More Information
Submitted: April 22, 2024 | Approved: May 11, 2024 | Published: May 13, 2024
How to cite this article: Karuru UD, Tummala SR, Naveen T, Kanjerla KK, Gautam PS, et al. Non-surgical Techniques for Combined Rheumatic Severe Aortic and Mitral Stenosis – Case Series and Brief Review of Literature. J Cardiol Cardiovasc Med. 2024; 9: 073-080.
DOI: 10.29328/journal.jccm.1001182
Copyright License: © 2024 Karuru UD, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Rheumatic heart disease; Mitral stenosis; Aortic stenosis; Percutaneous transvenous mitral commissurotomy; Balloon aortic valvotomy; Transcatheter aortic valve replacement
Non-surgical Techniques for Combined Rheumatic Severe Aortic and Mitral Stenosis – Case Series and Brief Review of Literature
Uma Devi Karuru, Sadanand Reddy Tummala*, Naveen T, Kiran Kumar Kanjerla, Gautam PS and Sai Kumar Mysore
Department of Cardiology, ESIC Medical College and Super-Speciality Hospital, Hyderabad, India
*Address for Correspondence: Dr. Sadanand Reddy Tummala, Professor & Head, Department of Cardiology, ESIC Medical College and Super-Speciality Hospital, Hyderabad, India, Email: [email protected]
Rheumatic heart disease persists as a significant concern in developing regions, often resulting in multivalvular heart conditions. Treatment options are limited, though percutaneous transvenous mitral commissurotomy effectively addresses rheumatic mitral stenosis. Non-surgical interventions for aortic stenosis include balloon aortic valvotomy and Transcatheter aortic valve replacement (TAVR), tailored to patient factors like age and comorbidities.
We describe two cases of Rheumatic multivalvular disease which were managed non-surgical. The first case is a pioneering procedure performed on a young patient combined percutaneous transvenous mitral commissurotomy with balloon aortic valvotomy, guided by 4-dimensional transoesophageal echocardiography (4D TEE). This represents the first documented instance in medical literature, showcasing the potential of integrated interventions and advanced imaging techniques. In the second challenging case involving a heavily calcified, retrovirus, and Hepatitis B positive 55-year-old, a staged approach was adopted, involving percutaneous transvenous mitral commissurotomy followed by Transcatheter aortic valve replacement (TAVR). Despite complexities, this sequential strategy demonstrates the adaptability of transcatheter techniques in managing complex valvular pathologies.
These cases highlight the evolving landscape of interventional cardiology and underscore the importance of tailored, multidisciplinary approaches in optimizing outcomes for patients with rheumatic heart disease and multivalvular involvement, especially in resource-limited settings. Further exploration and dissemination of such innovative strategies hold promise for enhancing cardiac care quality and expanding treatment options globally.
Rheumatic heart disease (RHD) remains a pressing concern in developing countries, often leading to multivalvular heart disease. The limited treatment guidelines for such conditions underscore the medical complexities involved. Percutaneous transvenous mitral commissurotomy has emerged as a vital technique for addressing Rheumatic mitral stenosis, offering a means to postpone mitral valve replacement and thereby avoiding the need for long-term anticoagulation and regular blood tests for optimization.
In the realm of aortic stenosis, non-surgical options like balloon aortic valvotomy and Transcatheter aortic valve replacement (TAVR) provide alternatives based on factors such as age, valve anatomy, comorbidities, surgical risk, and patient preference. However, the prospect of double valve replacement presents considerable surgical mortality risks, subsequent lifestyle modifications, and the ongoing need for stringent monitoring to ensure optimal anticoagulation, all of which can place significant financial strain on both patients and healthcare systems, particularly in resource-poor settings and economically deprived populations.
To address these challenges, non-surgical methods offer promise in improving patient outcomes while alleviating the burdens associated with traditional surgical interventions. Herein, we present two unique cases demonstrating innovative approaches to valvular disease management:
1. Simultaneous balloon valvotomy for both the aortic and mitral valves in a young patient.
2. A staged intervention involving balloon mitral valvotomy followed by Transcatheter aortic valve replacement (TAVR) in a 55-year-old patient.
These cases not only showcase the efficacy of non-surgical interventions but also underscore the importance of tailored, multidisciplinary approaches in optimizing outcomes for patients with multivalvular heart disease, particularly in resource-limited settings. By reducing surgical risks and long-term management complexities, these methods hold promise for enhancing patient care and alleviating healthcare system burdens worldwide.
Presentation history
A 28-year-old gentleman presented to our center with complaints of exertional dyspnea, which progressed from NYHA class I to NYHA class III over a 2-year period, along with easy fatiguability, dizziness, and poor exercise capacity. He worked as a construction worker.
Past medical history
He had no known history of hypertension, diabetes, or alcohol use.
Investigations
His hemogram, liver function tests (LFT), renal function tests (RFT), and lipid profile were normal. Viral markers were negative. Electrocardiography (ECG) indicated normal sinus rhythm, left atrial (LA) enlargement, and left ventricular hypertrophy (LVH) with a strain pattern. Chest X-ray revealed mild cardiomegaly, LA enlargement, and mild pulmonary venous hypertension (PVH). Two-dimensional Echocardiography (2D ECHO) showed rheumatic heart disease (RHD), severe mitral stenosis (MS), and severe aortic stenosis (AS) with normal biventricular function. Considering his young age, suitable valve anatomy, sinus rhythm, and freedom from anticoagulation, he was considered for concurrent balloon mitral valvotomy (BMV) and balloon aortic valvotomy (BAV).
