More Information
Submitted: March 11, 2024 | Approved: March 28, 2024 | Published: March 29, 2024
How to cite this article: Rahman T, Tahia KNN. Diagnosing Peripartum Cardiomyopathy in a Resource-Limited Setting, a Clinical Perspective: Case Report. J Cardiol Cardiovasc Med. 2024; 9: 058-060.
DOI: 10.29328/journal.jccm.1001179
Copyright License: © 2024 Rahman T, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Peripartum cardiomyopathy; PPCM; Acute severe pancreatitis; Transthoracic echocardiography; Puerperium; Heart failure; Pregnancy; LV systolic dysfunction; Reduced ejection fraction; Intensive care unit
Diagnosing Peripartum Cardiomyopathy in a Resource-Limited Setting, a Clinical Perspective: Case Report
Tyfur Rahman* and Kazi Nazratun Nomany Tahia
Department of Medicine, Institute of Applied Health Sciences, Foy’s Lake, Chittagong, Bangladesh
*Address for Correspondence: Tyfur Rahman, Department of Medicine, Institute of Applied Health Sciences, Foy’s Lake, Chittagong, Bangladesh, Email: [email protected]
Peripartum cardiomyopathy is a rare case of heart failure with reduced ejection fraction and is considered a diagnosis of exclusion. The symptoms of heart failure in patients with peripartum cardiomyopathy can mimic the physiologic conditions of normal pregnancy. In an acute decompensated state, PPCM can present with acute severe upper abdominal or epigastric pain. We are presenting a 24-year-old female with no personal or family history of heart disease and no identifiable risk factor for PPCM. Based on her initial presentation in the emergency department, a diagnosis of acute severe pancreatitis was sought, and she was referred to the Intensive Care Unit. After further evaluation of the serological tests and imaging, she was eventually diagnosed as a case of PPCM. We emphasize the rare nature of the disease with a diverse presentation which poses a diagnostic challenge, especially in a resource-limited setting where advanced diagnostic tools may be restricted and socioeconomic condition poses a barrier to further patient evaluation. This case exemplifies the infrequent occurrence and atypical manifestation, presenting a learning opportunity for future clinicians.
Peripartum cardiomyopathy (PPCM, also called pregnancy-associated cardiomyopathy is a rare cause of heart failure (HF) that affects women late in pregnancy or in the early puerperium [1-3]. The definition is broad, as the Working Group sought to avoid underdiagnoses of PPCM. All three conditions must be met: development of HF in the last month of pregnancy (or toward the end of pregnancy) or within five months following delivery, absence of another identifiable cause for the HF, left ventricular (LV) systolic dysfunction with an LV ejection fraction (LVEF) of less than 45%, with or without LV dilation [4]. Incidence is higher in African-American women and in women with older maternal age, hypertensive disorders of pregnancy, and multiple gestation pregnancies [5-11]. Symptoms of heart failure mimic those of normal pregnancy, often resulting in a delay in diagnosis and preventable complications [4].
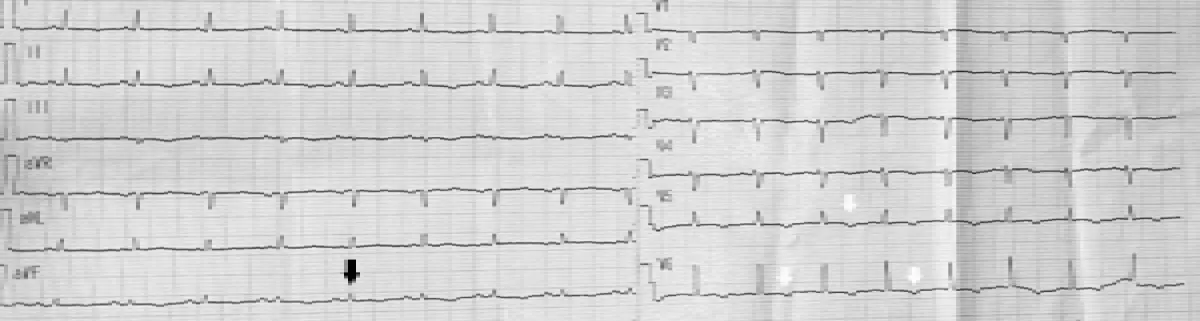
A 24-year-old female, non-diabetic, normotensive presents with severe shortness of breath and epigastric pain for one day in the medicine inpatient department. The patient had generalized weakness and loss of appetite for more than one month preceding her symptoms. There was no associated cough or vomiting. She had a history of cesarean section 2 months back. She has no family history of heart disease or sudden cardiac death. On examination, she exhibited exaggerated use of the muscles of respiration and labored breathing. She had mild anemia and pedal edema. Her blood pressure was 100/50, pulse 84 bpm, and RR 30 breaths/min. The thyroid gland was non-palpable and there was no lymphadenopathy. There was abdominal tenderness in the upper epigastric region. An urgent ECG showed low voltage on all leads and global ischemic changes with inverted T-waves (Figure 1). She was urgently referred to the ICU for respiratory support due to impending respiratory failure from muscle fatigue.
