More Information
Submitted: 12 August 2019 | Approved: 16 August 2019 | Published: 19 August 2019
How to cite this article: Benlafqih C, Bouhdadi H, Bakkali A, Rhissassi J, Sayah R, et al. Late discover of a traumatic cardiac injury: Case report. J Cardiol Cardiovasc Med. 2019; 4: 100-102.
DOI: 10.29328/journal.jccm.1001048
Copyright License: © 2019 Benlafqih C, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Cardiac injury; Traumatic mitral regurgitation; Ventricular septal defect
Late discover of a traumatic cardiac injury: Case report
Benlafqih C, Bouhdadi H*, Bakkali A, Rhissassi J, Sayah R and Laaroussi M
Cardiovascular Surgery A, Ibn Sina Hospital, Rabat, Morocco
*Address for Correspondence: Hanae Bouhdadi, Cardiovascular Surgery A, Ibn Sina Hospital, Rabat, Morocco, Tel: 00212 676155494; Email: [email protected]
Blunt chest trauma leads to a wide range of lesions, relatively minor parietal injuries to potentially fatal cardiac lesions, making diagnosis and management difficult. The diagnosis is currently facilitated by imaging, however, these lesions may go unnoticed and be discovered late through complications.
We report the case of a neglected heart wound revealed by a heart failure. This case is notable due to a favourable outcome despite a delay in diagnosis due to a lack of pericardial effusion and the absence of cardiac symptoms, and a long delay from injury to appropriate treatment in the presence of a penetrating cardiac wound deep enough to cause a muscular ventricular septal defect and lacerate the anterior mitral leaflet.
Penetrating cardiac injury is rare and frequently not survivable. Significant haemorrhage resulting in cardiac tamponade commonly ensues. Such cardiac tamponade is a clear clinical, radiological and sonographic indicator of significant underlying injury. In the absence of cardiac tamponade, diagnosis can be more challenging [1]. We present the case of a neglected cardiac injury, resulting in a mitral valve regurgitation and ventricular septal defect, discovered forty five days after the initial trauma in a 25-year-old man presenting with signs of heart failure.
We present the case of a 25-year-old patient. Admitted to the emergency department of Ibn Sina Hospital for a class III dyspnea. In his medical history there is the notion of epigastric penetrating wound by a 3-cm knife forty five days earlier. Four days after the initial trauma, a radiological examination showed an abdominal effusion, which led to an exploratory laparotomy that did not show any underlying lesions.
The clinical examination found an orthopneic patient, polypneic at 32 cycles / min with a heart rate at 120b / min. The blood pressure was 120/80 mmHg, giant V waves in his neck upon jugular venous pulse examination and edema of the lower limbs. The abdominal examination revealed a laparotomy scar and hepatomegaly, a shudder was palpable at the apex. The heart sounds were slightly muffled, a systolic murmure was perceived at the apex. Pulmonary auscultation found bilateral crackles and a syndrome of fluid effusion.
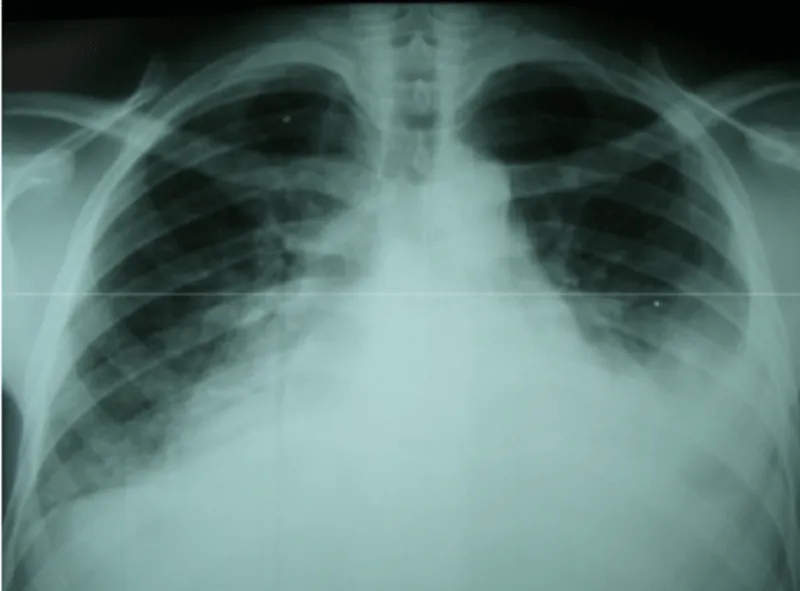
The electrocardiogram recorded a regular sinus rhythm. The X-ray showed a more marked bilateral effusion on the left, flaky opacities at the two hiles and cardiomegaly (Figure 1).