Management
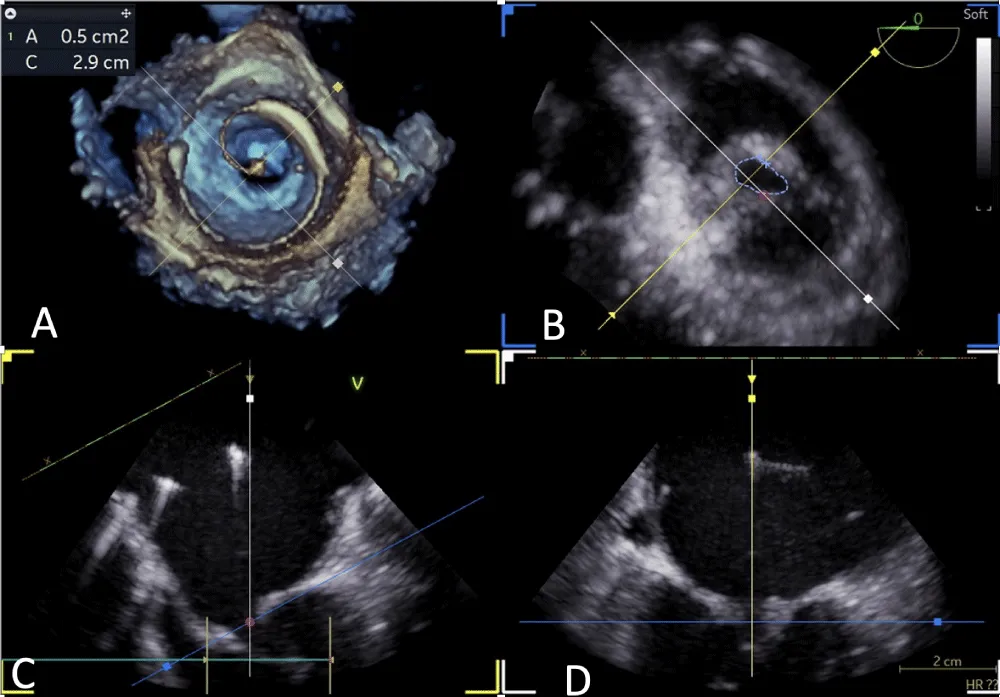
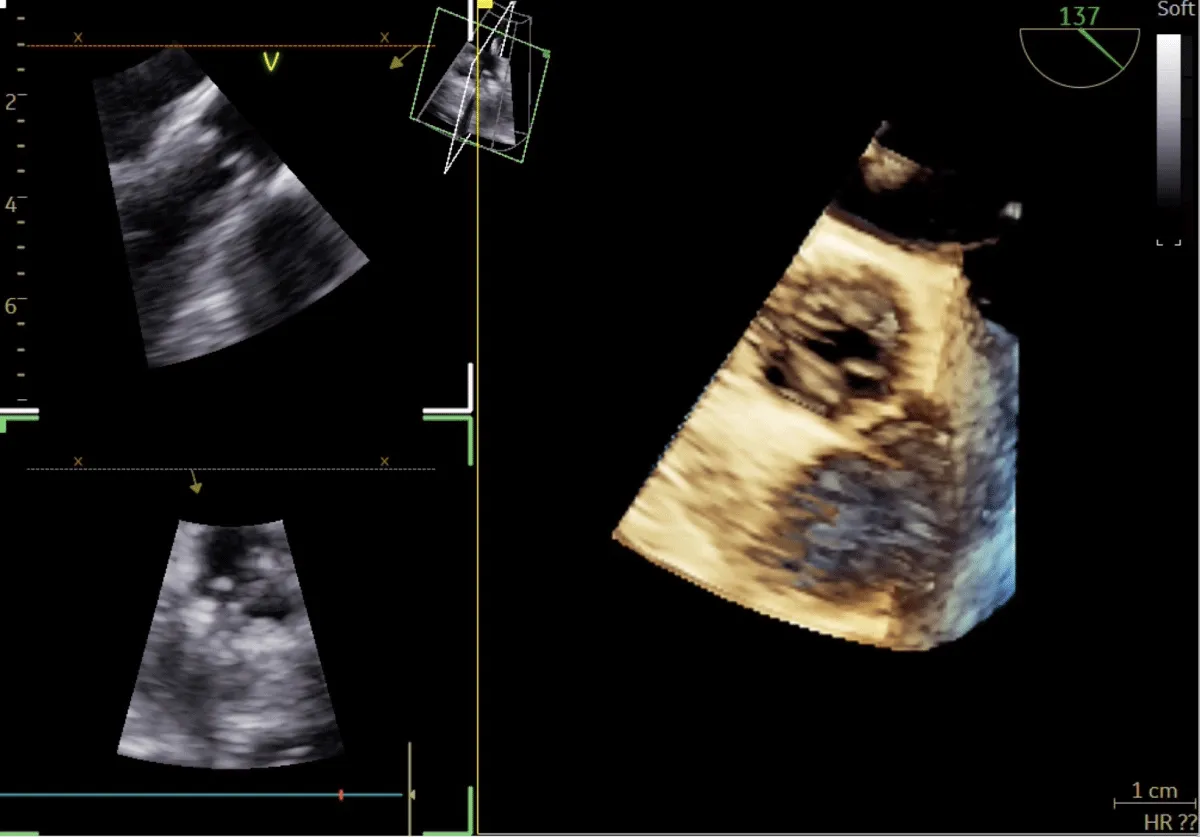
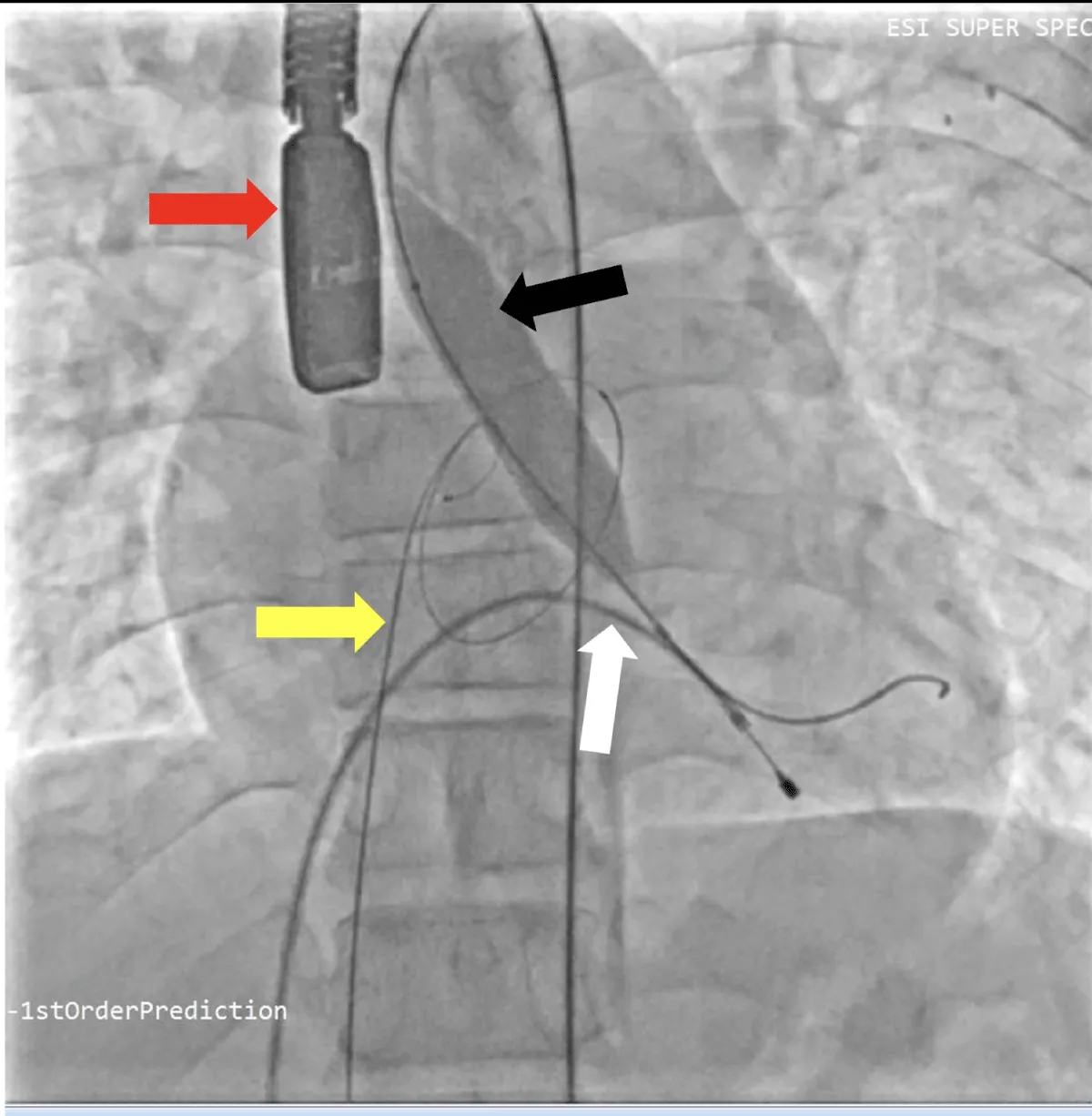
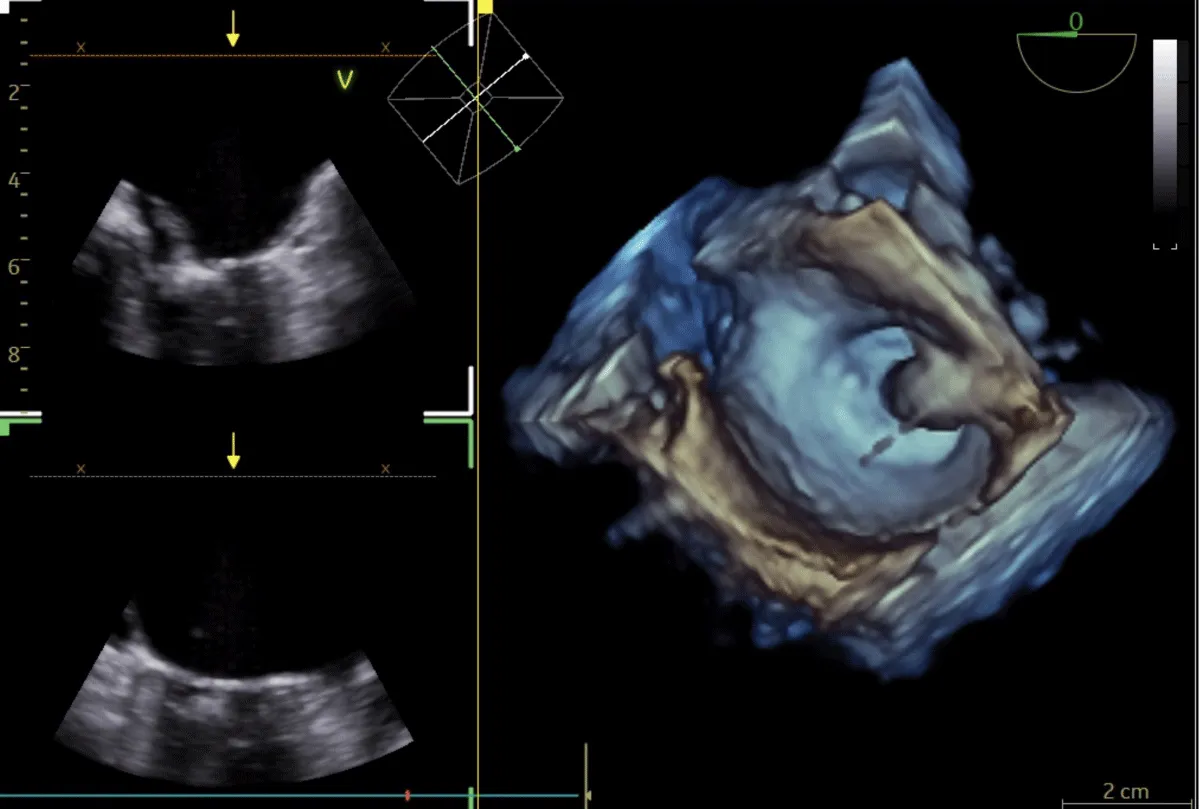
After obtaining consent, access was obtained through the right femoral vein and artery. Under 4D Transesophageal Echocardiography (4D TEE) guidance, the first transseptal puncture was performed with a broken Brough needle, and the LA wire was inserted through femoral venous access (Figure 1). Right femoral artery access was used for retrograde crossing of the aortic valve (AV) (Figure 2), and a Teflon wire was placed in the left ventricle. The aortic valve (AV) was dilated with a 14 mm ATLAS GOLD (BARD) balloon (Figure 3, Video 1).