Figure 1: Low voltage (black arrow) and T-wave inversions (white arrows) seen in ECG.
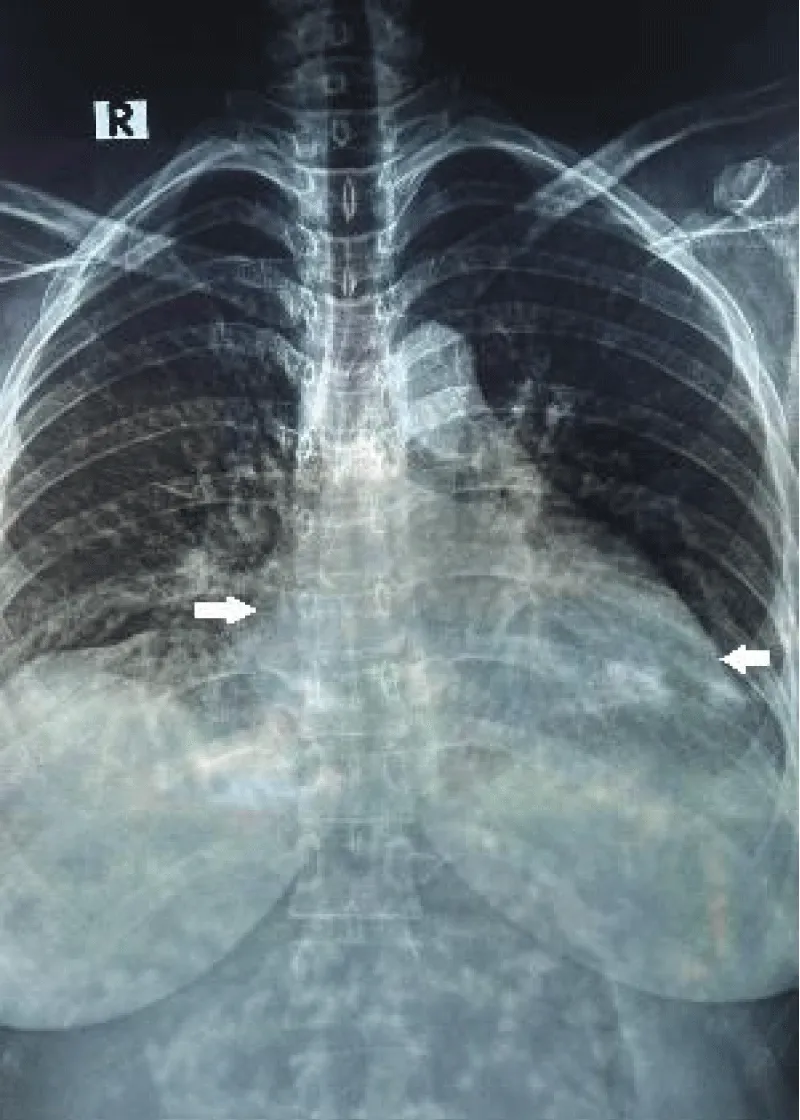
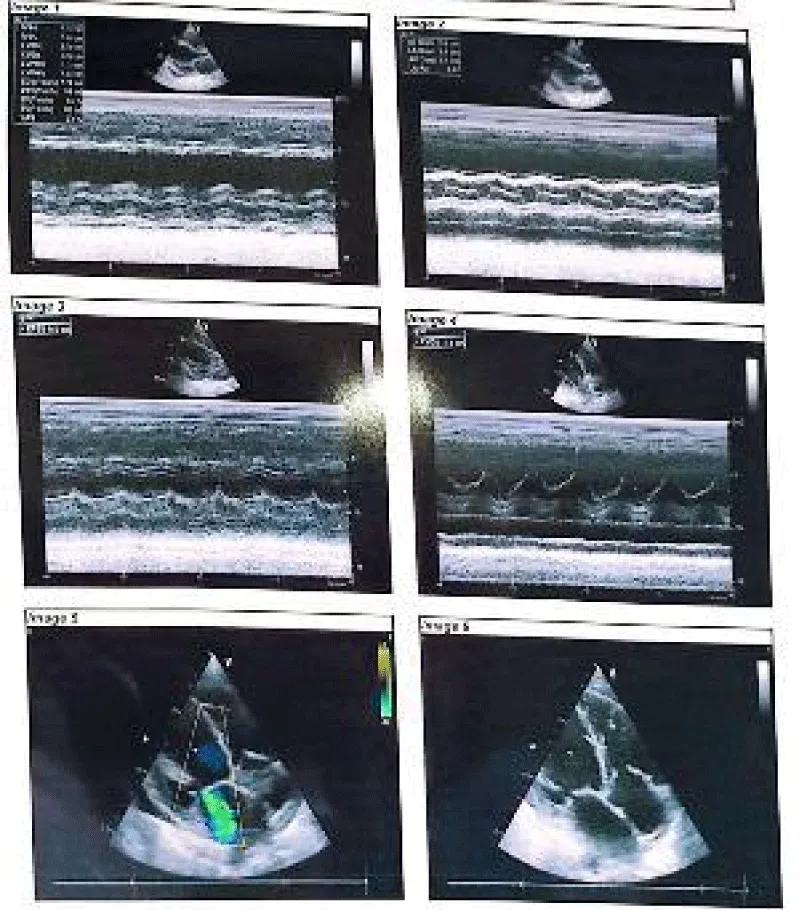
Her complete blood count, lipase, CRP, troponin, electrolytes, creatinine, calcium, magnesium, alkaline phosphatase, and urine routine microscopic examinations were unremarkable. Her bicarbonate level was 17.0 mmol/L and revealed an anion gap of 32.34. The lipid profile was abnormal for triglycerides of 984 mg/dL. Chest x-ray showed cardiomegaly (Figure 2). An echocardiogram showed dilated cardiomyopathy, mild MR, TR, and LV systolic dysfunction-ejection fraction (EF) of 45% (Figure 3). The patient was shifted to the general ward after 2 days upon stabilization. A diagnosis of acute severe pancreatitis was considered initially based on the clinical presentation with peripartum cardiomyopathy