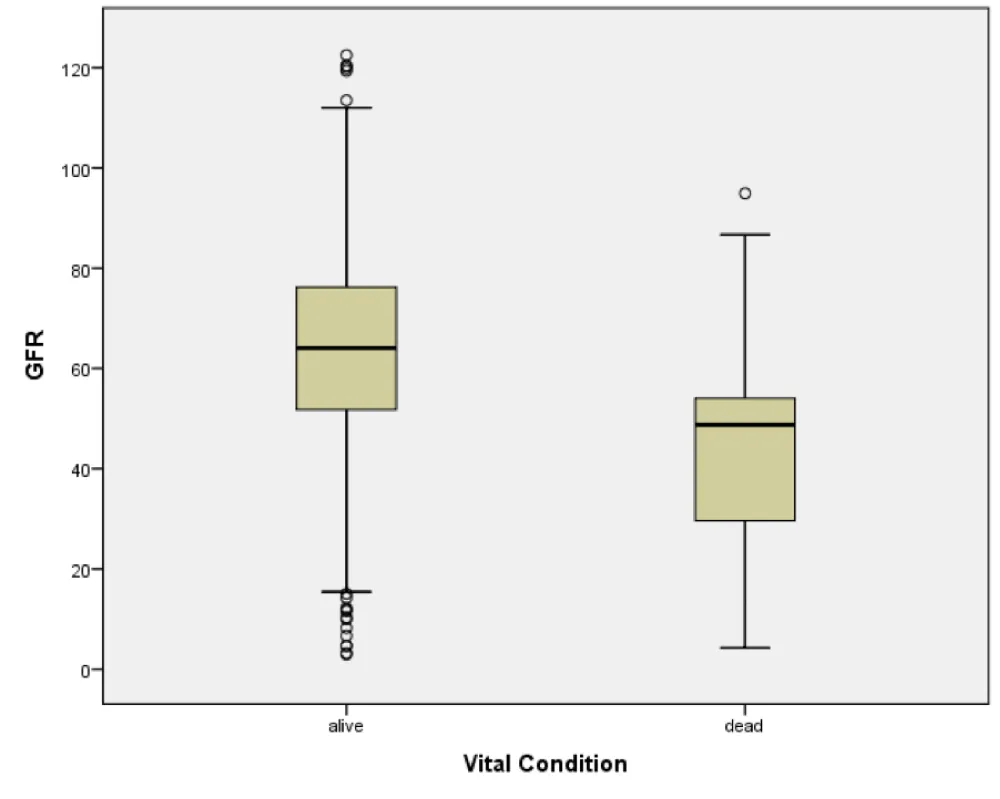
This study included a total of 314 women, with a mean age of 69.8 ± 13.2 years, and 725 men, with a mean age of 60.5 ± 13.8 years. The characteristics of the patients are presented in Table 1. The loss rate for follow-up and assessment of Major Adverse Cardiovascular Events (MACE) was 7.7%, which accounted for 80 patients. During the one-year follow-up period, 8.7% of the patients died (Table 2). The study found a significant relationship between low Glomerular Filtration Rate (GFR) levels and higher mortality rates. Patients with a GFR below 60 had a mortality rate of 15.7%, compared to 3.5% for those with a GFR of 60 or above (Table 3). Age, sex, GFR, and Diabetes Mellitus (DM) were identified as significant risk factors for MACE, while smoking, opium addiction, and Hypertension (HTN) did not show a significant association (Table 4). Patients with lower GFR levels were found to have a higher likelihood of experiencing MACE compared to those with higher GFR levels. Multivariate regression analysis revealed that DM, GFR, and Non-ST Elevation Myocardial Infarction (NSTEMI) were significant risk factors for cardiovascular events (p = 0.016, p = 0.015, p = 0.006, respectively). However, variables such as sex, age, and HTN were not significant risk factors (Table 5). There was a negative correlation between GFR and death (r = -0.241, p < 0.0001) (Figure 1).
