More Information
Submitted: January 24, 2024 | Approved: February 16, 2024 | Published: February 19, 2024
How to cite this article: Tserioti E, Chana H, Salmasi AM. Calcium Scoring on CT Coronary Angiography in Hypertensive Patients as a Criterion for the Prediction of Coronary Artery Disease. J Cardiol Cardiovasc Med. 2024; 9: 035-043.
DOI: 10.29328/journal.jccm.1001176
Copyright License: © 2024 Tserioti E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Coronary artery; Hypertension; Computed tomography; Coronary angiography
Calcium Scoring on CT Coronary Angiography in Hypertensive Patients as a Criterion for the Prediction of Coronary Artery Disease
Eleni Tserioti1, Harmeet Chana2 and Abdul-Majeed Salmasi3,4*
1Medical Student, Imperial College School of Medicine. London, UK
2Consultant Radiologist, London North West University Healthcare Hospital NHS Trust, London, UK
3Consultant Cardiologist, London North West University Healthcare Hospital NHS Trust, London, UK
4Clinical Senior Lecturer, National Heart and Lung Institute, Imperial College, London, UK
*Address for Correspondence: Dr. Abdul-Majeed Salmasi, Consultant Cardiologist, Central Middlesex Hospital, Acton Lane, London NW10 7NS, UK, Email: [email protected]
Introduction: Hypertension is the strongest independent predictor of Coronary Artery Disease (CAD) identified by Computed tomography of coronary arteries (CTCA). In this study, CTCA-assessed Coronary Calcium Scoring (CCS) was studied in hypertensive subjects referred for CTCA.
Methods: After excluding TAVI and graft assessment patients, the individual electronic health records of 410 consecutive patients who underwent CTCA between July and November 2020, were reviewed with a mean age of 58.7 years. Risk factors were recorded including smoking (38%), hyperlipidaemia (33%), positive family history (22%), systemic hypertension (48%), diabetes mellitus (30%), and male gender (46%). Referral criteria, ethnicity, cardiac, and past medical history were recorded. Patients were stratified into four groups according to CAD severity: absent, mild, moderate, and severe disease, as seen on CTCA. The mean CCS for each CAD category was compared between hypertensive and non-hypertensive patients. Mean CCS were further compared according to the number of coronary arteries affected and the severity of CAD in each artery.
Results: Out of all CTCA reports, 200 (48.8%) CCS were interpreted in the very low-risk category, 80 (19.5%) low risk, 58 (14.1%) moderate risk, 23 (5.6%) moderately high risk and 49 (12.0%) high risk. A significant difference in mean CCS and CAD severity was observed between mild, moderate, and severe CAD (p = 0.015 and p < 0.001). Comparison of CCS between hypertensives and non-hypertensives, across the four CAD severity categories, revealed a significant difference in mean CCS in the severe CAD category (p = 0.03). There was no significant difference in the CCS between hypertensives with chest pain and hypertensives without chest pain. A higher number of affected coronary arteries was associated with a higher mean CCS and a significant difference in CCS was observed between hypertensive and non-hypertensive subjects for the number of arteries affected. Similar results were observed when comparing mean CCS in moderate-severely affected coronary arteries.
Conclusion: Hypertensive patients with a high CCS were associated with a higher incidence of severe CAD independent of the presence of chest pain. These results suggest that the incorporation of CCS in the investigation of CAD on CT angiography may pose a powerful adjunct in proposing an alternative paradigm for the assessment of patients with hypertension, in the progress of coronary artery disease.
Coronary artery disease (CAD) is one of the leading causes of morbidity and mortality worldwide, accounting for 17.3 million deaths per year [1]. As its prevalence continues to rise, the need for a guideline-specific and effective pathway for the diagnosis of CAD is becoming essential.
National Institute for Health and Care Excellence (NICE) guidelines [2] ‘chest pain of recent onset: assessment and diagnosis’ (Clinical guideline 95, update 2016) recommend the use of Computed Tomography Coronary Angiogram (CTCA) as the first-line diagnostic tool for patients with stable chest pain if clinical assessment indicates typical or atypical angina or in patients with non-anginal chest pain who show electrocardiographic (ECG) changes that are suggestive of an underlying CAD. Accordingly, CTCA became a rapidly growing and powerful diagnostic tool to evaluate for the presence of CAD, which has changed the paradigm in the field of diagnostic cardiovascular medicine due to its cost-containing and value-based care [3]. With a high sensitivity and a high negative predictive value in appropriate patient cohorts, its utility in excluding coronary artery disease as a cause of chest pain cannot be understated [4].
Systemic hypertension and CAD share a profound and intricate relationship in the realm of cardiovascular health. Hypertension (HTN) per se can be a precursor for CAD, left ventricular hypertrophy which if untreated can be complicated by myocardial infarction, heart failure, and eventually death. Early identification and management thus can save lives and avoid early onset complications.
Previous studies have been crucial to our current knowledge of the identification of risk factors and their predictive value for CAD [5]. There exists, however, a gap in research into how these risk factors on CAD severity correlate with Coronary Calcium scoring (CCS) and CTCA findings. The understanding of such risk factors is critical not only in the re-evaluation and hence reformation of the CTCA pathway, but also, ultimately, for the prevention of cardiovascular morbidities and mortality altogether.
CCS plays an important role in cardiovascular risk stratification. The most widely used system for the quantification of CCS is the Agatston method which calculates a score based on the extent of coronary artery calcification, incorporating both the area and density of calcium deposits.
The aim of this investigation is to assess the ability of CCS to predict the severity of CAD on CT angiography in patients with arterial hypertension compared with normotensive subjects in a cohort of patients referred for CTCA.
Study population and data source
A retrospective study, reviewing the individual electronic health records of 566 consecutive patients, who underwent CTCA between July and November 2020, was conducted. Data were collected from the imaging database at London North West University Health NHS Trust in London. Patients who received imaging for Transcatheter Aortic Valve Implantation (TAVI) studies, Coronary Artery Bypass Grafting (CABG) assessment studies, and those with inadequate data availability were excluded from the study. Patients with known CAD were not included in the study.
Feature extraction
Data collected were used to define baseline characteristics, cardiovascular risk factors, previous medical history, and interventional procedures (previous percutaneous coronary intervention (PCI), CABG, permanent pacemaker (PPM) insertion or valve transplant). For this patient population, all risk factors were recorded including smoking status, dyslipidaemia, positive family history of cardiac disease, systemic hypertension, diabetes mellitus, and gender. Patients’ racial backgrounds were also recorded (Caucasian, Afro-Caribbean, Indo-Asian, Arabs, Chinese and Other).
Each patient case was followed indefinitely. Referral criteria, CTCA outcomes, and recommendations were reported. Any subsequent investigations and interventions were noted, including dobutamine stress echocardiography (DSE), stress nuclear test, cardiac magnetic resonance (CMR), stress CMR, exercise tolerance testing (ETT), and invasive coronary angiography (ICA).
CCTA was performed prospectively with padding, usually 30% to 80% at 10% intervals, in addition to best phases, with reconstructions of 0.5 mm thickness and 0.25 mm spacing, using small field-of-view images of the heart. Scanning was done using CCTA was carried out using a Siemens AS+ slice scanner (Siemens Healthcare GmbH, Erlangen, Germany). Although heart rate varied per scan, we aimed for ≤ 65 bpm using metoprolol (oral up to 100 mg; intravenous up to 30 mg) where required, safe, and indicated.
Radiology reports were used to collect data on the degree of stenosis and/or calcification in each coronary artery. Other information collected from radiology includes coronary origins and dominance, size of the left ventricle, left atrium and myocardium, aortic root size, pericardial effusion, and hiatus hernia, other non-coronary cardiac abnormality. Coronary Calcium Scoring (CCS) was also recorded and used for statistical analysis.
Outcome definition [6]
The degree of calcification/stenosis in each coronary artery was noted, as ‘absent’, ‘mild’, ‘moderate’, and ‘severe’. The most severe lesion in each case was identified and used for stratification and statistical analysis. Mild disease was defined as < 50% artery stenosis, moderate disease as 50% - 69% and severe disease as ≥ 70%.
