More Information
Submitted: June 18, 2024 | Approved: June 27, 2024 | Published: June 28, 2024
How to cite this article: Akmal S, Ikramullah I, Asif AS. Descriptive Study of the Urinary Tract Infections in Patients Admitted in the Cardiology Ward of Afghan Momand Medical Complex. J Cardiol Cardiovasc Med. 2024; 9: 098-101.
DOI: 10.29328/journal.jccm.1001186
Copyright License: © 2024 Akmal S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: UTI; Risk factors; Clinical profile
Descriptive Study of the Urinary Tract Infections in Patients Admitted in the Cardiology Ward of Afghan Momand Medical Complex
Shams Akmal1, Ibrahimi Ikramullah2* and Agha Said Asif3
1Head of Cardiology Department, Afghan Momand Medical Complex, Nangarhar, Afghanistan
2Lecturer, Department of Internal Medicine, Medical Faculty, Nangarhar University, Afghanistan
3Trainee, Department of Internal Medicine, Medical Faculty, Nangarhar University, Afghanistan
*Address for Correspondence: Ibrahimi Ikramullah, Lecturer, Department of Internal Medicine, Medical Faculty, Nangarhar University, Afghanistan, Email: [email protected]
Urinary Tract Infection (UTI) is very common in our community most specifically in married females with numerous antecedent risk factors. The aim of the study was to find out about the current risk factors and clinical profile of urinary tract infections in patients admitted to the cardiology ward of Afghan Momand Medical Complex for various purposes.
It was a cross-sectional descriptive hospital-based study including both male and female patients visiting the Afghan Momand Medical Complex from January 2022 to June 2022.
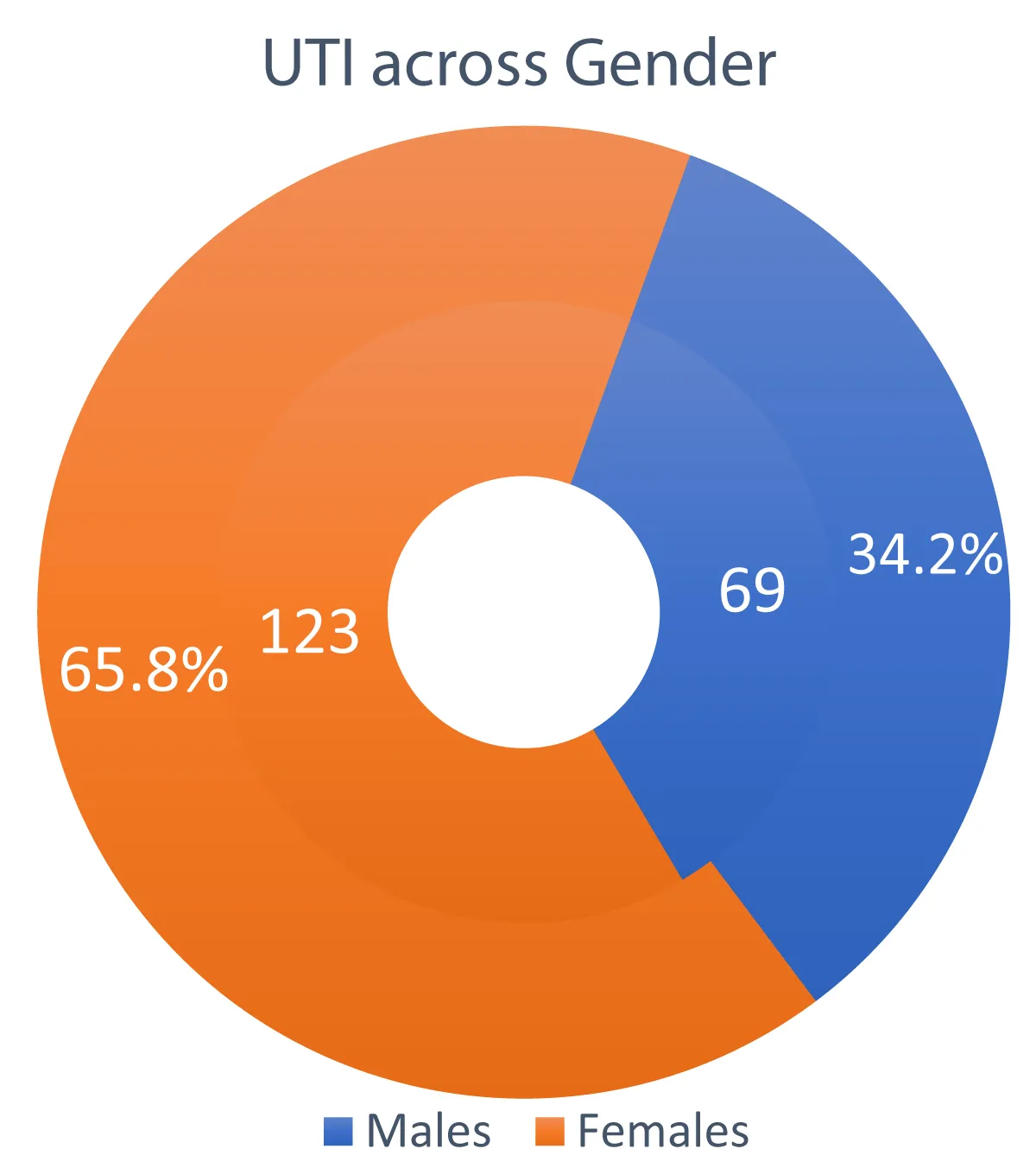
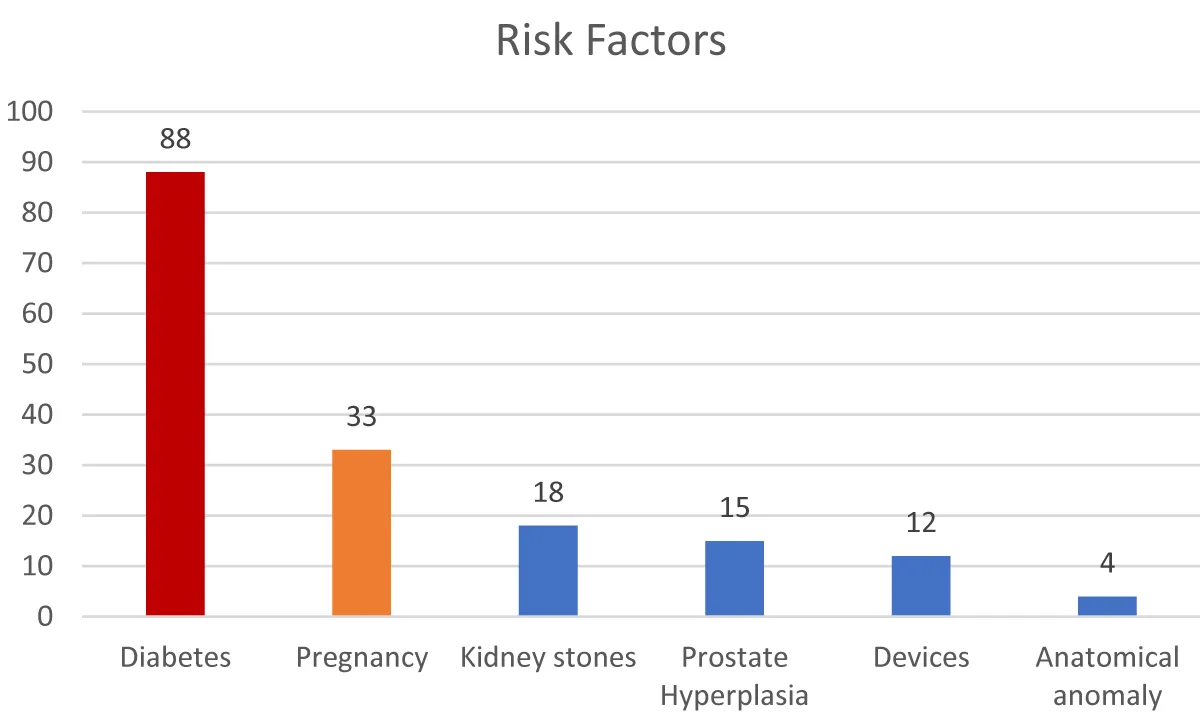