Figure 1: Relationship between Glomerular Filtration Rate and Mortality.
| Table 1: Baseline Characteristics of Study Population. | |
| Character | Mean ± SD N(%) |
| Age (yr) -Male -Female |
13.8 ± 60.5 13.2 ± 69.8 |
| Sex -Male -Female |
725(69.8) 314(30.2) |
| BMI > = 30 kg/ m2 | 190(18.3) |
| Risk factor -DM -HTN -HLP -Smoking -Opium addiction |
352(33.9) 494(47.5) 384(37) 252(24.3) 158(15.2) |
| MI type -STEMI -NSTEMI -LBBB -undetermined |
652(62.8) 365(35.1) 9(0.9) 13(1.2) |
| Treatment option -Medical -PCI |
550(52.9) 489(47.1) |
| Table 2: Association between Glomerular Filtration Rate and Adverse Cardiovascular Outcomes. | |||
| Event | N | % | Total |
| Death | 84 | 8.7 | 959 |
| Rehospitalisation | 263 | 27.4 | 959 |
| Repeat Revascularization | 161 | 16.8 | 959 |
| MACE | 508 | 52.9 | 959 |
| MACE: Major Adverse Cardiovascular Events. | |||
| Table 3: Association between GFR Level and Patient Survival. | |||
| GFR level | Alive | Deceased (%) | p |
| ≥ 60 | 528(96.5) | 19(3.5) | < 0.0001 |
| < 60 | 347(84.3) | 65(15.7) | |
| Note: GFR: Glomerular Filtration Rate. | |||
| Table 4: Association of Risk Factors with Major Adverse Cardiovascular Events (MACE). | |||||
| Parameter | With MACE (N) | Without MACE (N) | p | ||
| ≥ 60 | < 60 | ≥ 60 | < 60 | ||
| Age ≥ 60 yr | 59 | 136 | 146 | 187 | 0.004 |
| Male | 135 | 86 | 325 | 130 | 0.034 |
| Female | 23 | 101 | 41 | 132 | |
| Smoking | 58 | 21 | 121 | 32 | 0.863 |
| Opium addiction | 40 | 16 | 77 | 25 | 0.353 |
| DM | 48 | 89 | 92 | 106 | 0.039 |
| HLP | 45 | 69 | 119 | 131 | 0.518 |
| HTN | 61 | 112 | 131 | 166 | 0.136 |
| GFR | 158 | 187 | 366 | 262 | 0.001 |
| MACE: Major Adverse Cardiovascular Events. DM: DiabeteMellitus. HLP: Hyperlipidemia. HTN: Hypertension. GFR: Glomerular Filtration Rate. | |||||
| Table 5: Multivariate Regression Analysis of Risk Factors for Cardiovascular Events. | |||||
| Variable | Regression coefficient | Odd ratio | Min | Max | p - value |
| HTN | 0.112 | 1.12 | 0.803 | 1.557 | 0.508 |
| DM | 0.379 | 1.46 | 1.072 | 1.989 | 0.016 |
| HLP | -0.469 | 0.63 | 0.449 | 0.871 | 0.005 |
| MI type STEMI vs. NSTEMI |
-0.412 | 0.66 | 0.495 | 0.887 | 0.006 |
| Sex | 0.259 | 1.3 | 0.919 | 1.825 | 0.139 |
| Age | 0.4 | 1.4 | 0.992 | 1.015 | 0.536 |
| GFR | 0.419 | 1.52 | 1.085 | 2.133 | 0.015 |
| HTN: Hypertension; DM: Diabetes Mellitus; HLP: Hyperlipidemia; STEMI: ST-Elevation Myocardial Infarction; NSTEMI: Non-ST Elevation Myocardial Infarction; RC: Risk Category; GFR: Glomerular Filtration Rate. | |||||
Chronic Kidney Disease (CKD) is a significant global health issue affecting millions of individuals worldwide [11,12]. It is a progressive condition characterized by a gradual decline in kidney function, leading to the accumulation of toxins and waste products in the body [13]. CKD is associated with an increased risk of mortality, cardiovascular disease, and other health complications [14,15]. Glomerular Filtration Rate (GFR) is a measure of kidney function that estimates the amount of blood filtered by the kidneys over time [16]. This study used the Glomerular Filtration Rate (GFR) instead of serum creatinine for assessing kidney function. GFR is a more precise measure because it reflects the kidneys’ ability to filter blood and remove waste products [17]. Serum creatinine, although commonly used, can be influenced by various factors and may not provide an accurate indicator of kidney function alone. GFR, considers additional factors such as age, sex, race, and serum creatinine levels, resulting in a more accurate estimation of kidney function, especially in individuals with Chronic Kidney Disease (CKD) or those at risk of developing it [18]. GFR is preferred in research studies due to its standardized assessment of kidney function across different populations [19]. It allows for the classification of patients into different CKD stages and the evaluation of their clinical outcomes, including mortality, cardiovascular events, and treatment response [20]. A GFR level below 60 indicates CKD and a GFR level below 15 indicates kidney failure [21]. Our study revealed a significant association between lower GFR levels and higher mortality rates. Specifically, patients with a GFR below 60 had a mortality rate of 15.7%, compared to only 3.5% in patients with a GFR of 60 or above. These findings are consistent with previous research demonstrating a link between lower GFR and increased mortality in Acute Myocardial Infarction (AMI) patients [22-27]. For instance, a study by Ismail, et al. reported a one-year mortality rate of 13.2% in patients with a GFR below 60% compared to 2.4% in those with a GFR above 60% [28].