Statistical analysis
Subjects were stratified into four groups for analysis: absent, mild, moderate, and severe CAD disease, as seen on CTCA reports. Baseline characteristics and associated risk factors were compared, between patients with absent, mild, moderate, and severe disease, by means of univariate logistics regressions. Univariate analysis of risk factors was performed using the chi-square (χ2) test for categorical variables (gender, diabetes, hypertension, family history, smoking, and dyslipidaemia) and ANOVA for continuous variables (age). The mean CCS for each CAD category was compared between hypertensive and non-hypertensive patients using independent t - tests. Similarly, mean CCS were further compared, by means of a t - test, in regard to the number of coronary arteries affected and the severity of CAD in each artery.
Statistical analysis was performed using the SPSS software package (version 21.0; SPSS Inc., Chicago, IL, USA) [7].
Population characteristics
A total of 420 patient reports were analysed. Continuous variables are presented as means and standard deviations, while categorical variables are displayed as frequencies and percentages.
The mean age at the scan was 58.7 (SD 13.8 years), and 217 patients (52.9%) were females. (Table 1) summarises the baseline demographics and clinical characteristics of the study population (n = 410).
| Table 1:Baseline Demographics and Clinical Characteristics of total cohort. | |
| Variables | Study Patients (n = 410) |
| Age, years | 58.7 ± 13.8 |
| Female | 217 (52.9) |
| Ethnicity | |
| Afro-Caribbean | 6 (1.5) |
| Caucasian | 175 (42.7) |
| Chinese | 3 (0.7) |
| Indo-Asian | 202 (49.3) |
| Other | 24 (5.9) |
| Risk Factors | |
| Hypertension | 197 (48.0) |
| Diabetes | 122 (29.8) |
| Dyslipidaemia | 135 (32.9) |
| Current Smoker | 38 (9.3) |
| Family History | 90 (22.0) |
| Past Medical History | |
| Valve Transplant | 1 (0.2) |
| PPM | 6 (1.5) |
| Aortic Stenosis | 4 (1.0) |
| Results are presented as mean ± standard deviation or frequencies (percentage). CABG: Coronary Artery Bypass Graft; PCI: Percutaneous Coronary Intervention; PPM: Permanent Pacemaker. Defibrillator. | |
Understanding CTCA results – statistical analysis
Subjects were stratified into four groups for analysis: absent, mild, moderate, and severe CAD disease, as seen on CTCA reports.
To aid analysis of results, baseline population characteristics were compared (Table 2), between the four groups: absent, mild, moderate, and severe CAD. The normality of data was assessed via Kolmogorov-Smirnov and Shapiro-Wilk tests. The mean age increases with the severity of CAD, whereas the percentage of females who had CAD decreases dramatically with severity.
Out of all CTCA reports, 200 (48.8%) CCS were interpreted in the very low-risk category, 80 (19.5%) low risk, 58 (14.1%) moderate risk, 23 (5.6%) moderately high risk and 49 (12.0%) high risk.
The prevalence of hypertensive and diabetic patients increases with increasing severity of CAD. The prevalence of dyslipidaemia was the highest in patients with severe CAD, whereas the prevalence of smokers remains relatively similar across all four categories. Out of the total cohort, 203 (48.3%) patients were hypertensive.
182 (43.3%) patients of the total cohort presented with atypical chest pain symptoms, whereas only 37 (8.8%) had typical chest pain. As seen in Table 2, the majority of patients with atypical chest pain showed absent-mild CAD, whereas a majority of those with typical chest pain showed severe CAD on CTCA. A further 71 patients presented with non-anginal pain, either in the form of musculoskeletal-sounding chest pain or palpitations. 130 patients reported no chest pain at all, prior to CTCA.
| Table 2: Comparison of Baseline Characteristics and Risk Factors, amongst the 4 groups of CAD disease. | |||||
| CAD | |||||
| Variables | No Stenosis (n = 200) |
Mild (n = 80) | Moderate (n = 69) | Severe (n = 61) |
p - value |
| Age, years | 59.1 ± 13.3 | 57.7 ± 13.6 | 57.1 ± 15.2 | 60.4 ± 13.9 | < 0.001* |
| Female | 104 (52.0) | 41 (51.3) | 30 (43.4) | 42 (68.9) | 0.001* |
| Ethnicity | 0.392 | ||||
| Afro-Caribbean | 5 (2.5) | 0 (0.0) | 0 (0.0) | 1(1.6) | |
| Caucasian | 77 (38.5) | 39 (48.8) | 30 (43.4) | 29 (47.5) | |
| Chinese | 2 (1.0) | 1(1.3) | 0 (0.0) | 0 (0.0) | |
| Indo-Asian | 100 (50.0) | 38 (47.5) | 26 (37.7) | 38 (62.3) | |
| Other | 16 (8.0) | 4 (5.0) | 3 (4.3) | 1 (1.6) | |
| Risk Factors | |||||
| Hypertension | 62 (31.0) | 41 (51.3) | 40 (58.0) | 54 (88.5) | < 0.001* |
| Diabetes | 47 (23.5) | 24 (30.0) | 20 (29.0) | 31 (50.8) | 0.011* |
| Dyslipidaemia | 53 (26.5) | 28 (35.0) | 22 (31.9) | 37 (60.7) | 0.007* |
| Current Smoker | 13 (6.5) | 12 (15.0) | 9 (13.0) | 4 (6.6) | 0.020* |
| Family History | 41 (20.5) | 22 (27.5) | 12 (17.4) | 15 (24.6) | 0.451 |
| Chest Pain | < 0.001* | ||||
| Typical (n = 37) | 8 (4.0) | 6 (7.5) | 9 (13.0) | 14 (23.0) | |
| Atypical (n = 142) | 87 (43.5) | 36 (45.0) | 27 (39.1) | 25 (41.0) | |
| Mean CCS | 0.2 ± 0.07 | 59.5 ± 11.5 | 460.5 ± 96.3 | 1036.4 ± 40.0 | < 0.001* |
| Statistical analysis was done using chi-square test for categorical variables (gender, ethnicity, risk factors and chest pain) and one-way ANOVA for numerical variables (age, mean CCS). CCS; Coronary Calcium Score. Results are presented as mean ± standard deviation or frequencies (percentage). (*p ≤ 0.05). | |||||
Univariate analysis (Table 2), for comparison of patients with absent, mild, moderate, and severe CAD revealed that age, gender, hypertension, diabetes, dyslipidaemia, and smoking were all independently associated with the presence of CAD on CTCA / higher risk for CAD. However, family history of cardiac disease or ethnicity was not a significant predictor of CAD on CTCA.
Coronary Calcium Score (CCS)
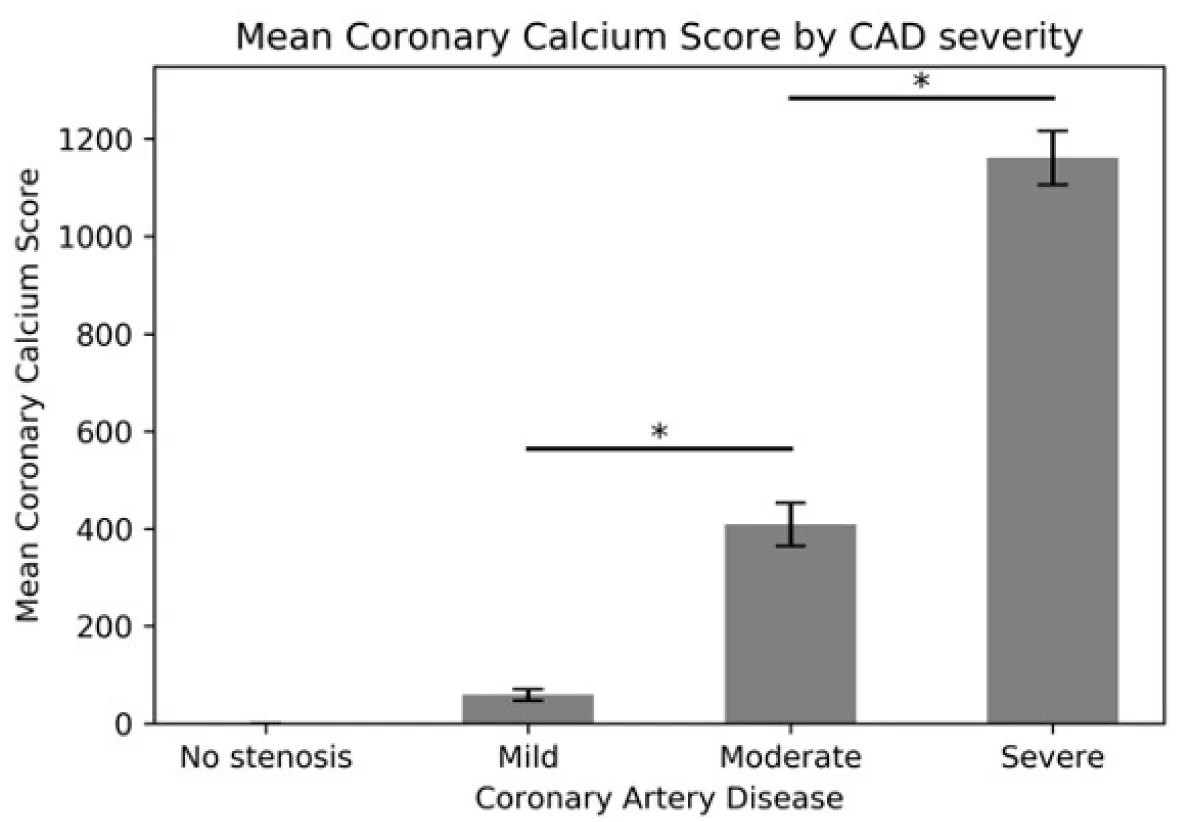
The mean CCS was calculated for each CAD category, as observed on CTCA (Figure 1). An increase in mean CCS is observed, with increasing severity of coronary disease. A significant difference in mean CCS and CAD severity was observed between mild, moderate, and severe CAD (p < 0.001).