Figure 1: Chest X-ray showing alveolar edema, pleural effusion and enlarged cardiac silhouette.
The biological assessment showed anemia at 10.5 g / dl of hemoglobin, 11800 / mm3 hyperleucocytosis and 77.9 mg / l of reactive protein C. Transthoracic echocardiography (TTE) showed a pericardial effusion with compression of the right atrium, a defect in the anterior mitral valve with very high filling pressures and a dilated left ventricle, and a ventricular septal defect (VSD).
Surgery was indicated and performed within the forty eight hours following diagnosis.
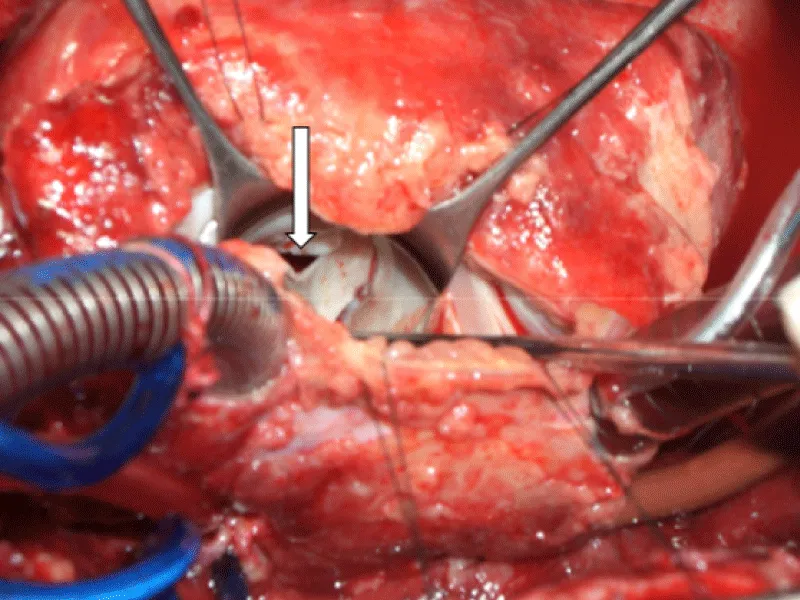
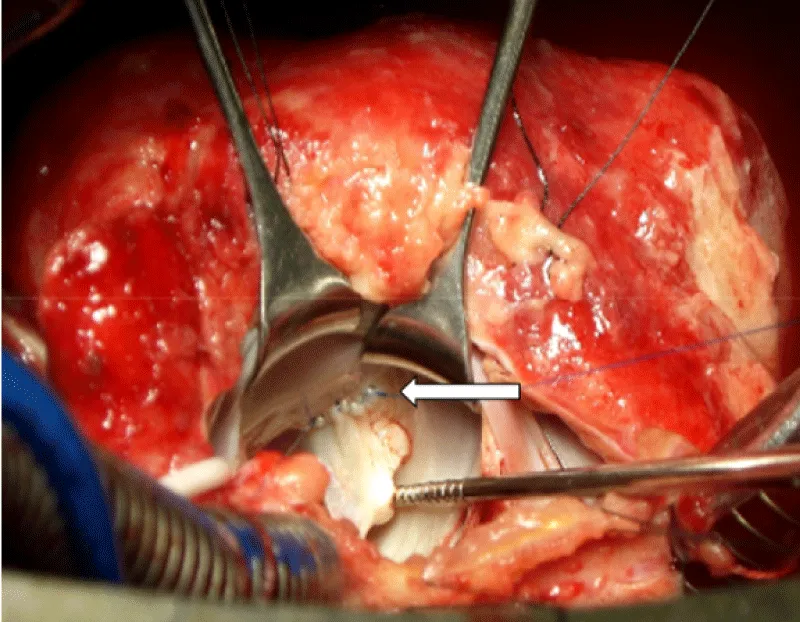
After sternotomy and opening of the pericardium which was thickened, an effusion with false membranes is revealed. There was no obvious bleeding point, and the point of break-in could not be objectified. After initiation of routine cardiopulmonary bypass, aortic cross-clamping and adequate myocardial protection, the mitral valve was exposed through a trans-septal approach, we revealed a 2 cm perforation in the anterior mitral valve (Figure 2). After suturing the defect (Figure 3), we proceeded to posterior mitral ring reduction by suture annuloplasty.