Of all 960 patients, 202 (21%) patients had urinary tract infections with gender distribution as 69 (34.2%) males and 133 (65.8%) females. In fact, 33 (16.3%) patients with urinary tract infections were single while the rest 169 (83.7%) patients were married. In addition, regarding clinical profile, the following clinic was respectively more prevalent: Dysuria in 120 (59.4%) patients, flank pain in 73 (36.1%) patients, urine frequency in 67 (33.1%) patients, urgency in 36 (17.8%) patients, fever in 24 (11.8%) patients, and nausea and vomiting in 19 (9.4%) patients. Moreover, the following risk factors were respectively the most common ones: Diabetes mellitus 86 (42.5%), pregnancy 30 (14.9%), stones 15 (7.4%), 10 (4.9%) devices, 10 (4.9%) prostatic hyperplasia, and 4 (2%) anatomical anomalies.
Urinary tract infection is a common disease in the admitted patients in Afghan Momand Medical Complex specifically being more common in females and early 20s of the age. In fact, diabetes, pregnancy, and kidney stones were the leading associated factors with UTI. Moreover, dysuria, bladder emptying irritative symptoms, and abdominal pain were the most prevalent clinical profile of the patients. Special attention should be paid to infectious diseases in cardiac patients since infection itself is a stress and a threat to such patients and authorities should design special measures to prevent UTI in the general population to avoid a sum of burden on the health system.
Infectious diseases are the leading burden on the health system in Afghanistan causing many adverse events [1]. In fact, urinary tract infection constitutes a major portion of the infection era in Afghanistan specifically in Nangarhar; in addition, it is supposed to be the major precipitating factor in diabetic patients resulting in diabetic ketoacidosis [2]. Females in comparison to males are more prone to developing urinary tract infections of their short