as the differential diagnosis. Based on her clinical signs, symptoms, and results of additional tests, the diagnosis of peripartum cardiomyopathy was made. After a consultation with the cardiology department, she was initiated on diuretics, ACEi, Beta Blockers, iron supplementation, empagliflozin, thiamine, and statin. Careful counseling was done regarding contraception and future pregnancies. She was advised to follow up one month later.
Figure 2: Chest X-ray showing cardiomegaly (white arrows, showing increased diameter).
Figure 3: Left ventricular cavity dilated, global hypokinesia with mild TR and MR is noted.
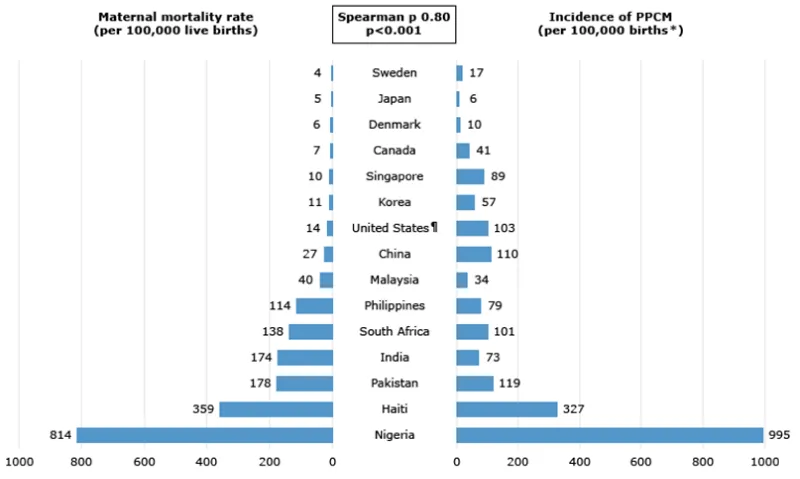
Peripartum cardiomyopathy is a rare (Figure 4) potentially life-threatening disease with varying clinical presentations such as heart failure, chest pain, and arrhythmia, pulmonary and systemic embolism.