Figure 1: Comparison of mean CCS for none, mild, moderate and severe CAD. Statistical analysis was done using independent one-sided t - test. Errors bars represent Std. Error. (*p < 0.001).
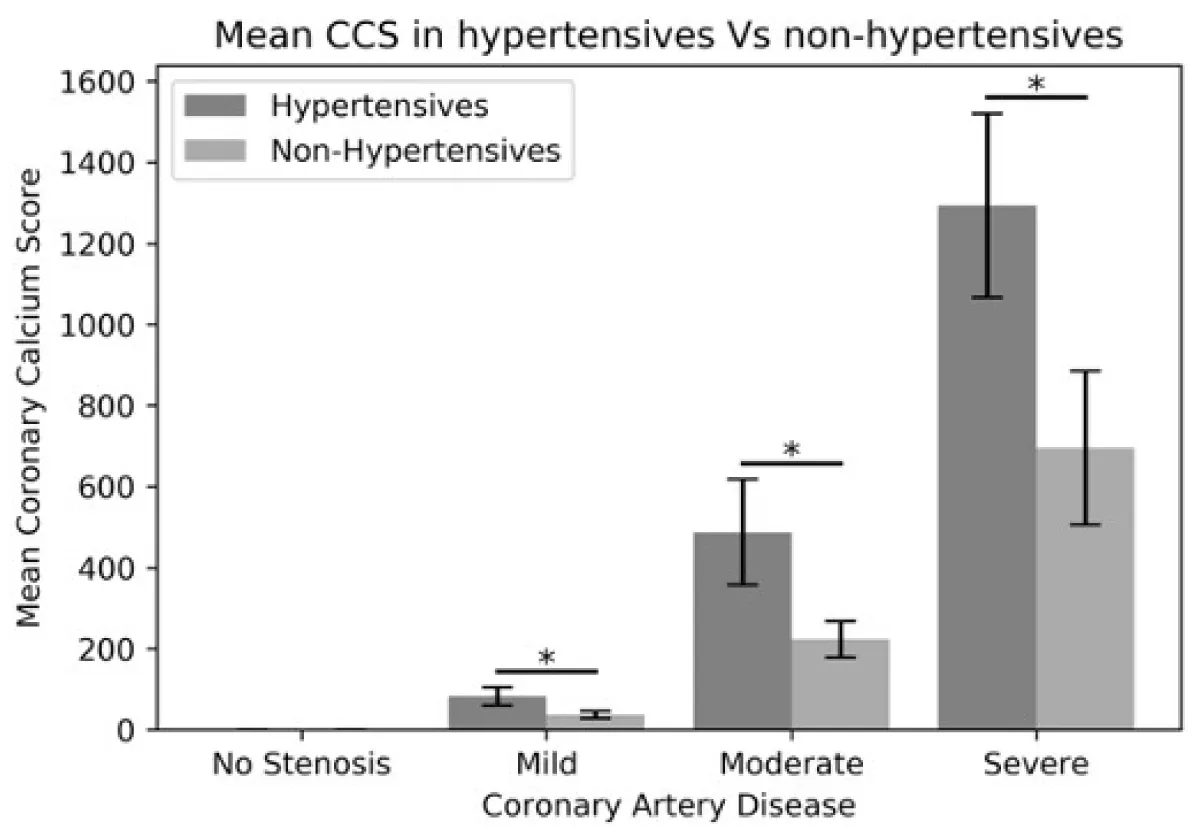
Mean CCS and hypertension
Accounting for the results of the univariate analysis and our previous study, (that Hypertension is the strongest independent predictor for the presence of CAD on CTCA, amongst diabetes, gender, dyslipidaemia, and smoking), the mean CCS was compared between Hypertensive and Normotensive patients across the four CAD severity categories (Table 3, Figure 2). A significant difference in mean CCS is observed in the mild (p = 0.033), moderate (p = 0.033), and severe (p = 0.030) CAD categories (Figure 3, Table 4).
Figure 2: Relationship between Glomerular Filtration Rate and Mortality.
Figure 3: Graphical representation of Table 3. Statistical analysis was done using independent one-sided t - tests. Error bars represent Std. Error. (*p ≤ 0.05,).
| Table 3: Comparison of Mean CCS in hypertensives and normotensive subjects, for Absent, Mild, Moderate and Severe CAD as seen on CTCA. | |||
| Mean CCS | |||
| CAD severity | Hypertensives (n = 197) | Normotensives (n = 213) | p - value |
| Absent stenosis (n = 200) | 0.23 ± 0.14 | 0.16 ± 0.08 | 0.216 |
| Mild (n = 80) | 82.6 ± 22.1 | 36.8 ± 9.01 | 0.033* |
| Moderate (n = 69) | 487.3 ± 131.6 | 223.2 ± 44.3 | 0.033* |
| Severe (n = 61) | 1293.0 ± 227.1 | 694.9 ± 198.6 | 0.030* |
| Statistical analysis was done using independent one-sided t - tests. Results are presented as mean ± standard error. (*p ≤ 0.05). | |||
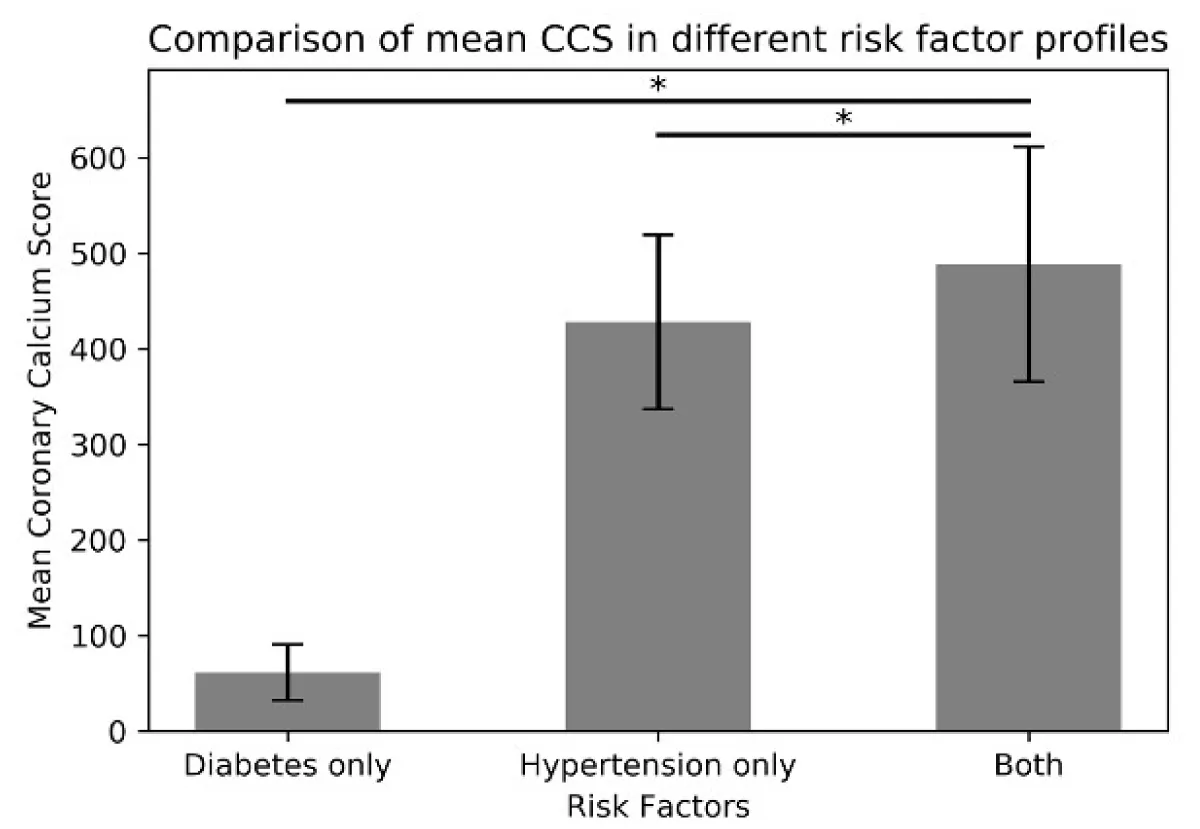
| Table 4:Comparison of Mean CCS in patients with only hypertension, diabetes only and patients with both hypertension and diabetes, for Absent, Mild, Moderate and Severe CAD as seen on CTCA. | ||||