urethra, poor hygiene, antispermicidal usage, and reduced post-coital voiding volume [3], in addition, patients with advanced age are considered more likely to develop urinary tract infection but it is uncommon in males except for the diurnal age of less than 1 year and greater than 60 years [4]. In fact, the frequency of sexual intercourse in the literature has been shown to directly increase the incidences of urinary tract infection as weekly sexual intercourse has been supposed to increase the incidences of urinary tract infection by 1.4 fold while sexual intercourse of five times a week has been related with a 4.8 fold increase in the incidences of urinary tract infection [3,5]. In post-menopause, anatomical defects affecting bladder voiding such as cystocele, urinary incontinence, residual urine, and premenopausal history of urinary tract infection are coined as well-known risk factors in the literature [6]. Diabetic patients else known as a vulnerable population are prone to the development of urinary tract infections for some reasons such as incomplete voiding, urinary flow obstruction, acontractile or neurogenic bladder, and impaired cytokine secretion in female diabetic patients, moreover, urinary tract infection in such population is considered as complicated UTI, in other words, it is a means of treatment failure [7].
Despite much research on the topic, we still lack analyzed data about urinary tract infections in our local hospital so we aimed to conduct this study to find out the exact data about the incidences, clinical profile of the patients, and pertaining risk factors of the disease in our population which can be used in various modalities.
It was a retrospective cross-sectional hospital-based study conducted from January 2022 up to June 2022 at the Afghan Momand Medical Complex.