Figure 2: Perforation of the body of the anterrior mitral valve (white arrow).
Figure 3: Continious suture of the tear of large mitral valve using 6-0 prolene (white arrow).
The subvalvular apparatus was undamaged.
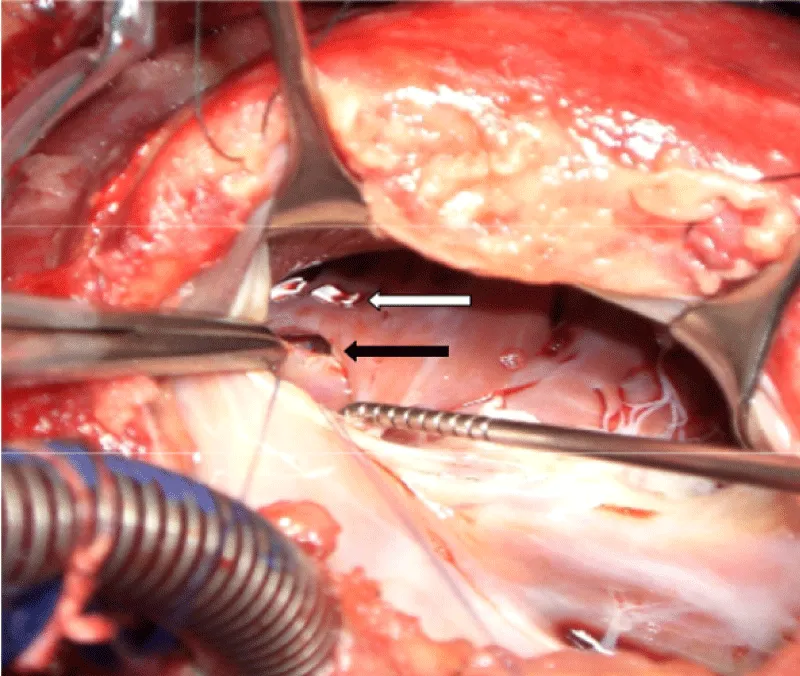
The VSD was closed by two interrupted pledgeted prolene sutures (Figure 4).
Figure 4: Closure of the VSD (black arrow) by two interrurpted pledgeted prolene sutures (white arrow).
Postoperative course was uneventful.
TTE showed a competent mitral valve and no residual shunt.
Follow-up at six months finds an asymptomatic patient.
Penetrating cardiac injury is one of the most lethal medical emergencies, with an estimated pre-hospital mortality rate of 94% and a subsequent in-hospital mortality rate of 50% among initial survivors. In a 10-year consecutive cohort of chest trauma victims with penetrating cardiac injuries from a major Scandinavian trauma center, approximately 50% died before reaching the hospital. Of the patients reaching the trauma center, the mortality was 50% despite high intensity of care. A predictor for survival was signs of life in the emergency room [2].
Initial clinical examination together with analysis of the trauma mechanism will provide vital information on potential severity and location of the injury. If the extent of the injury remains undetermined and the condition of the patient permits, imaging can provide further information [3].
In penetrating chest trauma, both ventricles are injured with similar frequency, but the RV is the most common site of entry because it forms most of the anterior surface of the heart. The most frequent trauma scenario is a young man who presents with a precordial stabbing or thoracic gunshot wound.
The initial manifestation is commonly cardiac tamponade and, depending on the haemodynamic stability of the patient, immediate surgical intervention may be necessary without further evaluation [4]. In the absence of cardiac tamponade, diagnosis can be more challenging. In this case of a 25-year old man stabbed, a significant pericardial effusion and cardiac tamponade did not occur despite an injury transversing the pericardium.
