More Information
Submitted: March 29, 2022 | Approved: April 25, 2022 | Published: April 26, 2022
How to cite this article: Moreno-Monsalve T, Frutos-Esteban L, Navarro-Fernández JL, Mohamed-Salem L, Castellón-Sánchez MI, et al. FDG PET/CT of uncommon cardiac angiosarcoma with bone metastases: a case report. J Cardiol Cardiovasc Med. 2022; 7: 036-039.
DOI: 10.29328/journal.jccm.1001130
Copyright License: © 2022 Moreno-Monsalve T, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
FDG PET/CT of uncommon cardiac angiosarcoma with bone metastases: a case report
Tatiana Moreno-Monsalve*, Laura Frutos-Esteban, Jose Luis Navarro-Fernández, Laroussi Mohamed-Salem, María Isabel Castellón-Sánchez, Ana Cristina Hernández-Martínez, Tomas Rodríguez-Locarno and Jose Fulgencio Contreras-Gutierrez
Department of Nuclear Medicine, Virgen de la Arrixaca University Clinical Hospital, Murcia, Spain
*Address for Correspondence: Tatiana Moreno-Monsalve, Spanish Society of Nuclear Medicine and Molecular Imaging, Spain, Email: [email protected]
Cardiac angiosarcomas are rare malignant neoplasms with an aggressive clinical course. These are characterized by the absence of specific clinical findings, rapid growth with frequent metastasis at the time of diagnosis, correlated with poor prognosis, and reduced response to treatment. But with early diagnosis, more possibilities for treatment and survival can be provided. We report the case of a young woman diagnosed with right atrial angiosarcoma locally advanced with bone metastases detected by 18F-FDG PET/CT, which revealed distant disease extent at diagnosis, consequently, chemotherapy was started.
Primary cardiac angiosarcomas are aggressive malignant tumors with high rates of local infiltration as well as systemic metastases and are often associated with poor prognosis [1]. These tumors are considered so rare that they are often misdiagnosed on initial examination. Hence the difficulty of offering standardized treatments [1].
The clinical manifestations of primary cardiac angiosar-comas are not specific. These depend on their infiltration into the myocardium and adjacent structures, in addition to the extent of metastases [2]. Thus, early and accurate detection and staging of the disease by imaging can lead to early treatment.
Furthermore, previous studies have shown that neo-adjuvant chemotherapy, local radical resection, postoperative radiation therapy, and targeted therapy can prolong the survival rate [1].
A 26-year-old patient, with a history of microcephaly and growth retardation, but no other relevant personal or family history, was admitted to cardiology due to progressive deterioration of the general condition, asthenia, and edema of the lower limbs. A Transthoracic echocardiogram showed a slightly enlarged right atrium, a mass-like lesion (3 cm2) in its cavity, and moderate pericardial effusion, associated with signs of hemodynamic compromise. An evacuation pericardiocentesis was performed. Cytology examinations of the pericardial effusion indicated sero-hemorrhagic fluid with the presence of mesothelial cells.