The study included all patients admitted in the cardiology ward of Afghan Momand Medical Complex in the aforementioned period that were further categorized as either having urinary tract infections or not where we finally received medical files of 202 confirmed patients with UTI.
The study was based on purposive sampling including both male and female patients with the age greater than 18 years being admitted to the center in the aforementioned period. Patients with missing or incomplete files and diseases other than UTI were excluded from the study.
Urinary tract infection was categorized as either upper UTI or lower UTI based on the presence of systemic clinic as fever and leukocytosis [8].
Ethical approval was taken from the hospital’s ethical board being registered at IRB 317.
Data was analyzed in SPSS version 26 using mean ± standard deviation for continuous variables and frequencies and percentages for categorical variables.
Out of 960 patients admitted to the internal medicine ward of Afghan Momand Medical Complex, 202 patients (21%) were diagnosed with urinary tract infection, their mean age at admission was 44.8 ± 18.2 and their mean body temperature was 37.5±0.8 centigrade.
Urinary tract infection was more prevalent in females compared to male patients in the study and its distribution across genders is shown in Figure 1.
Figure 1 shows urinary tract infection distribution across genders as being more in females compared to males; 123 (65.8%) patients diagnosed with UTI were females while only 69 (34.2%) patients diagnosed with UTI were males.
Figure 1: UTI Distribution across Gender.
Most cases of UTI were in the lowest age group of our study population, 18-30 years of age (44.1%) followed respectively by 31 years - 43 years of age (28.7%), 44-56 years of age (16.8%), and age group greater than 56 years (10.4%) as shown in Table 1.
| Table 1: UTI Distribution across Age Groups. | |
| Age Group (years) |
Frequency |
| 18-30 | 89 (44.1%) |
| 31-43 | 58 (28.7%) |
| 44-56 | 34 (16.8%) |
| > 56 | 21 (10.4%) |
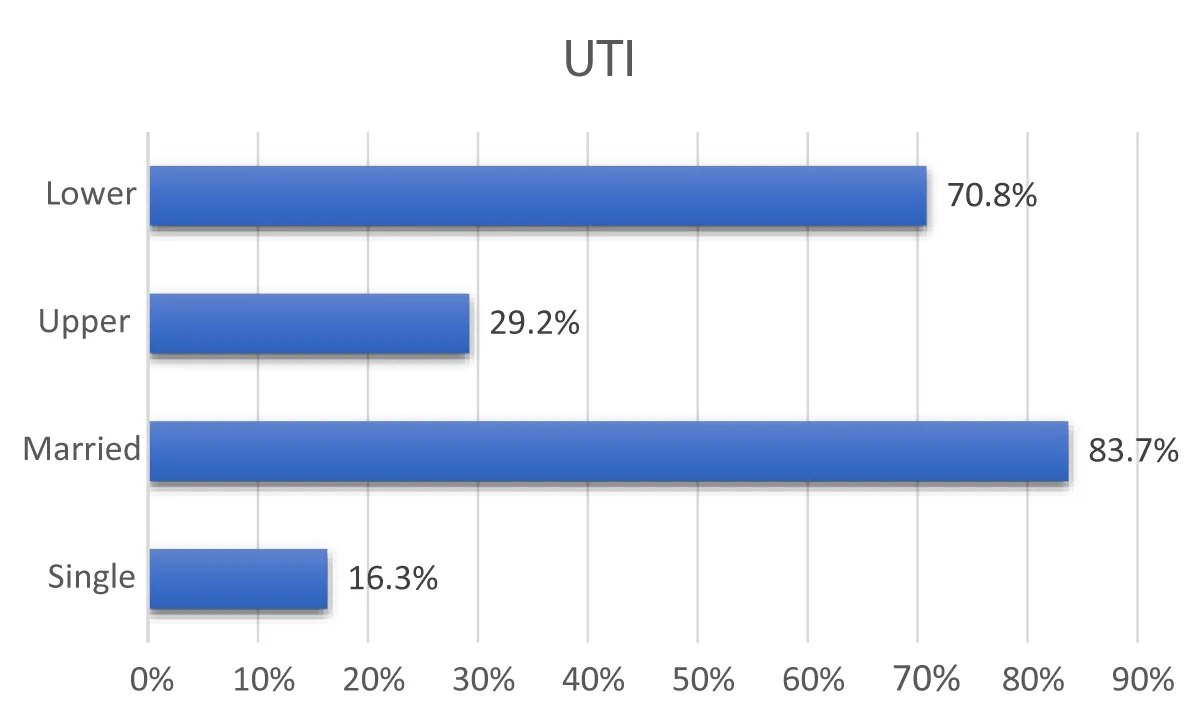
Urinary tract infection was obviously more common in couples compared to single patients. In addition, regarding the type of urinary tract infection, we found lower UTIs more prevalent in our study population compared to upper UTIs which were classified regarding systemic clinic as leukocytosis and fever. Cystitis was more common in lower urinary tract infections while acute pyelonephritis constituted a major class in patients with upper UTI. The aforementioned findings are shown in Figure 2 for better visualization and understanding.
Figure 2 shows that 143 (70.8%) patients out of 202 patients were diagnosed with lower UTI while 59 (29.2%) patients were diagnosed with upper UTI. Furthermore, married couples were identified as comparatively more prevalent subjects with the diagnosis of UTI compared to single patients: 169 (83.7%) vs. 33 (16.3%).