| Mean CCS | ||||
| CAD severity | Diabetics only (n = 34) | Hypertensives only (n = 109) | Hypertensive diabetics (n = 88) | p - value |
| Absent (n = 84) | 0.24 ± 0.23 | 0.26+0.18 | 0.31 +1.21 | 0.963 |
| Mild (n = 46) | 49.81 ± 22.9 | 48.46 ± 16.2 | 123.58 ± 42.3 | 0.148 |
| Moderate (n = 52) | 279.13 ± 180.3 | 539.86 ± 191.0 | 416.28 ± 169.1 | 0.834 |
| Severe (n = 49) | 419.00 ± 181.7 | 1301.82 ± 272.2 | 1285.23 ± 356.7 | 0.741 |
| Statistical analysis was done using one way ANOVA. Results are presented as mean ± standard error. (*P ≤ 0.05). | ||||
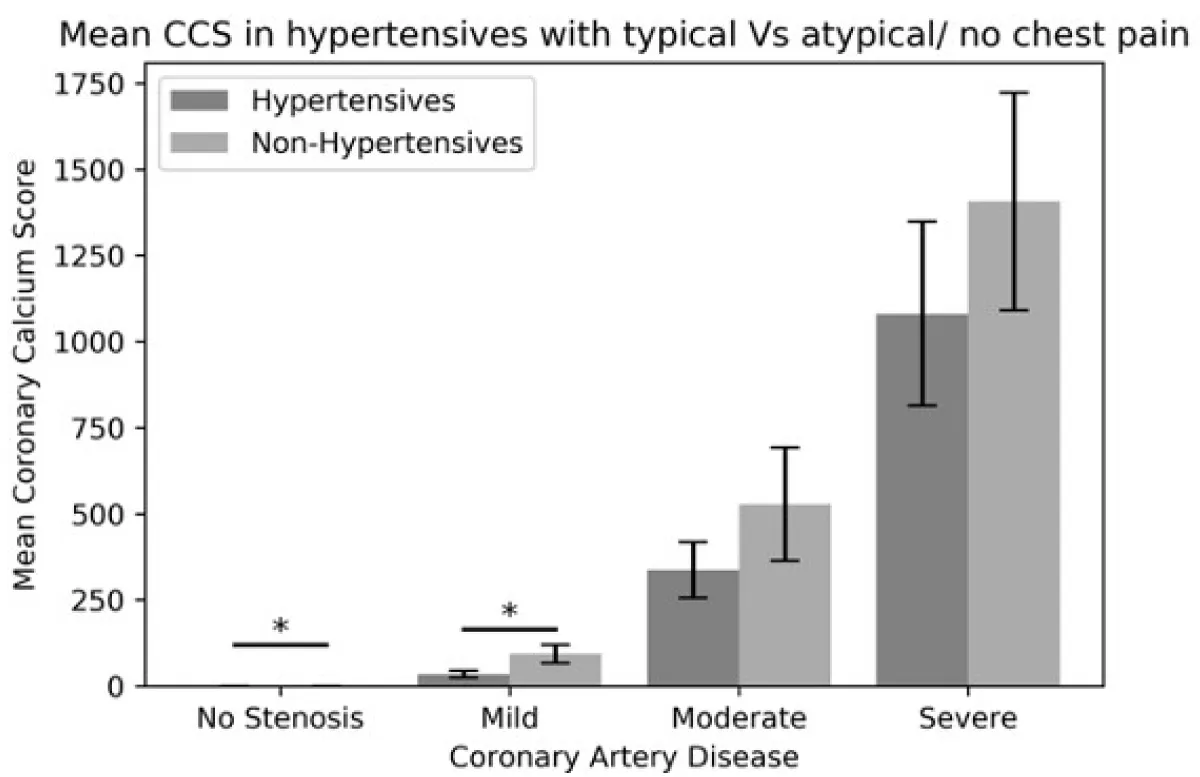
The mean CCS in hypertensive patients with typical chest pain were compared against hypertensives with atypical or no chest pain with regard to CAD severity (Table 5, Figure 4). A significant difference was observed in patients with absent stenosis (p = 0.023) and mild CAD (0.027) thus suggesting that CCS does not help to differentiate hypertensive subjects with or without chest pain.
| Table 5: Comparison of Mean CCS in hypertensive patients with chest pain and those without chest pain, for Absent, Mild, Moderate and Severe CAD as seen on CTCA. | |||
| Mean CCS | |||
| CAD severity | Hypertensives + Typical Chest Pain (n = 45) | Hypertensives + Atypical/ No Chest Pain (n = 152) | p - value |
| Absent stenosis (n = 62) | 0.0 ± 0.0 | 0.33 ± 0.16 | 0.023* |
| Mild (n = 39) | 34.5 ± 10.3 | 93.3 ± 26.5 | 0.027* |
| Moderate (n = 49) | 336.8 ± 81.2 | 527.9 ± 165.0 | 0.157 |
| Severe (n = 47) | 1080.8 ± 267.7 | 1406.4 ± 315.7 | 0.223 |
| Statistical analysis was done using independent one-sided t - test. Results are presented as mean ± standard error. | |||
Figure 4: Graphical Representation of Table 4. Error bars represent Std. Error. (*p ≤ 0.05).