In addition to mortality, our study investigated the risk factors associated with Major Adverse Cardiovascular Events (MACE). Age and Diabetes Mellitus (DM) were identified as significant risk factors for MACE. DM is a leading cause of CKD and is known to elevate the risk of cardiovascular disease. Interestingly, our study found an inverse relationship between hyperlipidemia and cardiovascular diseases. Further investigation is needed to explore whether statin treatment in patients with this history may provide protective effects against cardiac events. A meta-analysis indicated that statin administration resulted in a 41% reduction in cardiovascular disease risk in stages 1 - 3 CKD compared to placebo. Statins were also found to significantly reduce the risk of total mortality, coronary heart disease events, and stroke in the same patient population [29].
Studies have extensively examined AMI patients with CKD or End-Stage Renal Disease (ESRD). Renal injury in AMI patients is associated with an increased risk of mortality and CKD progression. Bleeding is the primary cause of mortality in dialysis patients with ESRD, and STEMI patients on dialysis exhibit higher in-hospital mortality rates. AMI patients with ESRD require personalized management and appropriate coronary revascularization. Impaired renal function in STEMI patients is linked to a higher mortality risk, and primary Percutaneous Coronary Intervention (PCI) yields better outcomes than fibrinolysis. These studies emphasize the importance of recognizing and managing renal injury and comorbidities in AMI patients with CKD or ESRD to improve outcomes [24,30-34]. Our study also employed multivariate regression analysis to identify risk factors associated with cardiovascular disease. The analysis revealed that DM and Non-ST Elevation Myocardial Infarction (NSTEMI) are significant risk factors for cardiovascular events. However, variables such as sex, age, and Hypertension (HTN) did not show a significant association. These findings align with previous studies that have identified DM and the type of MI as significant risk factors for cardiovascular events [24,35]. Furthermore, the study found that Percutaneous Coronary Intervention (PCI) was more frequently performed in patients with ST-Elevation Myocardial Infarction (STEMI) compared to those with NSTEMI. This difference in PCI utilization may contribute to the variation in Major Adverse Cardiovascular Event (MACE) incidence between the two groups. Studies suggest that an early invasive strategy may improve outcomes in non-ST-elevation Acute Coronary Syndrome (ACS) patients with CKD [36-38].
The findings of our study underscore the importance of managing risk factors to mitigate the risk of cardiovascular disease and enhance health outcomes. This may involve lifestyle modifications such as adopting a healthy diet, engaging in regular physical activity, and smoking cessation, as well as medication management and regular monitoring of kidney function [39,40].
The study was a retrospective analysis of patients with Chronic Kidney Disease (CKD) who had experienced an Acute Myocardial Infarction (AMI). While the study provided important insights into the management and outcomes of this patient population, several limitations had to be considered when interpreting the results.
First, the retrospective nature of the study limited the ability to establish causality or control for potential confounders. This meant that while the study could identify associations between different variables, it could not determine whether one variable directly caused another. Additionally, the study was conducted at a single center, which may have limited the generalizability of the findings to other settings. Another limitation of the study was its relatively short follow-up period of one year. This may have underestimated the incidence of long-term outcomes, such as mortality and cardiovascular events, which are important outcomes for patients with CKD and AMI. Furthermore, the study excluded patients with a history of heart failure before myocardial infarction, which may have limited the generalizability of the findings to this patient population. This was an important limitation, as heart failure is a common complication of CKD and is associated with increased morbidity and mortality. Moreover, the study did not include information on certain variables that may have impacted the outcomes, such as medication use and comorbidities. This was a significant limitation, as the management of CKD and AMI typically involves multiple medications and the presence of comorbidities can impact treatment decisions and outcomes. Finally, the study did not provide information on the specific interventions used to manage patients with CKD and AMI. This was an important limitation, as the choice of interventions can impact outcomes such as mortality and cardiovascular events.