Figure 2: UTI types and their distribution across marital status.
It is well-known that clinical profile depends mainly on the type of UTI but a few symptoms and signs are common in both types such as those of the bladder emptying irritative symptoms. In fact, dysuria was the most common symptom in our study followed by others as shown in Table 2.
| Table 2: Clinical profile of patients with UTI. | |
| Clinical Profile | Frequency |
| Dysuria | 130 (59.4%) |
| Flank pain | 73 (36.1%) |
| Frequency | 67 (33.1%) |
| Urgency | 36 (17.8%) |
| Fever | 24 (11.8%) |
| Nausea/vomiting | 19 (9.4%) |
Diabetes mellitus was found the most accompanying disease in patients with urinary tract infection in our study which is shown in Figure 3 along with other accompanying conditions.
Figure 3 shows the frequency of risk factors or associated conditions in chronological order in patients with urinary tract infections. Diabetes was shown the most common one followed by pregnancy, kidney stones, etc. respectively.
Figure 3: Risk factors.
The major findings of the study show that UTI was a common disease in patients being admitted to the cardiology ward of Afghan Momand Medical Complex (21%) which is comparable to the findings of studies in the literature; in fact, a study in Uganda by Odoki, et al. demonstrated 36% prevalence of UTI in a single center hospital-based study in 2019 [9]. In fact, the reasons for the comparatively lower prevalence in our study may be self-administration of antibiotics, having a single-sex partner lifelong, and lack of the use of indwelling catheters and intrauterine contraceptive devices. The wondering point in our study was the presence of relatively young patients in the cardiology ward presumably due to lack of screening for cardiac problems in early childhood, high prevalence of rheumatic heart disease which most predominantly occurs earlier than 20, presence of depression and anxiety, use of illicit drugs, and presence of congenital heart disease with an overt clinic in the second decade of life.
UTI in our study was more common in females and the lowest age group, 18-30 which is, in fact, comparable with the findings of a study by Magliano, et al. in 2012 [10]. In fact, studies have shown that females are more prone to developing UTI for their short urethra since the most common transmission is known as ascending transmission, reduced post-coital voiding volume, and the use of spermicidal agents [3].
The clinical profile more prevalent in our study was comparable to the findings of a study by Odoki, et al. in 2019 in Uganda and Bay, et al. in 2006 in the Philippines. In fact, they also found dysuria, abdominal pain, and fever as the most prevalent clinic in their patients [9,11].