CCS and number of diseased coronary arteries
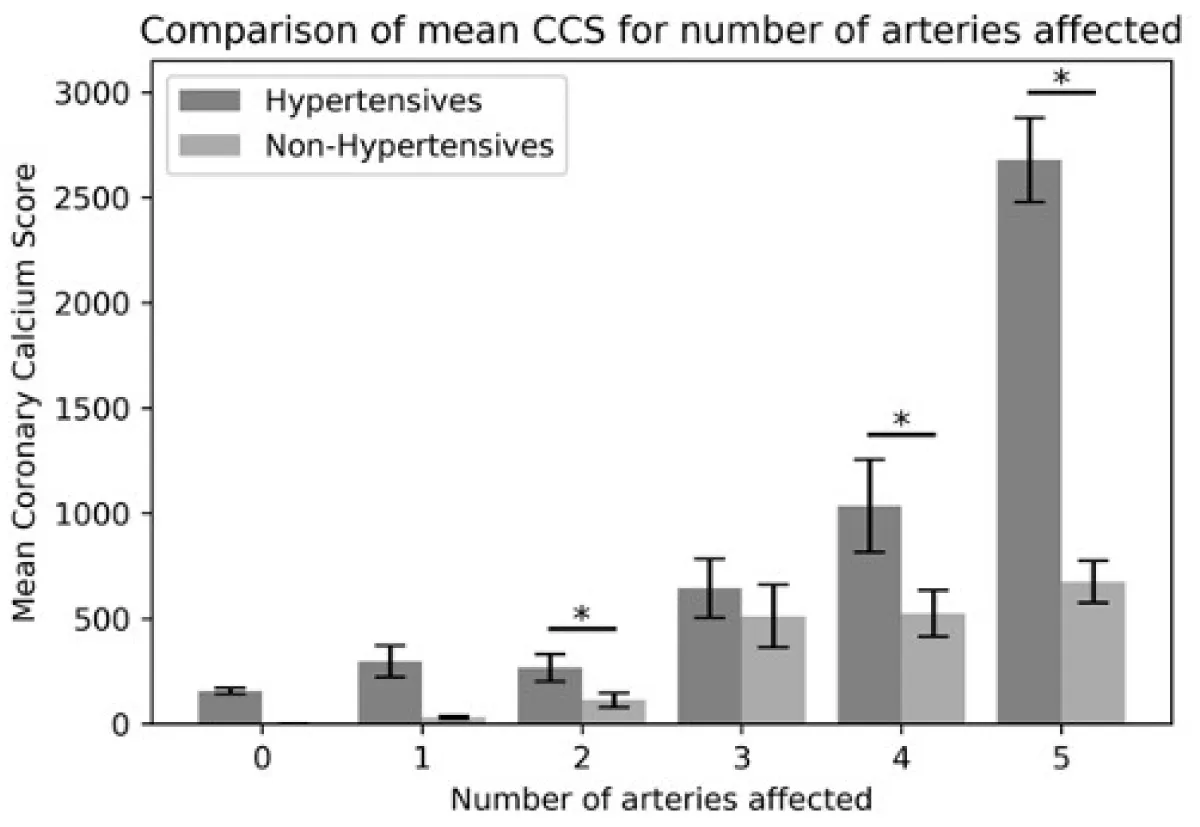
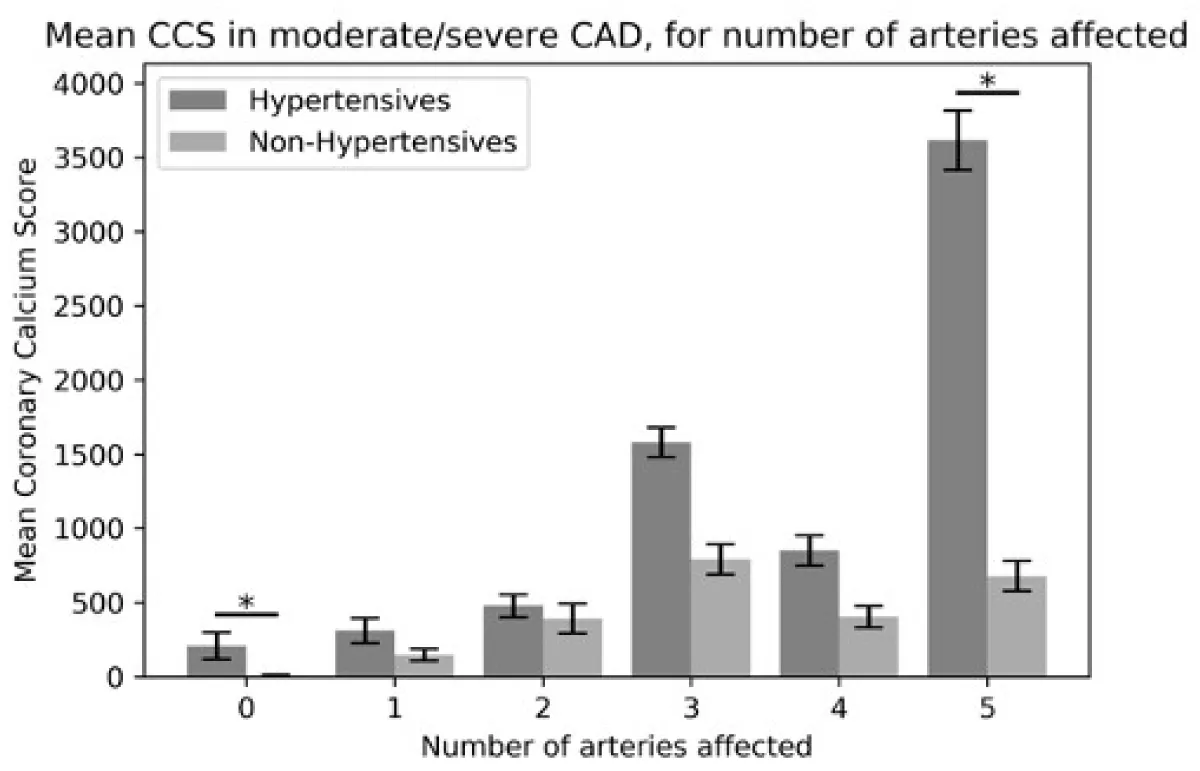
A higher number of affected coronary arteries correlated with a higher mean CCS and a significant difference in CCS was observed between hypertensives and non-hypertensives for the number of arteries affected (Table 6, Figure 5). Similar results were observed when comparing mean CCS in moderate-severely affected coronary arteries (Tables 6,7 Figure 6).
| Table 6: Comparison of Mean CCS in hypertensive patients and non-hypertensives, for number of coronary arteries affected with CAD as seen on CTCA. | |||
| Total number of arteries affected | Mean CCS | ||
| Hypertensives | Non-Hypertensives | p - value | |
| 0 | 156.0 ± 14.3 | 0.1 ± 0.0 | 0.181 |
| 1 | 297.4 ± 75.1 | 30.3 ± 7.6 | 0.142 |
| 2 | 267.5 ± 65.1 | 112.6 ± 35.8 | 0.047* |
| 3 | 645.3 ± 148.6 | 511.4 ± 157.7 | 0.549 |
| 4 | 1035.6 ± 225.7 | 524.0 ± 118.7 | 0.007* |
| 5 | 2679.0 ± 242.2 | 676.0 ± 100.0 | 0.019* |
| Statistical analysis was done using independent t-test. Results are presented as mean ± SEM. Number of arteries involved, refers to the four main coronary arteries, namely Left Main Artery, Left anterior descending (LAD), Left Circumflex and Right Coronary Artery (RCA) and their branches. | |||
| Table 7: Comparison of Mean CCS in hypertensive patients and non-hypertensives, for number of coronary arteries affected with CAD as seen on CTCA. Statistical analysis was done using independent t - test. Results are presented as mean ± standard deviation. | |||
| N of moderate-severely arteries affected | Mean CCS | ||
| Hypertensives | Non- Hypertensives | p - value | |
| 0 | 208.0 ± 91.2 | 8.7 ± 2.3 | 0.032* |
| 1 | 311.6 ± 83.9 | 147.6 ± 43.8 | 0.095 |
| 2 | 478.8 ± 76.9 | 392.4 ± 109.0 | 0.545 |
| 3 | 1579.8 ± 105.6 | 791.6 ± 262.8 | 0.073 |
| 4 | 850.8 ± 168.3 | 403.9 ± 72.8 | 0.314 |
| 5 | 3614.8 ± 262.0 | 676.0 ± 100.0 | 0.038* |
Figure 5: Graphical Representation of Table 5. Error bars represent Std. Error. (*p ≤ 0.05).
Figure 6: Graphical Representation of Table 6. Error bars represent Std. Error (*p ≤ 0.05).
We have shown that hypertensive patients with a high CCS have a higher incidence of severe CAD independent of the presence or absence of stable chest pain. Compared to normotensive patients, additional symptoms in those with hypertension, appear to have no effect on CCS. Furthermore, this data has shown that a higher number of affected coronary arteries was associated with a higher mean CCS, and a significant difference in CCS was observed between hypertensives and non-hypertensives for the number of affected arteries. These novel results further enhance the prominence of hypertension as the most important predictor for CAD severity, while additionally revealing the equally important implication of CCS in the presence and investigation pathway of CAD on CT angiography.
The use of CCS in the coronary arteries is a reliable predictor of coronary heart disease events. Because of its ease of use and lack of invasiveness, it is broadly used in clinical practice for determining the risk of major cardiovascular events. With high sensitivities for disease (from 88% to 100%) [8-11] a negative test has a negative predictive value of nearly 100% for ruling out significant coronary disease [12-14]. Therefore, asymptomatic individuals with no associated risk factors and CCS = 0 are highly unlikely to have any atheromatous plaque or any cardiovascular events within the next two to five years [15]. On the contrary, positive (non-zero) CCS scores, indicate the existence of coronary atherosclerotic disease, and rising values are linked to increased CAD risk [16]. Despite this, studies have questioned the use of CCS in low-risk populations since significant stenosis with a CCS of 0, is possible [17]. Nonetheless, the added predictive value of CCS on CV events remains to be confirmed [18].