The findings of this study demonstrate a significant association between GFR levels below 60 and increased mortality rates. Patients with lower GFR levels are more likely to experience MACE compared to those with higher GFR levels. Furthermore, GFR emerges as a crucial predictor of mortality and should be incorporated into the assessment of cardiovascular disease risk.
We are deeply grateful to the esteemed officials of the Yazd Cardiovascular Research Center, as well as the Clinical Research and Development of Afshar Hospital, who have supported us in this research.
Author contributions
Abbas Andishmand contributed to the conception and design, drafted the manuscript, gave final approval, and agreed to be accountable for all aspects of the work ensuring integrity and accuracy.
Mahdiah Sadat Namayandah contributed to analysis and interpretation, drafted the manuscript, critically revised the manuscript, gave final approval, and agreed to be accountable for all aspects of the work ensuring integrity and accuracy.
Ehsan Zolfeqari contributed to the acquisition, drafted the manuscript, and prepared and revised the manuscript.
- Smith GL, Masoudi FA, Shlipak MG, Krumholz HM, Parikh CR. Renal impairment predicts long-term mortality risk after acute myocardial infarction. J Am Soc Nephrol. 2008 Jan;19(1):141-50. doi: 10.1681/ASN.2007050554. Epub 2007 Nov 14. PMID: 18003773; PMCID: PMC2391037.
- Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW; American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003 Oct 28;108(17):2154-69. doi: 10.1161/01.CIR.0000095676.90936.80. PMID: 14581387.
- Nestelberger T, Boeddinghaus J, Wussler D, Twerenbold R, Badertscher P, Wildi K, Miró Ò, López B, Martin-Sanchez FJ, Muzyk P, Koechlin L, Baumgartner B, Meier M, Troester V, Rubini Giménez M, Puelacher C, du Fay de Lavallaz J, Walter J, Kozhuharov N, Zimmermann T, Gualandro DM, Michou E, Potlukova E, Geigy N, Keller DI, Reichlin T, Mueller C; APACE Investigators. Predicting Major Adverse Events in Patients with Acute Myocardial Infarction. J Am Coll Cardiol. 2019 Aug 20;74(7):842-854. doi: 10.1016/j.jacc.2019.06.025. PMID: 31416527.
- Chen W, Tan X, Du X, Li Q, Yuan M, Ni H, Wang Y, Du J. Prediction models for major adverse cardiovascular events following ST-segment elevation myocardial infarction and subgroup-specific performance. Front Cardiovasc Med. 2023 Apr 25; 10:1181424. doi: 10.3389/fcvm.2023.1181424. PMID: 37180806; PMCID: PMC10167292.
- Janjani P, Motevaseli S, Salehi N, Heidari Moghadam R, Siabani S, Nalini M. Predictors of 1-Year Major Cardiovascular Events after ST-Elevation Myocardial Infarction in a Specialized Cardiovascular Center in Western Iran. J Tehran Heart Cent. 2022 Apr;17(2):62-70. doi: 10.18502/jthc.v17i2.9839. PMID: 36567930; PMCID: PMC9748231.
- Sattar S, Hussain S, Aijaz S, Khan G, Akhter Z, Malik R, Ali I, Pathan A. Major adverse cardiovascular events in patients undergoing percutaneous coronary intervention or coronary artery bypass graft with underlying chronic kidney disease. J Pak Med Assoc. 2020 Nov;70(11):1901-1907. doi: 10.5455/JPMA.22790. PMID: 33341827.
- Goldberg A, Hammerman H, Petcherski S, Zdorovyak A, Yalonetsky S, Kapeliovich M, Agmon Y, Markiewicz W, Aronson D. Inhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. Am Heart J. 2005 Aug;150(2):330-7. doi: 10.1016/j.ahj.2004.09.055. PMID: 16086939.