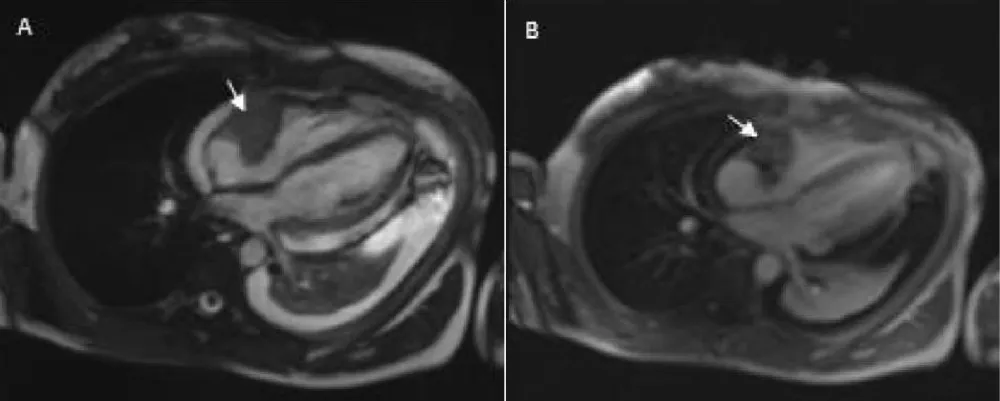
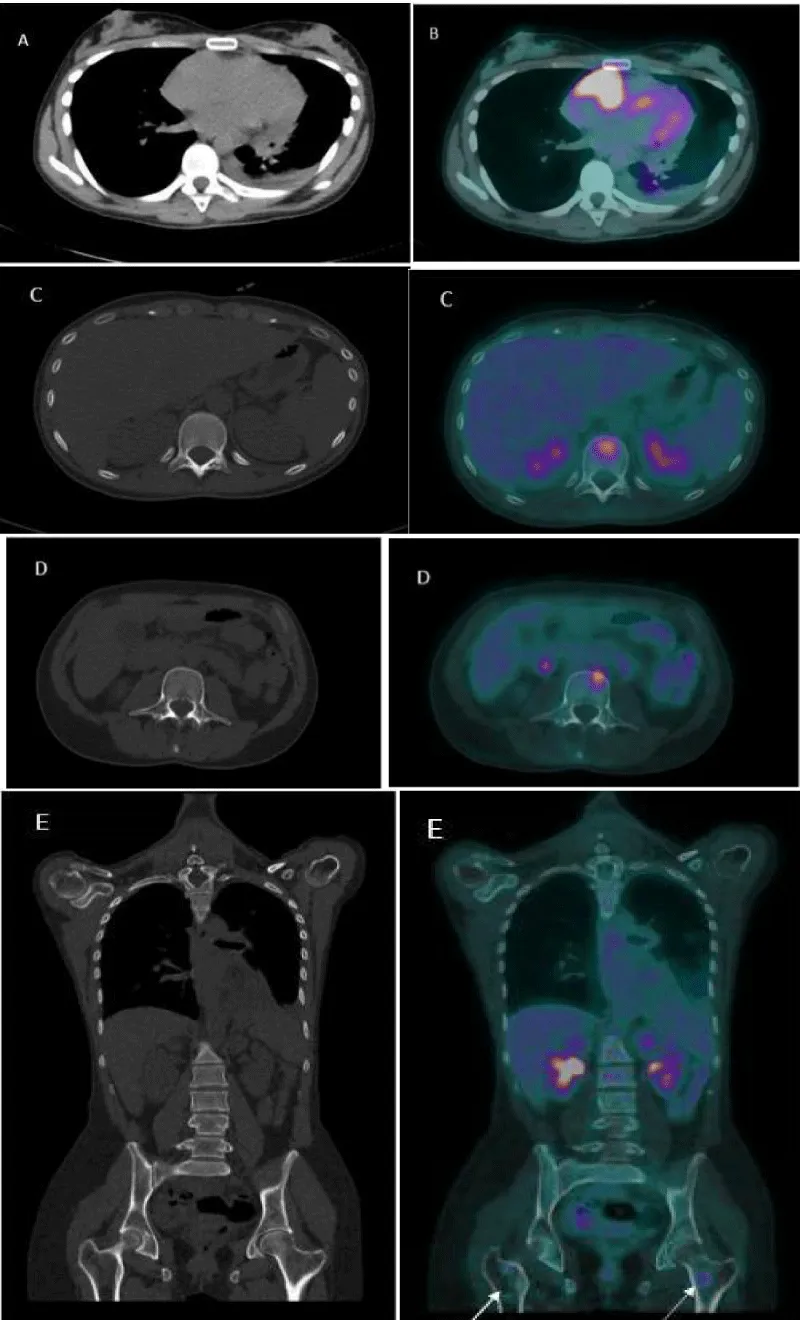
To better delineate and characterize the cardiac mass, a chest CT was performed (Figure 1). This examination revealed moderate pericardial effusion with the existence of a low attenuation mass in the right atrium, extending along the pericardium with heterogeneous enhancement, of approximately 3.5 cm, which corresponds to a cardiac tumor. Cardiac magnetic resonance imaging (Figure 2) exposed a cardiac mass at the level of the right atrium with extension into the pericardium and free wall of the right ventricle and heterogeneous late enhancement, being hypointense on T1 and T2, This is not the most typical pattern, which usually consists of low signal T1-weighted sequences, and increased signal and central areas of hyperintensity on T2weighted, consistent with hemorrhage and necrosis, and areas of moderate signal intensity in more peripheral regions [3]. Because of their high vascularity, strong signal enhancement is seen after the administration of IV gadolinium [3]. However, given the propensity of angiosarcomas to necrosis and hemorrhage, these often have heterogeneous signals on cardiac MR images [3]. Fluorodeoxyglucose-18 combined with positron emission tomography/computed tomography (18F-FDG-PET/CT) (Figure 3) confirmed pathological metabolic activity in the recognized mass in the right atrium extending along the pericardium with intensely increased FDG uptake (SUVmax) of 17.3. Moderate Pericardial effusion was noted and multiple hypermetabolic foci in the bodies of the D12, L2, and L3 vertebrae, as well as in the proximal third of both femurs, without evidence of structural lesions on CT with SUVmax of 6.9.