Figure 1: A,B: 4Dimensional multiplanar transoesophageal echocardiography. A. 4D image with Left atrial wire, B. Severe mitral stenosis with mitral area of 0.5 cm2, 1C &1D. Showing multiplane of mitral valve.
Figure 2: 4Dimensional multiplanar transoesophageal echocardiography view of aortic valve.
Figure 3: Fluoroscopic image of aortic valve. Balloon dilatation of aortic valve under fluoroscopy and transoesophageal echocardiography (Red arrow), yellow arrow – Left atrial wire, white arrow- Right ventricular pacing lead, black arrow- Balloon across the aortic valve.
Following a single dilatation, the AV gradient decreased from 82 mm Hg to 30 mm Hg without aortic regurgitation (AR). Subsequently, the mitral valve (MV) was dilated with a 26 mm Inoue balloon (Figures 4,5) (Video 2). After a single dilatation, the MV gradient was reduced from 35/21 mm Hg to 12/5 mm Hg, and the MV area increased from 0.5 cm2 to 1.6 cm2 (Figure 6)
Figure 4: Fluoroscopic image of mitral valve. Balloon dilatation of mitral valve under fluoroscopy and transoesophageal echocardiography (white arrow), black arrow- Balloon across the mitral valve.
Figure 5: 4Dimensional multiplanar transoesophageal echocardiography – Balloon dilatation of the mitral valve with Inoue balloon.
Figure 6: 4Dimensional multiplanar transoesophageal echocardiography – mitral valve after balloon dilatation.
Follow up
During the 1-month, 3-month, and 6-month follow-ups, the patient remained free from symptoms. He was able to resume his construction work without experiencing significant symptoms, comparable to his pre-symptomatic state. Additionally, his valve function was preserved, and he maintained a sinus rhythm. 2D-ECHO examinations revealed mild MS and mild AS without MR or AR, along with normal biventricular function.
Clinical presentation
A 55-year-old gentleman presented to our center with complaints of exertional dyspnea progressing from NYHA class I to NYHA class III over a 3-year period, along with easy fatiguability, dizziness, and poor exercise capacity.
Past history
He had no known history of hypertension, diabetes, or alcohol use. However, his viral markers were positive for human immunodeficiency virus (HIV) and hepatitis B antigen (HBsAg). He had been on anti-retroviral therapy for 3 years.
Investigations
His hemogram, LFT, RFT, and lipid profile were normal. ECG revealed atrial fibrillation with a controlled heart rate, LA enlargement, and LVH with a strain pattern. Chest X-ray showed mild cardiomegaly, LA enlargement, and mild PVH. 2D ECHO revealed RHD, severe calcific MS, and severe calcific AS with fair left ventricular function.