The association of CCS with CAD has been shown by many prospective studies [19]. Results from this study are consistent with previous studies (MESA, Framingham, and the Cardiovascular Health Study, Rotterdam, HNR) demonstrating that increasing CCS is associated with increased CAD risk. This study expands these findings, demonstrating that in patients with hypertension, a high CCS was associated with a higher incidence of severe CAD, as compared to normotensive patients.
MESA, a prospective multicentre study, used electron-beam computed tomography (EBCT) to investigate the CCS distribution across different ethnicities [20]. Most importantly, MESA introduced the presentation of estimated curves for the 50th, 75th, and 90th percentiles of CCS across age, aiding the clinical interpretation of CCS by providing guidance as to what constitutes a high CCS for a particular patient [21]. While these results are noteworthy in examining the distribution of CCS on the basis of age, gender, and ethnicity, CCS differences across ethnicities were not fully explained by risk factor discrepancies, suggesting that other factors must be accountable for the variability in CCS. Our previous study did not find any significant difference in ethnicity between hypertensive and non-hypertensives, suggesting that ethnicity is not a significant predictor of CAD severity, nor hypertension in the context of CTCA [22]. This could be due to the small cohort size of certain ethnic groups in our study. Larger cohort studies, of equally sized ethnic groups, would be essential in further establishing the predictive value of ethnicity on cardiovascular disease.
The CARDIA study included individuals aged between 32 and 46 years, to investigate the prognostic effect of CCS on CAD. The study reported CCS to highly predict risk beyond established risk variables in younger adults over a 10-year follow-up [23]. A CCS score of 100 or more was associated with an increased risk of fatal and nonfatal CHD during 12.5 years of follow-up. Therefore, selective use of screening for CCS might be considered in individuals with risk factors in early adulthood to inform discussions about primary prevention.
The predictive value of CCS scanning in symptomatic patients is less clearly established. Previous studies evaluating the accuracy of CCS score to detect significant CAD in a low-intermediate risk emergency department (ED) population have predominantly shown CCS to be an effective initial tool for risk stratification of low- to intermediate-risk patients with possible acute coronary syndromes, on the basis of its high sensitivity and high negative predictive value and additive diagnostic value [24-28]. Dennis et al conducted a prospective study in ED patients with stable chest pain and concluded that patients with absence/low CCS, are more likely to be experiencing non-cardiac chest discomfort.
Although these test characteristics would suggest the use of CCS as an effective supplement in evaluating people at low-to-intermediate risk, many studies argue that CCS alone did not improve prognostic value [29] in symptomatic patients.
A CCS of 0, does not rule out ACS, and a high CCS score does not rule out the need for CTCA [30].
CCS as a stand-alone test for acute chest pain triage has not been recommended per current guidelines [31]. Notable reasons for this recommendation are that these conclusions were derived from relatively small cohort studies, the possibility of missing obstructive non-calcified plaque, and the rapidly emerging evidence that CTCA is a safe and efficient tool in the triage of low-intermediate risk patients with acute chest pain in the ED [32-35].
Further, our current study has shown that a higher number of affected coronary arteries was associated with a higher mean CCS, and a significant difference in CCS was observed between hypertensive and non-hypertensive subjects for the number of affected arteries. Previous studies [36,37] agreed that the regional distribution of CCS and in particular the total number of coronary arteries affected, adds prognostic information, with higher risk in patients with diffuse atherosclerotic disease. Specifically, the Framingham Heart Study (FHS) concluded that the number of coronary arteries with CCS and the presence of CCS in the dominant coronary artery was significantly linked with major CV events over a median follow-up of seven years [38].
A high calcium score indicates an increased burden of atherosclerotic plaque in the coronary arteries. For hypertensive patients, this can be an essential tool for risk assessment. Since hypertension is a known risk factor for atherosclerosis and CAD, when combined with a high calcium score, it suggests a more significant risk of future cardiovascular events, such as heart attacks and strokes.
Future directions and guidelines [39]
The 2016 NICE guidelines on stable chest pain of recent onset, recommend that all patients with new onset stable chest pain should be investigated with a CTCA as a first-line investigation. However, the current national guidelines do not address the inequity between the increasing demand for CTCA and the contrasting constrained imaging capacity. In a previous study, we showed hypertension to be the strongest independent predictor of CAD detected on CTCA. Combined with the results of the current study, HTN remains the strongest independent predictor of CAD. Nonetheless, the use of CCS in the CTCA referral pathway is deemed equally important. The combination of the two factors can yield a powerful adjunct in proposing an alternative paradigm for the investigation of patients with hypertension and stable chest pain.
Interestingly, NICE guidelines, no longer recommend the use of a zero-calcium score to rule out CAD even in patients with a low-risk factor profile, because of case reports of significant coronary stenoses in patients with a zero-calcium score [40]. The 2017 guidelines from the SCCT recommended consideration of CCS testing, in the context of shared decision-making, for asymptomatic individuals with a 10-year atherosclerotic cardiovascular disease (ASCVD) risk of 5% to 20%, or in those with < 5% ten-year risk but with another strong indication, such as a family history of premature CAD [41]. Further, the 2018 US Preventative Services Task Force Guidelines on non-traditional risk factors, recommend that in asymptomatic adults, the current evidence is insufficient to assess the balance of benefits and harms of adding CAD score to traditional risk assessment for CVD prevention.
Future directions - Perfecting the guidelines
An approach, in attempting to minimise the number of CTCA referrals, would look into evaluating CCS data to skip unnecessary CTCA if obstructive lesions are highly unlikely. Previous studies have shown CCS to be a strong discriminator for obstructive CAD, suggesting that it should be accounted for in future studies. In asymptomatic patients with low to moderate atherosclerotic cardiovascular disease, CCS predicts atherosclerotic disease risk with high accuracy. However, in symptomatic patients, the value of CCS is less clear.
To further narrow down the pathway, we analysed the data to assess the CCS in hypertensive patients with typical chest pain against how many with atypical chest pain or no chest pain had significant CAD on CTCA. The data has shown that hypertensive patients with a high CCS were associated with a higher incidence of severe CAD independent of the presence or absence of stable chest pain. The data has also shown that the higher the CCS in hypertensive patients, the higher the risk of severe CAD, as compared to non-hypertensives, regardless of chest pain presentation. Consequently, a high CCS in the absence of hypertensives poses a lower risk of severe disease. These results suggest that hypertension remains the distinguishable factor and the strongest independent predictor for severe CAD and that those with hypertension, regardless of chest pain presentation, may benefit from alternative or concurrent functional investigation to better distinguish flow-limiting from non-flow-limiting CAD, depending on the treatment algorithm employed.
The presence of a high calcium score should prompt healthcare providers to intensify treatment and management strategies for hypertensive patients. This may include more aggressive blood pressure control, and cholesterol-lowering medication, in addition to lifestyle modifications such as diet and exercise to reduce cardiovascular risk.
In summary, a high calcium score in hypertensive patients holds significant value by aiding in risk assessment, guiding treatment decisions, motivating lifestyle changes, and monitoring disease progression. It underscores the importance of proactive cardiovascular risk management for individuals with hypertension.
Improving the CCS
The potential implementation of a new and improved CCS score in clinical practice is a matter of current debate [42]. Emerging evidence on the use of thinner slices for the detection of microcalcifications would be useful in distinguishing coronary atherosclerotic lesions in patients with zero CAC scores [43]. A new CCS score may potentially incorporate extra-coronary calcification (ECC) to improve individualized risk prediction, as evidence mounts that ECC has a graded association with higher CHD and mortality risk [44].
Most importantly, the prognostic value of the test can be further increased if the age and sex distribution within percentiles are taken into account. According to the 2016 European Guidelines on Cardiovascular Disease Prevention in clinical practice, a CAC score ≥ 300 Agatston units or ≥ 75th percentile for age, sex, and ethnicity is considered to indicate increased CV risk [44].
This study was limited because no quantifiable measures of hypertension, such as classification categories (Stage 1 or 2), were included in the analysis. The lack of available documentation on the electronic health records of patients has hindered this effort. A more detailed inspection into the classification of hypertension in patients would prove essential in enhancing our understanding of hypertension and risk factor pre-assessment for CTCA referrals.