Figure 1: Arterial phase chest CT. Findings: Right atrial mass with heterogeneous centripetal enhancement (arrow) and pericardial effusion.
Figure 2: Cardiac MRI findings: A: Axial T2-weighted images mass in the right atrium hypointense on T2 with extension into the pericardium and free wall of the right ventricle (arrow) B: Axial T1weighted image after administration of gadolinium shows heterogeneous late enhancement of the right atrial mass (arrow).
Figure 3: An 18F-FDG-PET/CT scan. A computed tomography (CT) and B fused PET/CT: Pathological metabolic activity in the known mass in the right atrium extending along the pericardium with intensely increased FDG uptake (SUVmax) of 17.3. Moderate Pericardial effusion was noted. C, D, E (CT and fused PET/TC) showed hypermetabolic foci in the bodies of the D12 and L3 vertebrae, as well as in the proximal third of both femurs (arrows), without evidence of structural lesions on CT with SUVmax of 6.9.
The radiological appearance of a mass with extensive local infiltration and the presence of secondary lesions on PET/CT was highly suggestive of a metastatic cardiac tumor. Consequently, a biopsy of the cardiac lesion was performed. The histopathological examination confirmed the existence of primary cardiac angiosarcoma. Microscopic findings showed that the tumor was composed of frequent slit-like vascular channels and hyperchromatic, elongated cells with moderate nuclear atypia. The immunohistochemical analysis revealed that tumor cells stained positive for CD31, CD34, VI antigen, and vimentin, with nuclear expression of ERG and FLI1, which confirmed the endothelial origin of the tumor.
Due to the suspicion of bone metastases, the study was completed with a bone biopsy of the vertebral lesions, which in turn proved the existence of metastatic disease.
Considering the definitive diagnosis of cardiac angiosarcoma locally advanced with bone metastases, urgent chemotherapy with weekly paclitaxel was started. The refractory pericardial effusion and the signs of hemodynamic compromise disappeared within 7 days, the patient was discharged from the hospital (ECOG-PS of 1) and completed the chemotherapy regimen in an outpatient clinic.
Primary cardiac sarcoma is an extremely rare subtype of soft tissue sarcoma [2]. It has an autopsy incidence of approximately 0.001% – 0.03% and an overall incidence of 0.007% [2].
Cardiac angiosarcomas (CAS) originate from vascular endothelial or vascular endothelial cells that differentiate from mesenchymal ones [4]. These tumors grow rapidly and are highly aggressive, often associated with the presence of metastases at the time of diagnosis (66% to 89%), and their etiology is still not fully understood [5].
Definitive risk factors include chronic lymphedema, radiation exposure, and a history of contact with environ-mental carcinogens [2]. Several family reports of cardiac angiosarcoma have indicated its genetic association [2].
Most (90%) locate in the right atrium, originating from its lateral wall, and the septum is rarely affected. The second most frequent spot is the left atrium, followed by the right ventricle and the left ventricle [5].
Early diagnosis of angiosarcoma is still very difficult and its clinical manifestations are atypical; often surfacing signs such as chest tightness, shortness of breath, arrhythmia, or symptoms of distal metastasis [6]. Extension to the peri-cardium is common and usually associated with the formation of massive, hemorrhagic, and recurrent effusions, with or without cardiac tamponade [5].
Angiosarcomas most commonly metastasize to the lungs, although secondary lesions have also been identified in other organs, including the liver, lymph nodes, brain, bones, spleen, adrenal glands, pleura, diaphragm, kidneys, thyroid, intestine, and skin [5].