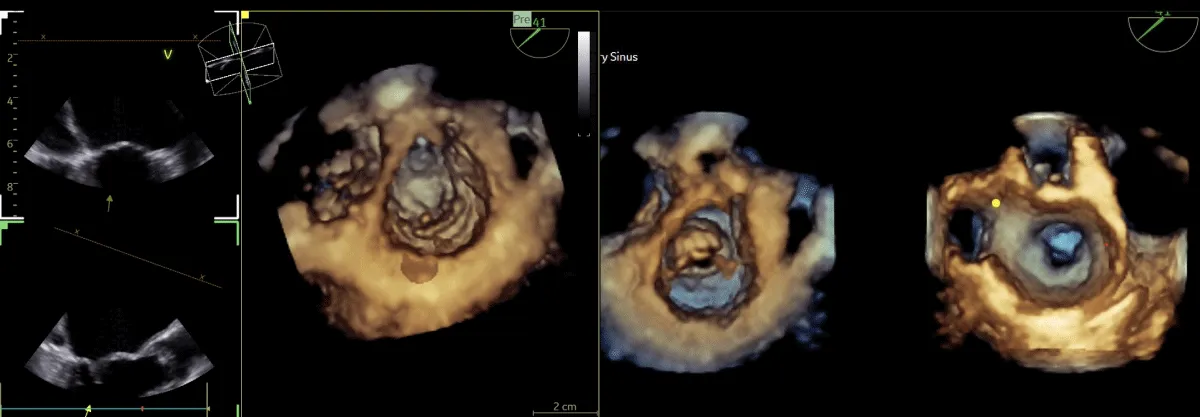
Management
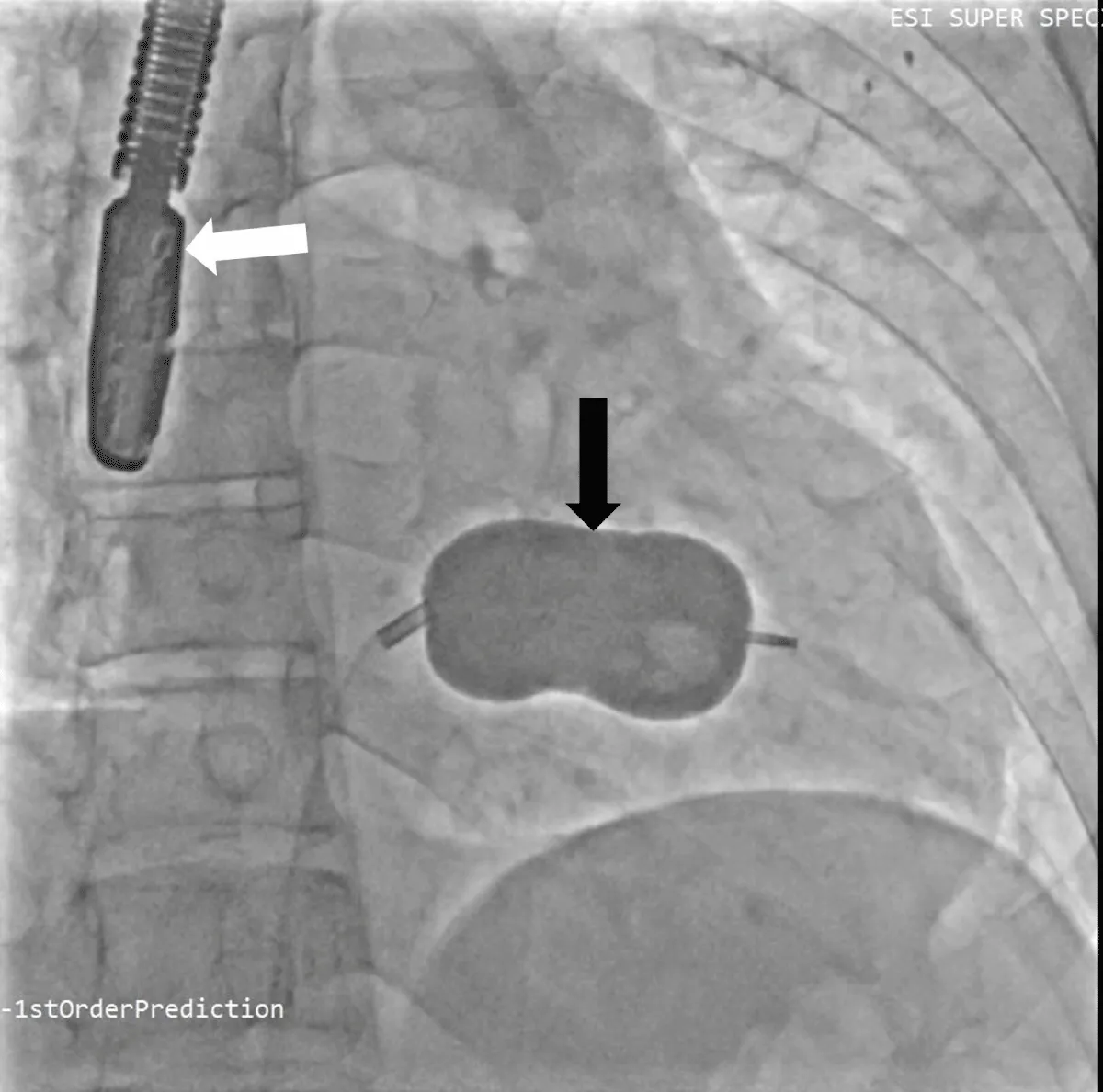
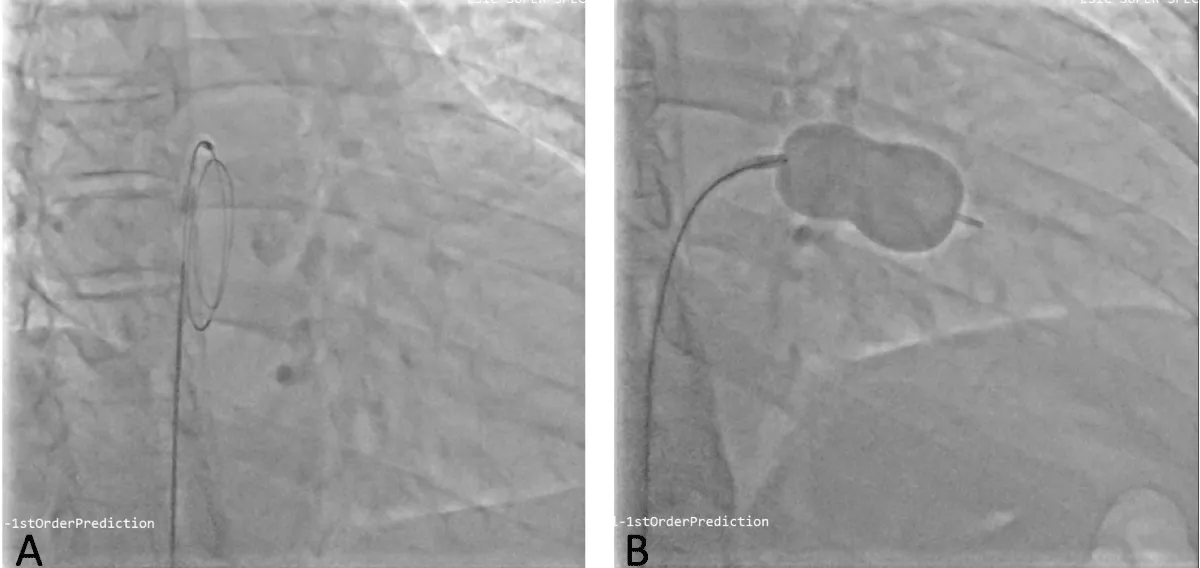
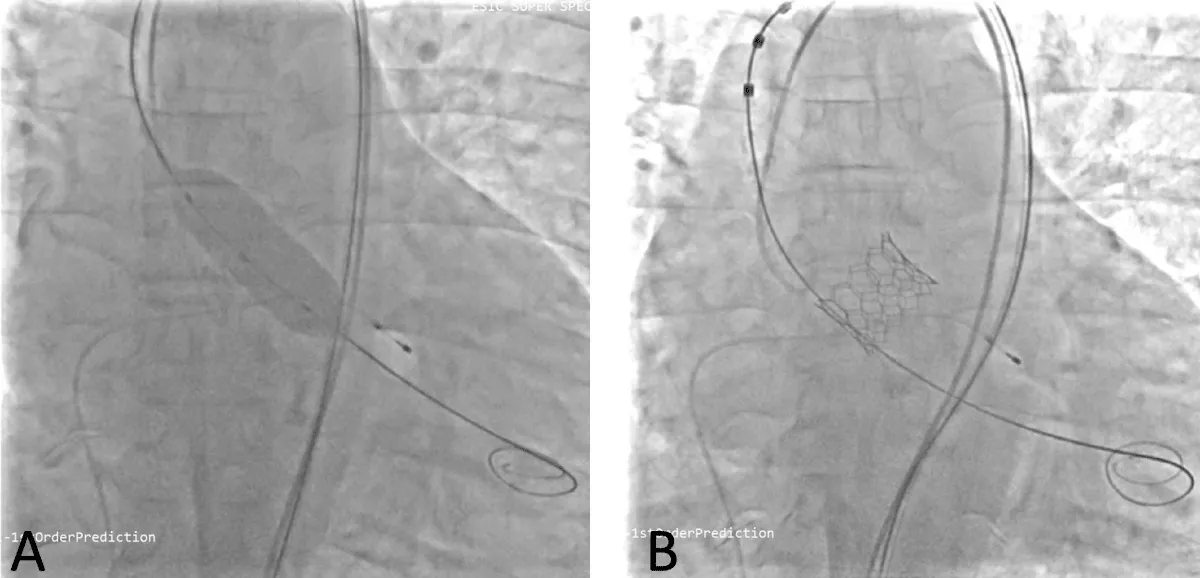
He was planned for double valve replacement (DVR), but the patient declined due to the high surgical risk. Therefore, he was considered for staged BMV and Transcatheter aortic valve replacement (TAVR). Pre-procedural planning was done for TAVR, and after ensuring the patency and adequacy of femoral vessels, he underwent a coronary angiogram (CAG), which showed normal coronaries. Following consent, the right femoral vein was accessed. A transseptal puncture was performed with a broken Brough needle, and the LA wire was parked. The MV was dilated with a 26 mm Inoue balloon (Figure 7), resulting in a reduction