Further, an element of selection bias may be present in the dataset, since those with the heaviest smoking history, the greatest degree of dyslipidaemia, and the most severe family history, may not necessarily have been referred for CTCA as they are deemed to be in a high-risk category. Naturally, without continuous data, this could not be evaluated. This selection bias may account partly, for some of the results that contradict earlier literature in failing to show a significant association between family history, diabetes, and smoking, on CAD predictability.
A supplementary limitation arises from the fact that the assessment of CAD severity was conducted by radiologists who possess prior knowledge of the CCS results. This circumstance potentially introduces bias into the interpretation of CAD, as the radiologists may inadvertently weigh their assessments in light of the CCS findings. Consequently, there exists a possibility of overestimation or underestimation of CAD severity, influenced by the pre-existing knowledge of the CCS results. Such an influence could introduce variability and compromise the accuracy of CAD interpretation in this study. Further exploration and consideration of strategies to mitigate the impact of this potential bias are warranted for future investigations in this domain.
Although the link between CCS and CAD in hypertensive patients is clear, future studies should be conducted to evaluate how useful CCS can be in the CTCA referral pathway. In line with our current understanding of risk factors and their predictive effect on CAD, it is vital that future studies on CCS, assess strict control of risk factors, especially of hypertension. The use of CCS as a valid screening tool for early diagnosis of CAD in asymptomatic patients is vital in the appropriate prevention and ultimately decrease of CAD-related mortality and morbidity.
Hypertensive patients with a high CCS were associated with a higher incidence of severe CAD. Further, in those with hypertension, an additional symptom of stable chest pain appears to have no effect on CCS. Combined, these results suggest that the incorporation of CCS in the investigation of CAD on CT angiography should be considered a key parameter in the assessment of patients for investigation of angiographic coronary disease.
Ethical consideration: This study was an audit done by the first author as part of her degree. Therefore no Ethical approval was required.
- Brown JC. Risk factors for coronary artery disease. StatPearls. 2023. https://www.ncbi.nlm.nih.gov/books/NBK554410/
- Overview: Recent-onset chest pain of suspected cardiac origin: Assessment anddiagnosis: Guidance. NICE. (n.d.). https://www.nice.org.uk/Guidance/CG95
- Rubin GD, Leipsic J, Joseph Schoepf U, Fleischmann D, Napel S. CT angiography after 20 years: a transformation in cardiovascular disease characterization continues to advance. Radiology. 2014 Jun;271(3):633-52. doi: 10.1148/radiol.14132232. PMID: 24848958; PMCID: PMC4669887.
- Gatti M. Diagnostic Accuracy of Coronary Computed Tomography Angiography (CCTA) for the Evaluation of Obstructive Coronary Artery Disease in Patients Referred for Transcatheter Aortic Valve Implantation (Tavi): A Systematic Review and Meta-analysis. 2019. https://doi.org/10.26226/morressier.60e81cd3e537565438d6c6ca
- DAWBER TR, MEADORS GF, MOORE FE Jr. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health. 1951 Mar;41(3):279-81. doi: 10.2105/ajph.41.3.279. PMID: 14819398; PMCID: PMC1525365.
- NHS. (n.d.). Carotid endarterectomy - when it’s needed. NHS choices. https://www.nhs.uk/conditions/carotid-endarterectomy/why-its-done/
- IBM (2012) IBM SPSS Statistics for Windows (Version 21.0). Armonk, NY: IBM.
- Margolis JR, Chen JT, Kong Y, Peter RH, Behar VS, Kisslo JA. The diagnostic and prognostic significance of coronary artery calcification. A report of 800 cases. Radiology. 1980 Dec;137(3):609-16. doi: 10.1148/radiology.137.3.7444045. PMID: 7444045.
- Simons DB, Schwartz RS, Edwards WD, Sheedy PF, Breen JF, Rumberger JA. Noninvasive definition of anatomic coronary artery disease by ultrafast computed tomographic scanning: a quantitative pathologic comparison study. J Am Coll Cardiol. 1992 Nov 1;20(5):1118-26. doi: 10.1016/0735-1097(92)90367-v. PMID: 1401612.
- Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995 Oct 15;92(8):2157-62. doi: 10.1161/01.cir.92.8.2157. PMID: 7554196.
- Rumberger JA, Schwartz RS, Simons DB, Sheedy PF 3rd, Edwards WD, Fitzpatrick LA. Relation of coronary calcium determined by electron beam computed tomography and lumen narrowing determined by autopsy. Am J Cardiol. 1994 Jun 15;73(16):1169-73. doi: 10.1016/0002-9149(94)90176-7. PMID: 8203333.
- Budoff MJ, Diamond GA, Raggi P, Arad Y, Guerci AD, Callister TQ, Berman D. Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography. Circulation. 2002 Apr 16;105(15):1791-6. doi: 10.1161/01.cir.0000014483.43921.8c. PMID: 11956121.
- Shavelle DM, Budoff MJ, LaMont DH, Shavelle RM, Kennedy JM, Brundage BH. Exercise testing and electron beam computed tomography in the evaluation of coronary artery disease. J Am Coll Cardiol. 2000 Jul;36(1):32-8. doi: 10.1016/s0735-1097(00)00696-3. PMID: 10898409.
- Haberl R, Becker A, Leber A, Knez A, Becker C, Lang C, Brüning R, Reiser M, Steinbeck G. Correlation of coronary calcification and angiographically documented stenoses in patients with suspected coronary artery disease: results of 1,764 patients. J Am Coll Cardiol. 2001 Feb;37(2):451-7. doi: 10.1016/s0735-1097(00)01119-0. PMID: 11216962.
- Neves PO, Andrade J, Monção H. Coronary artery calcium score: current status. Radiol Bras. 2017 May-Jun;50(3):182-189. doi: 10.1590/0100-3984.2015.0235. PMID: 28670030; PMCID: PMC5487233.
- Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2005 Mar 15;111(10):1313-20. doi: 10.1161/01.CIR.0000157730.94423.4B. PMID: 15769774.
- Marwan M, Ropers D, Pflederer T, Daniel WG, Achenbach S. Clinical characteristics of patients with obstructive coronary lesions in the absence of coronary calcification: an evaluation by coronary CT angiography. Heart. 2009 Jul;95(13):1056-60. doi: 10.1136/hrt.2008.153353. Epub 2009 Apr 22. PMID: 19389719.
- Gibson AO, Blaha MJ, Arnan MK, Sacco RL, Szklo M, Herrington DM, Yeboah J. Coronary artery calcium and incident cerebrovascular events in an asymptomatic cohort. The MESA Study. JACC Cardiovasc Imaging. 2014 Nov;7(11):1108-15. doi: 10.1016/j.jcmg.2014.07.009. Epub 2014 Nov 10. PMID: 25459592; PMCID: PMC4254694.
- Hecht HS, Superko HR. Electron beam tomography and national cholesterol education program guidelines in asymptomatic women. ACC Current Journal Review. 2001; 10(5): 24. https://doi.org/10.1016/s1062-1458(01)00371-3
- McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2006 Jan 3;113(1):30-7. doi: 10.1161/CIRCULATIONAHA.105.580696. Epub 2005 Dec 19. PMID: 16365194.
- Carr JJ, Jacobs DR Jr, Terry JG, Shay CM, Sidney S, Liu K, Schreiner PJ, Lewis CE, Shikany JM, Reis JP, Goff DC Jr. Association of Coronary Artery Calcium in Adults Aged 32 to 46 Years With Incident Coronary Heart Disease and Death. JAMA Cardiol. 2017 Apr 1;2(4):391-399. doi: 10.1001/jamacardio.2016.5493. PMID: 28196265; PMCID: PMC5397328.
- Tserioti E, Chana H, Salmasi AM. Hypertensive Subjects are More Likely to Develop Coronary Artery Lesions: A Study by Computerised Tomography Coronary Angiography. Angiology. 2023 Sep 7:33197231200774. doi: 10.1177/00033197231200774. Epub ahead of print. PMID: 37678558.
- Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffmann U, Cury RC, Abbara S, Brady TJ, Budoff MJ, Blumenthal RS, Nasir K. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging. 2009 Jun;2(6):675-88. doi: 10.1016/j.jcmg.2008.12.031. Erratum in: JACC Cardiovasc Imaging. 2010 Oct;3(10):1089. Hoffman, Udo [corrected to Hoffmann, Udo]. PMID: 19520336.