Figure 4: Maternal mortality rate and incidence of PPCM in various countries.
Given the rare nature of the disease and the low level of suspicion, its diagnosis goes unnoticed. Additionally, the presentations can coincide with the symptoms of an uneventful pregnancy such as fatigue, shortness of breath, and edema. When evaluating a patient with Peripartum cardiomyopathy, a wide range of differential diagnoses must be considered to avoid overdiagnosis. Careful attention to possible pre-existing heart disease including cardiomyopathies and Valvular heart diseases is important for diagnosing PPCM, which was performed [5]. We diagnosed our patient in Bangladesh, a resource-limited region with low socio-economic status. We advised relevant investigations that allowed us to exclude other conditions and reach our presumptive diagnosis. We evaluated our patient for co-existing heart diseases by comprehensive history taking, review of previous records, and family history. Thromboembolism is the most severe complication, affecting around 6% of patients with PPCM [11]. With no long-term studies, patients with normal LV function (LVEF > 50%) for a period of at least six months, stepwise weaning of the HF regimen with close clinical follow-up (e.g., every three to four months) and with echocardiographic monitoring (e.g., every six months) must be ensured to assess LV function during and for at least one to two years after weaning of HF medications to ensure stability. Management of the patient was done accordingly with plans in light of up-to-date guidelines and research. The patient was counseled regarding the risk of recurrence with subsequent pregnancies, including the option of avoidance of subsequent pregnancy, due to the risk of relapse [12-15]. The mortality rate for PPCM varies with region and ranges from 1.4% to 3.4% within 30 days of diagnosis [16]. Our patient survived with a proper timely approach which led to the improvement of her condition and established our diagnosis of peripartum cardiomyopathy.
A high level of suspicion must be present to diagnose peripartum cardiomyopathy in a postpartum female with severe shortness of breath and upper epigastric pain. This will reduce the risk of life-threatening outcomes. The treatment regimen should also be tailored based on individualized preference and the lactational status of the mother. A multidisciplinary approach including but not limited to cardiology is essential to coordinate care in patients with peripartum cardiomyopathy.
- Davis MB, Arany Z, McNamara DM, Goland S, Elkayam U. Peripartum Cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020 Jan 21;75(2):207-221. doi: 10.1016/j.jacc.2019.11.014. PMID: 31948651.
- Demakis JG, Rahimtoola SH, Sutton GC, Meadows WR, Szanto PB, Tobin JR, Gunnar RM. Natural course of peripartum cardiomyopathy. Circulation. 1971 Dec;44(6):1053-61. doi: 10.1161/01.cir.44.6.1053. PMID: 4256828.
- Pearson GD, Veille JC, Rahimtoola S, Hsia J, Oakley CM, Hosenpud JD, Ansari A, Baughman KL. Peripartum cardiomyopathy: National Heart, Lung, and Blood Institute and Office of Rare Diseases (National Institutes of Health) workshop recommendations and review. JAMA. 2000 Mar 1;283(9):1183-8. doi: 10.1001/jama.283.9.1183. PMID: 10703781.
- Bauersachs J, König T, van der Meer P, Petrie MC, Hilfiker-Kleiner D, Mbakwem A, Hamdan R, Jackson AM, Forsyth P, de Boer RA, Mueller C, Lyon AR, Lund LH, Piepoli MF, Heymans S, Chioncel O, Anker SD, Ponikowski P, Seferovic PM, Johnson MR, Mebazaa A, Sliwa K. Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur J Heart Fail. 2019 Jul;21(7):827-843. doi: 10.1002/ejhf.1493. Epub 2019 Jun 27. PMID: 31243866.
- Mielniczuk LM, Williams K, Davis DR, Tang AS, Lemery R, Green MS, Gollob MH, Haddad H, Birnie DH. Frequency of peripartum cardiomyopathy. Am J Cardiol. 2006 Jun 15;97(12):1765-8. doi: 10.1016/j.amjcard.2006.01.039. Epub 2006 Apr 21. PMID: 16765131.