- Fox CS, Muntner P, Chen AY, Alexander KP, Roe MT, Cannon CP, Saucedo JF, Kontos MC, Wiviott SD; Acute Coronary Treatment and Intervention Outcomes Network registry. Use of evidence-based therapies in short-term outcomes of ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction in patients with chronic kidney disease: a report from the National Cardiovascular Data Acute Coronary Treatment and Intervention Outcomes Network registry. Circulation. 2010 Jan 26;121(3):357-65. doi: 10.1161/CIRCULATIONAHA.109.865352. Epub 2010 Jan 11. PMID: 20065168; PMCID: PMC2874063.
- Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004 Sep 23;351(13):1296-305. doi: 10.1056/NEJMoa041031. Erratum in: N Engl J Med. 2008;18(4):4. PMID: 15385656.
- Herzog CA, Ma JZ, Collins AJ. Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med. 1998 Sep 17;339(12):799-805. doi: 10.1056/NEJM199809173391203. PMID: 9738087.
- Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, De Zeeuw D, Hostetter TH, Lameire N, Eknoyan G. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005 Jun;67(6):2089-100. doi: 10.1111/j.1523-1755.2005.00365.x. PMID: 15882252.
- Lv JC, Zhang LX. Prevalence and Disease Burden of Chronic Kidney Disease. Adv Exp Med Biol. 2019; 1165:3-15. doi: 10.1007/978-981-13-8871-2_1. PMID: 31399958.
- Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022 Apr;12(1):7-11. doi: 10.1016/j.kisu.2021.11.003. Epub 2022 Mar 18. PMID: 35529086; PMCID: PMC9073222.
- van der Velde M, Matsushita K, Coresh J, Astor BC, Woodward M, Levey A, de Jong P, Gansevoort RT; Chronic Kidney Disease Prognosis Consortium; van der Velde M, Matsushita K, Coresh J, Astor BC, Woodward M, Levey AS, de Jong PE, Gansevoort RT, Levey A, El-Nahas M, Eckardt KU, Kasiske BL, Ninomiya T, Chalmers J, Macmahon S, Tonelli M, Hemmelgarn B, Sacks F, Curhan G, Collins AJ, Li S, Chen SC, Hawaii Cohort KP, Lee BJ, Ishani A, Neaton J, Svendsen K, Mann JF, Yusuf S, Teo KK, Gao P, Nelson RG, Knowler WC, Bilo HJ, Joosten H, Kleefstra N, Groenier KH, Auguste P, Veldhuis K, Wang Y, Camarata L, Thomas B, Manley T. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int. 2011 Jun;79(12):1341-52. doi: 10.1038/ki.2010.536. Epub 2011 Feb 9. PMID: 21307840.
- Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular Disease in Chronic Kidney Disease: Pathophysiological Insights and Therapeutic Options. Circulation. 2021 Mar 16;143(11):1157-1172. doi: 10.1161/CIRCULATIONAHA.120.050686. Epub 2021 Mar 15. PMID: 33720773; PMCID: PMC7969169.
- Kaufman DP, Basit H, Knohl SJ. Physiology, Glomerular Filtration Rate. In: StatPearls. Treasure Island (FL): StatPearls. 2023; PMID: 29763208.
- Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function--measured and estimated glomerular filtration rate. N Engl J Med. 2006 Jun 8;354(23):2473-83. doi: 10.1056/NEJMra054415. PMID: 16760447.
- Ebert N, Bevc S, Bökenkamp A, Gaillard F, Hornum M, Jager KJ, Mariat C, Eriksen BO, Palsson R, Rule AD, van Londen M, White C, Schaeffner E. Assessment of kidney function: clinical indications for measured GFR. Clin Kidney J. 2021 Feb 22;14(8):1861-1870. doi: 10.1093/ckj/sfab042. PMID: 34345408; PMCID: PMC8323140.
- Hussain J, Grubic N, Akbari A, Canney M, Elliott MJ, Ravani P, Tanuseputro P, Clark EG, Hundemer GL, Ramsay T, Tangri N, Knoll GA, Sood MM. Associations between modest reductions in kidney function and adverse outcomes in young adults: retrospective, population based cohort study. BMJ. 2023 Jun 22; 381:e075062. doi: 10.1136/bmj-2023-075062. PMID: 37353230; PMCID: PMC10286512.