- Fernandez-Friera L, Garcia-Alvarez A, Bagheriannejad-Esfahani F, Malick W, Mirelis JG, Sawit ST, Fuster V, Sanz J, Garcia MJ, Hermann LK. Diagnostic value of coronary artery calcium scoring in low-intermediate risk patients evaluated in the emergency department for acute coronary syndrome. Am J Cardiol. 2011 Jan;107(1):17-23. doi: 10.1016/j.amjcard.2010.08.037. PMID: 21146680.
- Georgiou D, Budoff MJ, Kaufer E. Screening patients with chest pain in the emergency department using Electron Beam Computer Tomography: A follow-up study. ACC Current Journal Review. 2002; 11(1): 37. https://doi.org/10.1016/s10621458(01)00562-1
- Nabi F, Chang SM, Pratt CM, Paranilam J, Peterson LE, Frias ME, Mahmarian JJ. Coronary artery calcium scoring in the emergency department: identifying which patients with chest pain can be safely discharged home. Ann Emerg Med. 2010 Sep;56(3):220-9. doi: 10.1016/j.annemergmed.2010.01.017. Epub 2010 Feb 6. PMID: 20138399.
- Nucifora G, Bax JJ, van Werkhoven JM, Boogers MJ, Schuijf JD. Coronary artery calcium scoring in cardiovascular risk assessment. Cardiovascular Therapeutics. 2010; 29(6). https://doi.org/10.1111/j.1755-5922.2010.00172.x
- Chang AM, Le J, Matsuura AC, Litt HI, Hollander JE. Does coronary artery calcium scoring add to the predictive value of coronary computed tomography angiography for adverse cardiovascular events in low-risk chest pain patients? Acad Emerg Med. 2011 Oct;18(10):1065-71. doi: 10.1111/j.1553-2712.2011.01173.x. PMID: 21996072.
- Pursnani A, Chou ET, Zakroysky P, Deaño RC, Mamuya WS, Woodard PK, Nagurney JT, Fleg JL, Lee H, Schoenfeld D, Udelson JE, Hoffmann U, Truong QA. Use of coronary artery calcium scanning beyond coronary computed tomographic angiography in the emergency department evaluation for acute chest pain: the ROMICAT II trial. Circ Cardiovasc Imaging. 2015 Mar;8(3):e002225. doi: 10.1161/CIRCIMAGING.114.002225. Epub 2015 Feb 20. PMID: 25710925; PMCID: PMC4340089.
- Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O’Gara P, Rubin GD. ACCF/SCCT/ACR/aha/ase/ASNC/nasci/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. Circulation. 2010; 122(21).https://doi.org/10.1161/cir.0b013e3181fcae66
- Hoffmann U, Truong QA, Schoenfeld DA, Chou ET, Woodard PK, Nagurney JT, Pope JH, Hauser TH, White CS, Weiner SG, Kalanjian S, Mullins ME, Mikati I, Peacock WF, Zakroysky P, Hayden D, Goehler A, Lee H, Gazelle GS, Wiviott SD, Fleg JL, Udelson JE; ROMICAT-II Investigators. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012 Jul 26;367(4):299-308. doi: 10.1056/NEJMoa1201161. PMID: 22830462; PMCID: PMC3662217.
- Litt HI, Gatsonis C, Snyder B, Singh H, Miller CD, Entrikin DW, Leaming JM, Gavin LJ, Pacella CB, Hollander JE. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012 Apr 12;366(15):1393-403. doi: 10.1056/NEJMoa1201163. Epub 2012 Mar 26. PMID: 22449295.
- Goldstein JA, Chinnaiyan KM, Abidov A, Achenbach S, Berman DS, Hayes SW, Hoffmann U, Lesser JR, Mikati IA, O'Neil BJ, Shaw LJ, Shen MY, Valeti US, Raff GL; CT-STAT Investigators. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol. 2011 Sep 27;58(14):1414-22. doi: 10.1016/j.jacc.2011.03.068. PMID: 21939822.
- Hoffmann U, Bamberg F, Chae CU, Nichols JH, Rogers IS, Seneviratne SK, Truong QA, Cury RC, Abbara S, Shapiro MD, Moloo J, Butler J, Ferencik M, Lee H, Jang IK, Parry BA, Brown DF, Udelson JE, Achenbach S, Brady TJ, Nagurney JT. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol. 2009 May 5;53(18):1642-50. doi: 10.1016/j.jacc.2009.01.052. PMID: 19406338; PMCID: PMC2747766.
- Blaha MJ, Budoff MJ, Tota-Maharaj R, Dardari ZA, Wong ND, Kronmal RA, Eng J, Post WS, Blumenthal RS, Nasir K. Improving the CAC Score by Addition of Regional Measures of Calcium Distribution: Multi-Ethnic Study of Atherosclerosis. JACC Cardiovasc Imaging. 2016 Dec;9(12):1407-1416. doi: 10.1016/j.jcmg.2016.03.001. Epub 2016 Apr 13. PMID: 27085449; PMCID: PMC5055410.
- Tota-Maharaj R, Joshi PH, Budoff MJ, Whelton S, Zeb I, Rumberger J, Al-Mallah M, Blumenthal RS, Nasir K, Blaha MJ. Usefulness of regional distribution of coronary artery calcium to improve the prediction of all-cause mortality. Am J Cardiol. 2015 May 1;115(9):1229-34. doi: 10.1016/j.amjcard.2015.01.555. Epub 2015 Feb 12. PMID: 25743208.
- Ferencik M, Pencina KM, Liu T, Ghemigian K, Baltrusaitis K, Massaro JM, D'Agostino RB Sr, O'Donnell CJ, Hoffmann U. Coronary Artery Calcium Distribution Is an Independent Predictor of Incident Major Coronary Heart Disease Events: Results From the Framingham Heart Study. Circ Cardiovasc Imaging. 2017 Oct;10(10):e006592. doi: 10.1161/CIRCIMAGING.117.006592. PMID: 28956774; PMCID: PMC5659296.
- US Preventive Services Taskforce. (2018). Cardiovascular disease: Risk assessment with Nontraditional Risk Factors. Recommendation: Cardiovascular Disease: Risk Assessment with Nontraditional Risk Factors | United States Preventive Services Taskforce. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cardiovasculardisease-screening-using-nontraditional-risk-assessment
- Alfakih K, Greenwood JP, Plein S. The 2016 update to Nice CG95 guideline for the -investigation of new-onset stable chest pain: More -innovation, but at a cost? Clinical medicine (London, England). 2017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6297566/
- Hecht H, Blaha MJ, Berman DS, Nasir K, Budoff M, Leipsic J, Blankstein R, Narula J, Rumberger J, Shaw LJ. Clinical indications for coronary artery calcium scoring in asymptomatic patients: Expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2017 Mar-Apr;11(2):157-168. doi: 10.1016/j.jcct.2017.02.010. Epub 2017 Feb 24. PMID: 28283309.
- Blaha MJ, Mortensen MB, Kianoush S, Tota-Maharaj R, Cainzos-Achirica M. Coronary Artery Calcium Scoring: Is It Time for a Change in Methodology? JACC Cardiovasc Imaging. 2017 Aug;10(8):923-937. doi: 10.1016/j.jcmg.2017.05.007. PMID: 28797416.
- Urabe Y, Yamamoto H, Kitagawa T, Utsunomiya H, Tsushima H, Tatsugami F, Awai K, Kihara Y. Identifying Small Coronary Calcification in Non-Contrast 0.5-mm Slice Reconstruction to Diagnose Coronary Artery Disease in Patients with a Conventional Zero Coronary Artery Calcium Score. J Atheroscler Thromb. 2016 Dec 1;23(12):1324-1333. doi: 10.5551/jat.35808. Epub 2016 Jul 9. PMID: 27397477; PMCID: PMC5221495.
- Tison GH, Guo M, Blaha MJ, McClelland RL, Allison MA, Szklo M, Wong ND, Blumenthal RS, Budoff MJ, Nasir K. Multisite extracoronary calcification indicates increased risk of coronary heart disease and all-cause mortality: The Multi-Ethnic Study of Atherosclerosis. J Cardiovasc Comput Tomogr. 2015 Sep-Oct;9(5):406-14. doi: 10.1016/j.jcct.2015.03.012. Epub 2015 Apr 7. PMID: 26043963; PMCID: PMC4582663.
- Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Løchen ML, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016 Aug 1;37(29):2315-2381. doi: 10.1093/eurheartj/ehw106. Epub 2016 May 23. PMID: 27222591; PMCID: PMC4986030.