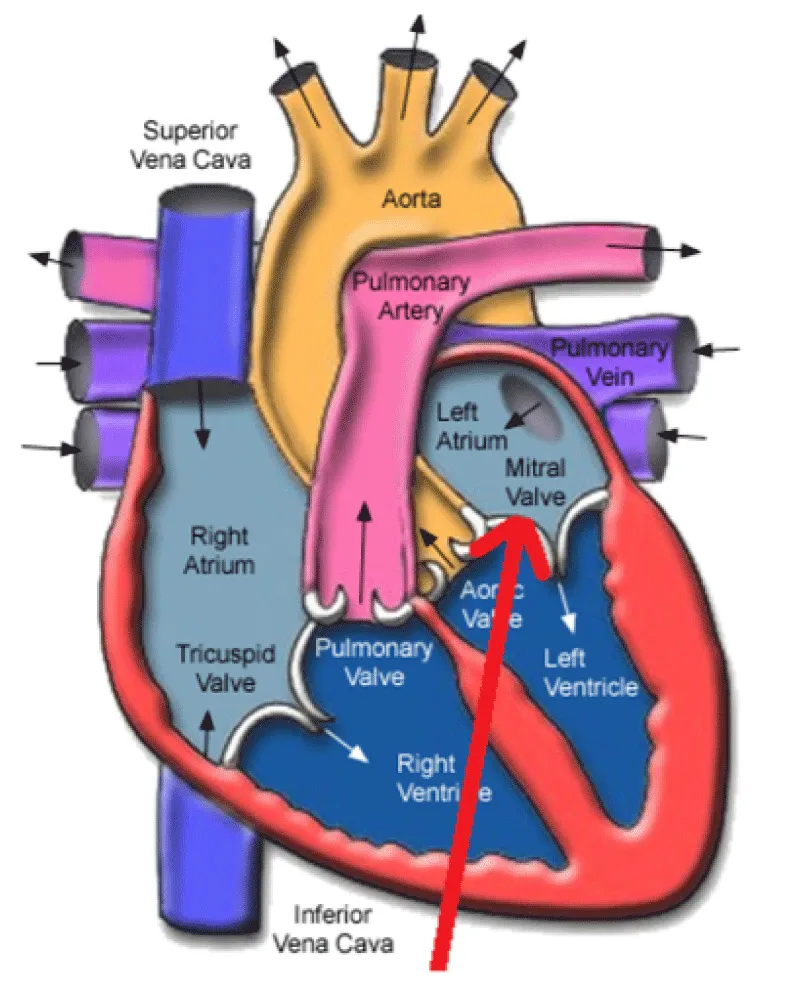
In our case, the epigastric wound was directed towards the thorax, passing through the diaphragm, then the right ventricle, the interventricular septum, and the anterior mitral valve (Figure 5).
The peritoneal effusion, mistaken for a hemoperitoneum, was actually, and given the context, an ascite secondary to ventricular dysfunction. Its discovery should have alerted the surgeon for more investigations.
Figure 5: Red arrow: presumed path of the white weapon.
This case highlights the importance of a high index of suspicion for cardiac injury based on the mechanism, even in the absence of pericardial tamponade. In front of any wound in the epigastric region, cardiac involvement should be evoked. The possibility of septal defect or valvular lesion requires special attention and constant concern of the trauma team.
- Connelly TM, Kolcow W, Veerasingam D, DaCosta M. A severe penetrating cardiac injury in the absence of cardiac tamponade. Interact Cardiovasc Thorac Surg. 2017; 24: 286-287. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27789730
- Kaljusto ML, Skaga NO, Pillgram-Larsen J, Tønnessen T. Survival predictor for penetrating cardiac injury; a 10-year consecutive cohort from a scandinavian trauma center. Scand J Trauma Resusc Emerg Med. 2015; 23. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26032760
- Christie-Large M, Michaelides D, James S. Focused assessment with sonography for trauma: the FAST scan. Trauma. 2008; 10: 93-101.
- Leite L, Gonçalves L, Vieira DN. Cardiac injuries caused by trauma: Review and case reports. J Forensic Leg Med. 2017; 52: 30-34. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28850860