- Cusumano AM, Tzanno-Martins C, Rosa-Diez GJ. The Glomerular Filtration Rate: From the Diagnosis of Kidney Function to a Public Health Tool. Front Med (Lausanne). 2021 Nov 25; 8:769335. doi: 10.3389/fmed.2021.769335. PMID: 34926510; PMCID: PMC8675900.
- Hill NR, Fatoba ST, Oke JL, Hirst JA, O'Callaghan CA, Lasserson DS, Hobbs FD. Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-Analysis. PLoS One. 2016 Jul 6;11(7):e0158765. doi: 10.1371/journal.pone.0158765. PMID: 27383068; PMCID: PMC4934905.
- Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord. 2017 Feb 7;17(1):53. doi: 10.1186/s12872-017-0482-9. PMID: 28173750; PMCID: PMC5297173.
- Chaitman BR, Cyr DD, Alexander KP, Pracoń R, Bainey KR, Mathew A, Acharya A, Kunichoff DF, Fleg JL, Lopes RD, Sidhu MS, Anthopolos R, Rockhold FW, Stone GW, Maron DJ, Hochman JS, Bangalore S. Cardiovascular and Renal Implications of Myocardial Infarction in the ISCHEMIA-CKD Trial. Circ Cardiovasc Interv. 2022 Aug;15(8):e012103. doi: 10.1161/CIRCINTERVENTIONS.122.012103. Epub 2022 Aug 16. PMID: 35973009.
- Charytan DM, Kuntz RE, Mauri L, DeFilippi C, Ikonomidis JS, McLennan E, Robbins SL, Sabatine MS, Solomon SD, Steg PG, Stone GW, Zannad F, Pfeffer MA. Acute Myocardial Infarction in Patients with Chronic Kidney Disease: Lessons from the CARES Trial. JACC Cardiovasc Interv. 2020 May 11;13(9):1050-1062. doi 10.1016/j.jcin.2020.02.002. PMID: 32381447.
- Hu SS, Wang X, Ye P, Liu Y, Yang Q, Ye Z, Xie Y, Hu R, Xue J, Li J, Chen J. Impact of estimated glomerular filtration rate on long-term clinical outcomes in patients with acute myocardial infarction: a retrospective cohort study. BMC Cardiovasc Disord. 2021 Mar 5;21(1):115. doi 10.1186/s12872-021-01908-0. PMID: 33673756; PMCID: PMC7938314.
- Li X, Li C, Liang H, Xu W, Chen Y, Xiong C, Zhang X, Huang Y, Liang W, Liu X. Association between glomerular filtration rate and clinical outcomes in patients with acute myocardial infarction: a retrospective cohort study. BMC Cardiovasc Disord. 2021 Oct 5;21(1):461. doi 10.1186/s12872-021-02341-0. PMID: 34611104; PMCID: PMC8485940.
- Wang Y, Zhang H, Wang Y, Wang J, Liang J, Wang X, Zhang J, Zhang Y. Association of estimated glomerular filtration rate with risk of mortality in patients with acute myocardial infarction. J Clin Lab Anal. 2021 May;35(5):e23706. doi 10.1002/jcla.23706. Epub 2021 Feb 24. PMID: 33624371.
- Ismail MD, Jalalonmuhali M, Azhari Z, Mariapun J, Lee ZV, Zainal Abidin I, Wan Ahmad WA, Zuhdi ASM; NCVD-PCI investigators. Outcomes of STEMI patients with chronic kidney disease treated with percutaneous coronary intervention: The Malaysian National Cardiovascular Disease Database - Percutaneous Coronary Intervention (NCVD-PCI) registry data from 2007 to 2014. BMC Cardiovasc Disord. 2018 Sep 24;18(1):184. doi: 10.1186/s12872-018-0919-9. PMID: 30249197; PMCID: PMC6154951.
- Major RW, Cheung CK, Gray LJ, Brunskill NJ. Statins and Cardiovascular Primary Prevention in CKD: A Meta-Analysis. Clin J Am Soc Nephrol. 2015 May 7;10(5):732-9. doi: 10.2215/CJN.07460714. Epub 2015 Apr 1. PMID: 25833405; PMCID: PMC4422238.