The most common associated factors with urinary tract infection in our study were diabetes, pregnancy, kidney stones, indwelling catheters, intrauterine contraceptive devices, etc. However, kidney stones in our study were underestimated because such patients are referred to the urology ward and/or they primarily visit the urology ward. Diabetes Mellitus in literature is shown to reduce bladder emptying and cause urinary flow obstruction or retention due to neurogenic bladder, an autonomic neuropathy resulting from diabetes mellitus [7]. In fact, the aforementioned findings are consistent with the findings of the studies by Odoki, et al. in Uganda in 2019, Magliano, et al., in 2012, and Bay, et al. in the Philippines in 2006 [9-11].
Regarding the connection between cardiovascular disease and urinary tract symptoms, a systematic review of 15 studies revealed a higher incidence of major cardiovascular events in patients with moderate to severe lower urinary tract symptoms compared to patients with no urinary tract symptoms [12]. Furthermore, in a population-based cohort study including 4144 participants, it was demonstrated that severe lower urinary tract symptoms were significantly associated with an increased risk of early diabetes mellitus and heart disease; in other words, it could be said that UTI and cardiovascular disease share some risk factors including hypertension, diabetes, etc [13-15]. In addition, the literature demonstrates peak incidences of UTI and heart disease in the winter season and it might be concluded that both diseases simultaneously exist [16,17]. Furthermore, dapagliflozin used in the treatment of heart failure is associated with an increased risk of urinary tract infections [18]. There are various reasons that could explain the connection between cardiovascular disease (CVD) and lower urinary tract symptoms (LUTS): these include metabolic syndrome, persistent inflammation, pelvic ischemia due to atherosclerosis, heightened activation of Rho-kinase, dysfunction in the nitric-oxide synthase pathway in endothelial cells, autonomic overactivity with sympathetic irregularities, and declining testosterone levels [19,20].
Our study had a few limitations such as the study design being a descriptive cross-sectional, loss to follow up, and a few missing variables in most files e.g. urine culture and sensitivity. However, the authors have made their utmost effort in collecting clean data and its analysis.
Urinary tract infection is a common disease in the admitted patients in Afghan Momand Medical Complex specifically being more common in females and early 20s of the age. In fact, diabetes, pregnancy, and kidney stones were the leading associated factors with UTI. Moreover, dysuria, bladder emptying irritative symptoms, and abdominal pain were the most prevalent clinical profile of the patients. Special attention should be paid to infectious diseases in cardiac patients since infection itself is a stress and a threat to such patients and authorities should design special measures to prevent UTI in the general population to avoid a sum of burden on the health system.
The authors express their warm gratitude to all those who facilitated data collection.
- Measure DHS. Afghanistan Mortality Survey 2010: Afghan Public Health Institute. Ministry of Public Health, Central Statistics Organization, Kabul, Afghanistan, ICF Macro, Calverton, Maryland, USA, IIHMR, Jaipur, India and WHO/EMRO, Cairo, Egypt. 2011.
- Ibrahimi II, Ahmadzai H, Shams SJ. Precipitating Factors and Clinical Presentation at the Time of Admission for Diabetic Ketoacidosis in Nangarhar Afghanistan. Interdisciplinary Approaches to Medicine. 2023; 4(2).
- Khatri B, Basnyat S, Karki A, Poudel A, Shrestha B. Etiology and antimicrobial susceptibility pattern of bacterial pathogens from urinary tract infection. Nepal Med Coll J. 2012 Jun;14(2):129-32. PMID: 23671963.
- Budaya TN, Ardiani A, Ardiani A. Prevalence of urinary tract infection and correlation with lifestyle in women at Hadakewa Health Center, Lembata, East Nusa Tenggara. Drug Invention Today. 2019;12(11).