Imaging tests are essential when studying a cardiac mass. Both the treatment to be administered and the course of the disease are directly conditioned by the initial stage and particularly the results obtained in the initial imaging tests, which in turn lead to risk stratification.
Echocardiography has become the gold standard for the primary evaluation of a cardiac neoplasm, although it is both operator and acoustic windows dependent [5].
CT and MRI are better able to delineate and characterize these tumors and provide accurate details about local spread and involvement of adjacent structures [5].
18F-FDG-PET/CT is not routinely considered in the general staging protocol for this tumor type. However, due to its high metabolic rate, this technique has reasonably high global sensitivity and specificity values in the detection of metastatic disease between 80% and 90% respectively [6], allowing early detection of distant disease, as in the case of our patient.
Histological examination establishes the definitive diag-nosis. Angiosarcomas are composed of cells with endo-thelial or fusiform morphology with a malignant appearance and hyperchromaticnuclei [5].
The treatment of primary cardiac tumors remains contro-versial. Still, surgery plays an essential role in the context of localized disease, with or without adjuvant chemotherapy or radiotherapy [4].
Complete surgical excision is the most important prognostic factor. However, this is rarely possible due to the extensive local dissemination and the large size of the tumor mass [5], as in our clinical case, where there was distant involvement at the time of diagnosis. Thus, chemotherapy remains the best option for unresectable situations.
The median survival associated with cardiac angiosarcoma is very low, ranging from 6 to 11 months, regardless of treatment [5]. However, early detection and an aggressive approach may have a more favorable outcome, leading to a prolongation of survival beyond one year [5]. Case in point, chemotherapy has been of limited benefit in prolonging quality of life.
This clinical case demonstrates the importance of considering a primary cardiac neoplasm in the differential diagnosis of young patients suffering from pericardial effusion and non-specific symptoms related to local tumor growth (change in cardiac flow) that affect the pericardium and neighboring structures, as took place in the case of our patient.
The use of non-invasive imaging modalities for a comprehensive analysis of tumor characteristics may improve the early detection of cardiac neoplasms and may provide a specific classification before histopathological analysis [2].
Therefore, clinicians must have an appropriate high index of suspicion and formulate a diagnostic investigation for primary cardiac angiosarcomas [1]. Early diagnosis and correct classification and staging of patients by both morphological and metabolic imaging techniques in the case of PET/CT, has the potential to improve treatment planning, prevent tumor progression and metastasis in certain cases, and even provide opportunities for further treatment [1].
- Kurian KC, Weisshaar D, Parekh H, Berry GJ, Reitz B. Primary cardiac angiosarcoma: case report and review of the literature. Cardiovasc Pathol. 2006; 15: 110-112. PubMed: https://pubmed.ncbi.nlm.nih.gov/16533700/
- Chen Y, Li Y, Zhang N, Shang J, Li X, et al. Clinical and Imaging Features of Primary Cardiac Angiosarcoma. Diagnostics (Basel, Switzerland). 2020; 10: 776. PubMed: https://pubmed.ncbi.nlm.nih.gov/33008011/
- O'Donnell DH, Abbara S, Chaithiraphan V, Yared K, Killeen RP, et al. Cardiac tumors: optimal cardiac MR sequences and spectrum of imaging appearances. Am J Roentgenol. 2009; 193: 377–387. PubMed: https://pubmed.ncbi.nlm.nih.gov/19620434/
- Zhang C, Huang C, Zhang X, Zhao L, Pan D. Clinical characteristics associated with primary cardiac angiosarcoma outcomes: a surveillance, epidemiology, and end result analysis. Eur J Med Res. 2019; 24: 29. PubMed: https://pubmed.ncbi.nlm.nih.gov/31426842/
- Saraiva F, Antunes M, Providência LA. Cardiac angiosarcoma in a pregnant woman: a case report and review of the literature. Acta Cardiol. 2012; 67: 727–731. https://pubmed.ncbi.nlm.nih.gov/23393946/
- Gabriel M, Rubello D. 18F-FDG PET-CT in soft tissue sarcomas: staging, restaging, and prognostic value? Nucl Med Commun. 2016; 37: 3–8. PubMed: https://pubmed.ncbi.nlm.nih.gov/26457597/