of the MV gradient from 24/10 mm Hg to 9/5 mm Hg and an increase in MV area from 0.9 cm2 to 1.6 cm2. There were no post-procedural complications. After 1 month, he underwent TAVI. Both right and left femoral artery access was obtained. Following pre-dilatation of the AV with an 18 mm balloon, TAVR was performed using a 26 mm balloon-expandable valve (Myval, Meril Lifesciences, Vapi, Gujarat, India) (Figure 8) (Video 3), followed by post-dilatation under accelerated right ventricular pacing (180 bpm). ECHO and final aortography showed no paravalvular leakage after device release (Figure 9).
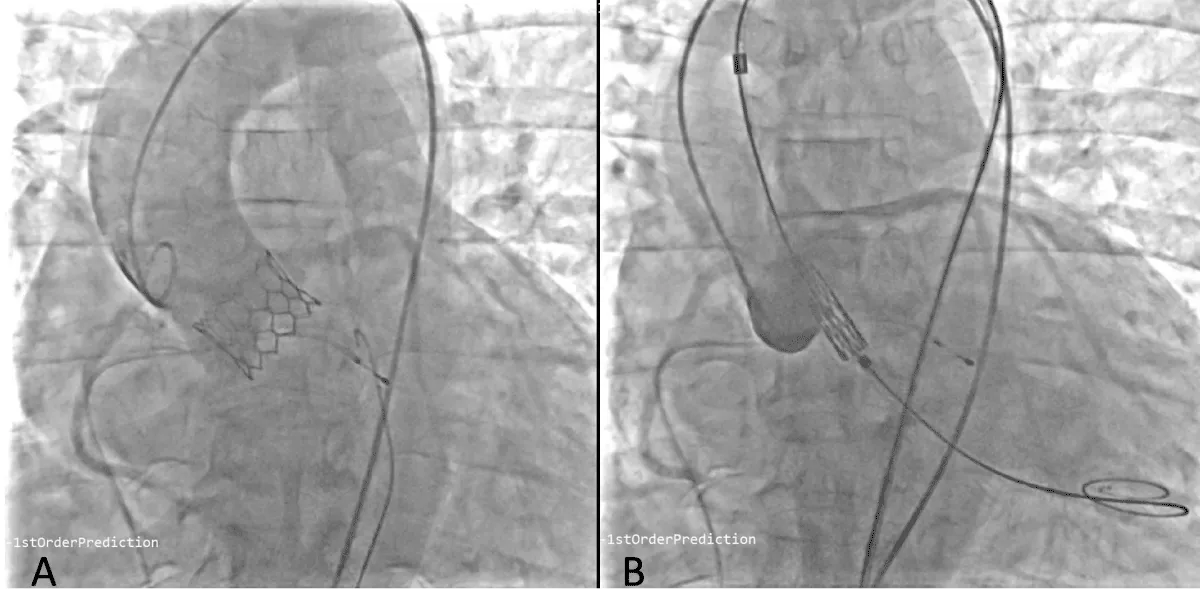
Figure 7: Fluoroscopic image of LA wire passed through atrial septal puncture (A) and Balloon dilatation of the mitral valve with Inoue balloon (B).