- Brar SS, Khan SS, Sandhu GK, Jorgensen MB, Parikh N, Hsu JW, Shen AY. Incidence, mortality, and racial differences in peripartum cardiomyopathy. Am J Cardiol. 2007 Jul 15;100(2):302-4. doi: 10.1016/j.amjcard.2007.02.092. Epub 2007 Jun 6. PMID: 17631087.
- Gentry MB, Dias JK, Luis A, Patel R, Thornton J, Reed GL. African-American women have a higher risk for developing peripartum cardiomyopathy. J Am Coll Cardiol. 2010 Feb 16;55(7):654-9. doi: 10.1016/j.jacc.2009.09.043. PMID: 20170791; PMCID: PMC3814012.
- Harper MA, Meyer RE, Berg CJ. Peripartum cardiomyopathy: population-based birth prevalence and 7-year mortality. Obstet Gynecol. 2012 Nov;120(5):1013-9. doi: 10.1097/aog.0b013e31826e46a1. PMID: 23090517.
- Irizarry OC, Levine LD, Lewey J, Boyer T, Riis V, Elovitz MA, Arany Z. Comparison of Clinical Characteristics and Outcomes of Peripartum Cardiomyopathy Between African American and Non-African American Women. JAMA Cardiol. 2017 Nov 1;2(11):1256-1260. doi: 10.1001/jamacardio.2017.3574. PMID: 29049825; PMCID: PMC5815055.
- Elkayam U, Akhter MW, Singh H, Khan S, Bitar F, Hameed A, Shotan A. Pregnancy-associated cardiomyopathy: clinical characteristics and a comparison between early and late presentation. Circulation. 2005 Apr 26;111(16):2050-5. doi: 10.1161/01.CIR.0000162478.36652.7E. PMID: 15851613.
- Chirillo F, Baritussio A, Cucchini U, Toniolli E, Polo A, Iavernaro A. Challenges in the diagnosis of peripartum cardiomyopathy: a case series. Eur Heart J Case Rep. 2021 Feb 16;5(2):ytab001. doi: 10.1093/ehjcr/ytab001. PMID: 33738415; PMCID: PMC7954255.
- Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E, Regitz-Zagrosek V, Schaufelberger M, Tavazzi L, van Veldhuisen DJ, Watkins H, Shah AJ, Seferovic PM, Elkayam U, Pankuweit S, Papp Z, Mouquet F, McMurray JJ; Heart Failure Association of the European Society of Cardiology Working Group on Peripartum Cardiomyopathy. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J Heart Fail. 2010 Aug;12(8):767-78. doi: 10.1093/eurjhf/hfq120. PMID: 20675664.
- Elkayam U, Tummala PP, Rao K, Akhter MW, Karaalp IS, Wani OR, Hameed A, Gviazda I, Shotan A. Maternal and fetal outcomes of subsequent pregnancies in women with peripartum cardiomyopathy. N Engl J Med. 2001 May 24;344(21):1567-71. doi: 10.1056/NEJM200105243442101. Erratum in: N Engl J Med 2001 Aug 16;345(7):552. PMID: 11372007.
- Sutton MS, Cole P, Plappert M, Saltzman D, Goldhaber S. Effects of subsequent pregnancy on left ventricular function in peripartum cardiomyopathy. Am Heart J. 1991 Jun;121(6 Pt 1):1776-8. doi: 10.1016/0002-8703(91)90025-d. PMID: 2035390.
- Codsi E, Rose CH, Blauwet LA. Subsequent Pregnancy Outcomes in Patients With Peripartum Cardiomyopathy. Obstet Gynecol. 2018 Feb;131(2):322-327. doi: 10.1097/AOG.0000000000002439. PMID: 29324614.
- Sliwa K, Mebazaa A, Hilfiker-Kleiner D, Petrie MC, Maggioni AP, Laroche C, Regitz-Zagrosek V, Schaufelberger M, Tavazzi L, van der Meer P, Roos-Hesselink JW, Seferovic P, van Spandonck-Zwarts K, Mbakwem A, Böhm M, Mouquet F, Pieske B, Hall R, Ponikowski P, Bauersachs J. Clinical characteristics of patients from the worldwide registry on peripartum cardiomyopathy (PPCM): EURObservational Research Programme in conjunction with the Heart Failure Association of the European Society of Cardiology Study Group on PPCM. Eur J Heart Fail. 2017 Sep;19(9):1131-1141. doi: 10.1002/ejhf.780. Epub 2017 Mar 8. PMID: 28271625.