- Kofman N, Margolis G, Gal-Oz A, Letourneau-Shesaf S, Keren G, Rozenbaum Z, Shacham Y. Long-term renal outcomes and mortality following renal injury among myocardial infarction patients treated by primary percutaneous intervention. Coron Artery Dis. 2019 Mar;30(2):87-92. doi: 10.1097/MCA.0000000000000678. PMID: 30422833.
- Ocak G, Noordzij M, Rookmaaker MB, Cases A, Couchoud C, Heaf JG, Jager KJ. Mortality due to cardiovascular disease in patients with chronic kidney disease at different ages and stages: a nationwide cohort study. BMC Med. 2019 Mar 18;17(1):57. doi 10.1186/s12916-019-1298-4. PMID: 30885116; PMCID: PMC6425732.
- Bansal N, Szpiro AA, Reynolds K, Smith DH, Siscovick D, Fann N, Lumley T. Long-term exposure to ambient air pollution and renal function in older adults: The Cardiovascular Health Study. Environ Int. 2018 Oct; 119:310-319. doi 10.1016/j.envint.2018.06.027. Epub 2018 Jul 5. PMID: 29981997; PMCID: PMC6434893.
- Wang X, Guo Y, Ni Z, Jin Y, Wu J, Chen J. Cardiovascular disease and mortality in patients with chronic kidney disease and acute myocardial infarction: a systematic review and meta-analysis. Ren Fail. 2018 Nov;40(1):657-666. doi 10.1080/0886022X.2018.1488531. PMID: 30086677.
- Wu M, Ruan L, Sun Y, Liang Y, Li H, Huang C, Huang Y, Cai X, Huang X, Qin X. Association of serum uric acid levels with mortality in patients with acute myocardial infarction and chronic kidney disease. BMC Cardiovasc Disord. 2021 Jun 3;21(1):291. doi 10.1186/s12872-021-02050-6. PMID: 34082794; PMCID: PMC8170273.
- Fu Y, Sun H, Guo Z, Xu L, Yang X, Wang L, Li K, Chen M, Gao Y. A risk score model to predict in-hospital mortality of patients with end-stage renal disease and acute myocardial infarction. Intern Emerg Med. 2021 Jun;16(4):905-912. doi: 10.1007/s11739-020-02529-3. Epub 2020 Oct 19. PMID: 33078224.
- Bhandari S, Jain P. Management of acute coronary syndrome in chronic kidney disease. J Assoc Physicians India. 2012 Nov; 60:48-51. PMID: 23767202.
- Sacco A, Montalto C, Bravi F, Ruzzenenti G, Garatti L, Oreglia JA, Bartorelli AL, Crimi G, LA Vecchia C, Savonitto S, Leonardi S, Oliva FG, Morici N. Non-ST-elevation acute coronary syndrome in chronic kidney disease: prognostic implication of an early invasive strategy. Minerva Cardiol Angiol. 2023 Feb;71(1):44-50. doi: 10.23736/S2724-5683.21.05839-7. Epub 2022 Feb 25. PMID: 35212503.
- Sattar S, Ahmed N, Akhter Z, Aijaz S, Lakhani S, Malik R, Pathan A. In-Hospital outcomes in acute coronary syndrome patients with concomitant severe chronic kidney disease undergoing percutaneous coronary intervention. Pak J Med Sci. 2019 Mar-Apr;35(2):291-297. doi: 10.12669/pjms.35.2.276. PMID: 31086503; PMCID: PMC6500806.
- Jun M, Lv J, Perkovic V, Jardine MJ. Managing cardiovascular risk in people with chronic kidney disease: a review of the evidence from randomized controlled trials. Ther Adv Chronic Dis. 2011 Jul;2(4):265-78. doi: 10.1177/2040622311401775. PMID: 23251754; PMCID: PMC3513885.
- Luyckx VA, Tuttle KR, Garcia-Garcia G, Gharbi MB, Heerspink HJL, Johnson DW, Liu ZH, Massy ZA, Moe O, Nelson RG, Sola L, Wheeler DC, White SL. Reducing major risk factors for chronic kidney disease. Kidney Int Suppl (2011). 2017 Oct;7(2):71-87. doi: 10.1016/j.kisu.2017.07.003. Epub 2017 Sep 20. PMID: 30675422; PMCID: PMC6341126.