Figure 8: Fluoroscopic image of Balloon dilatation of the aortic valve (A) followed by aortic valve implantation (B) under right ventricular pacing.
Figure 9: Fluoroscopic image of aortic valve implantation without coronary compression after (A) and before the deployment (B).
Post-TAVR, the AV gradient was reduced from 98 →10 mm Hg. No procedural or post-procedural complications occurred. The hospital course was uncomplicated, and the patient was discharged after 4 days.
Follow up
At the 1-month follow-up, the patient was classified as NYHA class I. He successfully resumed his routine activities, and 2D ECHO indicated mild MS without MR or AR, along with near-normal left ventricular function.Rheumatic heart disease (RHD) often necessitates double valve replacement (DVR) for combined multivalvular lesions, which carries a higher operative mortality rate compared to isolated aortic valve replacement (AVR) [1]. In response, percutaneous options have emerged as an alternative for high-risk patients with concomitant severe aortic stenosis (AS) and mitral stenosis (MS). Percutaneous transvenous mitral commissurotomy (PTMC) is the preferred treatment for severe MS with pliable valves, typically indicated by a Wilkins score < 8, assessed via 2D echocardiography [2] based on the valve and sub valvular apparatus morphology.
Non-surgical options for AS encompass balloon aortic valvotomy (BAV) and Transcatheter aortic valve replacement (TAVR), with the choice guided by various factors such as age, valve anatomy, comorbidities, surgical risk, patient preference, and centre experience.
The combination of PTMC with BAV has been utilized in the past, though initially viewed as palliative due to restenosis concerns. Before 2000, these combination techniques were predominant, particularly in palliative cases involving high-risk or surgically unsuitable patients. However, with the decreasing incidence of RHD, these methods became less common.
In our first index case, the patient was a young manual labourer from a poor socioeconomic background and limited access to medical care. Given these factors, we offered the combination technique to postpone surgery and avoid long-term anticoagulation, considering the occupational risk and poor medical access. To our knowledge, our case represents the first instance where PTMC with BAV was performed under 4D TEE guidance, facilitating transseptal puncture and balloon negotiation across the mitral valve.
In the second case, the patient was unwilling for surgery. We performed staged TAVR following balloon mitral valvotomy to ensure successful PTMC prior to TAVR in view of the heavily calcified valve seeming unsuitable for intervention.
Supplementary Table 1 summarizes existing literature on non-surgical techniques for multivalvular disease management, showcasing various treatment modalities and outcomes.
| Supplementary Table 1: The summary of the published cases of non-surgical techniques for multivalvular disease. | |||||
| Author, Year | Age (years) & Sex | Cases | Presentation | Treatment modality | Outcome |
| Amir Aziz Alkatiri, et al. 2022 [3] | 85-year-old woman | 1 | Effort-related dyspnea NYHA II with multiple co-morbidities | Staged TAVR + PTMC | Preserved valve function at 3 years |
| Bilge M, et al. 2015 [4] | 52-year-old woman with urethral carcinoma | 1 | Effort-related dyspnea NYHA II | TAVR + PTMC simultaneously | Preserved valve function |
| Mechmeche R, et al. [5] | 33-year woman | 1 | - | PTMC +BAV | Improved valve function |
| Satyavan Sharma, et al. 1997 [6] | 9-52 years | 10 | NYHA I-IV | PTMC+BAV | Improved clinical features at 2.5years |
| OR Rosales, et al. 1993 [7] | Elderly | 27 | NYHA class II to IV | PTMC +BAV | Preserved valve function |
| C E Ruiz, et al. 1992 [8] | 43-year-old woman | 1 | Recurrent ASD, severe MS, AS, and TR | PTMC+BAV+ ASD device closure | Clinical improvement & expired after 8 weeks |
| George S Konugres, et al. 1990 [9] | 35 year old woman | 1 | NHYA III | PTMC+BAV+ Tricuspid valvotomy | Clinical improvement |
| Aaron D Berman, et al, 1988 [10] | 60yrs- 83yrs | 6 | NYHA class II to IV | PTMC +BAV | Preserved valve function at 1-8 months |
| Gordon L Kritzer et al. 1987 [11] | 87 year old woman | 1 | Acute pulmonary edema | PTMC +BAV | Improved heart failure |
| NYHA: New York Heart Association; MS: Mitral Stenosis; AS: Aortic Stenosis; ASD: Atrial Septal Defect; TR: Tricuspid Regurgitation; PTMC: Percutaneous Transvenous Mitral Commissurotomy; BAV: Balloon Aortic Valvotomy; TAVR: Transcatheter Aortic Valve Replacement; BMV: Balloon Mitral Valvotomy | |||||
Considering the middle age and tight calcific AS, a balloon-expandable intra-annular device was inserted so that a self-expanding supra-valvular device could be considered in case of restenosis. Regarding TAVR, while its utilization is increasing globally due to technological advancements, its use in countries like India is hindered by cost, lack of hardware, indigenous valves, structured training, and poor anatomical substrates [12]. The findings from the MyVal-1 study have demonstrated notable enhancements in aortic valve gradients, functional status, and the six-minute walk test [13]. As a result, this valve has emerged as an appealing option, particularly among interventional cardiologists in developing nations. Its lower cost compared to Western valves makes this therapy accessible to a broader patient population, thereby addressing a crucial need in regions where resources are limited. This increased accessibility has the potential to significantly impact patient care by providing effective treatment options to a larger number of individuals who may otherwise face barriers to accessing advanced medical interventions. Additionally, the positive outcomes observed in studies like MyVal-1 underscore the importance of continued research and development efforts to improve the availability and affordability of essential medical technologies in resource-constrained settings.
Limitations and future directives
These two case reports offer valuable insights; however, it’s important to recognize that their findings may not be applicable to all situations. Generalizing results from such limited data can be misleading. Therefore, future research endeavours should focus on conducting prospective studies. These studies would provide more comprehensive and reliable evidence, especially for financially constrained and high-risk patients. By undertaking prospective studies, we can better understand the efficacy and implications of these interventions in diverse patient populations, thus informing clinical practice and healthcare decision-making more effectively.
Multivalvular heart disease remains a significant concern in developing countries, where treatment guidelines are often limited. In conclusion, proper case selection, comprehensive pre-operative evaluation, and appropriate use of multimodality imaging are crucial for successful outcomes, particularly in complex cases of multivalvular heart disease. Percutaneous techniques, including combined PTMC with BAV, can offer benefits to young patients with favorable anatomy who struggle with adherence to anticoagulation, and staged PTMC with TAVR, offers viable options for high-risk patients deemed unwilling or unsuitable for traditional surgical approaches.
Ethical considerations
We have obtained permission from the patients to publish their medical information and images in a medical journal, respecting their autonomy and individual rights.
- The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2022 Update on Outcomes and Research. Kim, Karen M. et al. The Annals of Thoracic Surgery, 2022; 115(3):566 – 574
- Wilkins GT, Weyman AE, Abascal VM, Block PC, Palacios IF. Percutaneous balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J. 1988 Oct;60(4):299-308. doi: 10.1136/hrt.60.4.299. PMID: 3190958; PMCID: PMC1216577.
- Alkatiri AA, Yamanaka F, Shishido K, Moriyama N, Ochiai T, Noguchi K, Firman D, Soerianata S, Saito S. Percutaneous transvenous mitral commissurotomy and transcatheter aortic valve replacement for rheumatic mitral and aortic stenosis. J Cardiol Cases. 2022 Aug 18;26(5):357-359. doi: 10.1016/j.jccase.2022.07.010. PMID: 36312777; PMCID: PMC9605916.
- Bilge M, Alsancak Y, Ali S, Yasar AS. Concurrent Transcatheter Aortic Valve Implantation and Percutaneous Transvenous Mitral Commissurotomy for Totally Percutaneous Treatment of Combined Severe Rheumatic Aortic and Mitral Stenosis. J Heart Valve Dis. 2015 May;24(3):286-9. PMID: 26901896.
- Mechmeche R, Cherif A, Elmnouchi R. Dilatation percutanee d'un double retrecissement mitral et aortique d'origine rhumatismale [Percutaneous balloon valvotomy for combined rheumatic mitral and aortic stenosis]. Tunis Med. 2008 Jun;86(6):598-9. French. PMID: 19216456.
- Satyavan S, Yunus SL, Dhruman MD, Robin Joseph P. Percutaneous double-valve balloon valvotomy for multivalve stenosis: Immediate results and intermediate-term follow-up. American Heart Journal. 1997; 133(1):64-70.
- Rosales OR, Hess MJ, Heibig J, Smalling RW. Percutaneous transluminal balloon aortic and mitral valvuloplasty in 27 patients treated at Hermann Hospital. Tex Med. 1993 Aug;89(8):60-8. PMID: 8372383.
- Ruiz CE, Gamra H, Mahrer P, Allen JW, O'Laughlin MP, Lau FY. Percutaneous closure of a secundum atrial septal defect and double balloon valvotomies of a severe mitral and aortic valve stenosis in a patient with Lutembacher's syndrome and severe pulmonary hypertension. Cathet Cardiovasc Diagn. 1992 Apr;25(4):309-12. doi: 10.1002/ccd.1810250411. PMID: 1373992.
- Konugres GS, Lau FY, Ruiz CE. Successive percutaneous double-balloon mitral, aortic, and tricuspid valvotomy in rheumatic trivalvular stenoses. Am Heart J. 1990 Mar;119(3 Pt 1):663-6. doi: 10.1016/s0002-8703(05)80290-x. Erratum in: Am Heart J 1990 Dec;120(6 Pt 1):1486. PMID: 1689932.
- Berman AD, Weinstein JS, Safian RD, Diver DJ, Grossman W, McKay RG. Combined aortic and mitral balloon valvuloplasty in patients with critical aortic and mitral valve stenosis: results in six cases. J Am Coll Cardiol. 1988 Jun;11(6):1213-8. doi: 10.1016/0735-1097(88)90284-7. PMID: 3366995.
- Kritzer GL, Block PC, Palacios I. Simultaneous percutaneous mitral and aortic balloon valvotomies in an elderly patient. Am Heart J. 1987 Aug;114(2):420-3. doi: 10.1016/0002-8703(87)90512-6. PMID: 2955690.
- Gupta P, Arora S, Qamar A, Gupta M, Seth A. Current status of transcatheter aortic valve replacement in India. Cardiovasc Diagn Ther. 2020 Feb;10(1):83-88. doi: 10.21037/cdt.2019.05.04. PMID: 32175230; PMCID: PMC7044098.
- Seth A. MyVal-1 Study: One-year clinical outcomes of India’s first indigenously designed and manufactured TAVR system. Presented as a Late Breaking Trial at the EuroPCR 2019; May 22nd, 2019; Paris, France.