- Lawrence M. Tierney Jr, Stefan Ime Phee Maxine A Papadakis. (2020) Current Medical diagnosis (59th ed). Mc-Graw Hill. USA. Pp 210.
- Haider, G., Zehra, N., Munir, A. A., & Haider, A. (2010). Risk factors of urinary tract infection in pregnancy. JPMA. The Journal of the Pakistan Medical Association, 60(3), 213.
- Prajapati P, Aundhakar S, Patil V. Hospital-acquired urinary tract infections in indoor patients with indwelling Foley's catheter: A prospective study in a tertiary care teaching hospital. Int J Pharm Res. 2020;12(3).
- Johansen TE, Botto H, Cek M, Grabe M, Tenke P, Wagenlehner FM, Naber KG. Critical review of current definitions of urinary tract infections and proposal of an EAU/ESIU classification system. Int J Antimicrob Agents. 2011 Dec;38 Suppl:64-70. doi: 10.1016/j.ijantimicag.2011.09.009. Epub 2011 Oct 21. PMID: 22018988.
- Odoki M, Almustapha Aliero A, Tibyangye J, Nyabayo Maniga J, Wampande E, Drago Kato C, Agwu E, Bazira J. Prevalence of Bacterial Urinary Tract Infections and Associated Factors among Patients Attending Hospitals in Bushenyi District, Uganda. Int J Microbiol. 2019 Feb 17;2019:4246780. doi: 10.1155/2019/4246780. PMID: 30906323; PMCID: PMC6397969.
- Magliano E, Grazioli V, Deflorio L, Leuci AI, Mattina R, Romano P, Cocuzza CE. Gender and age-dependent etiology of community-acquired urinary tract infections. ScientificWorldJournal. 2012;2012:349597. doi: 10.1100/2012/349597. Epub 2012 Apr 26. PMID: 22629135; PMCID: PMC3351074.
- Bay AG, Anacleto F. Clinical and laboratory profile of urinary tract infection among children at the outpatient clinic of a tertiary hospital. PIDSP J. 2010;11(1):10-16.
- Gacci M, Corona G, Sebastianelli A, Serni S, De Nunzio C, Maggi M, Vignozzi L, Novara G, McVary KT, Kaplan SA, Gravas S, Chapple C. Male Lower Urinary Tract Symptoms and Cardiovascular Events: A Systematic Review and Meta-analysis. Eur Urol. 2016 Nov;70(5):788-796. doi: 10.1016/j.eururo.2016.07.007. Epub 2016 Jul 20. PMID: 27451136.
- Hwang EC, Kim SO, Nam DH, Yu HS, Hwang I, Jung SI, Kang TW, Kwon DD, Kim GS. Men with Hypertension are More Likely to Have Severe Lower Urinary Tract Symptoms and Large Prostate Volume. Low Urin Tract Symptoms. 2015 Jan;7(1):32-6. doi: 10.1111/luts.12046. Epub 2013 Dec 23. PMID: 26663649.
- Kupelian V, Araujo AB, Wittert GA, McKinlay JB. Association of moderate to severe lower urinary tract symptoms with incident type 2 diabetes and heart disease. J Urol. 2015 Feb;193(2):581-6. doi: 10.1016/j.juro.2014.08.097. Epub 2014 Aug 27. PMID: 25171906.
- Lin HJ, Weng SF, Yang CM, Wu MP. Risk of hospitalization for acute cardiovascular events among subjects with lower urinary tract symptoms: a nationwide population-based study. PLoS One. 2013 Jun 12;8(6):e66661. doi: 10.1371/journal.pone.0066661. PMID: 23776691; PMCID: PMC3680437.
- Pell JP, Cobbe SM. Seasonal variations in coronary heart disease. QJM. 1999 Dec;92(12):689-96. doi: 10.1093/qjmed/92.12.689. PMID: 10581331.
- Ibrahimi I, Shams SJ, Ahmadzai H, Sarwari Z. Seasonal variation of diabetic ketoacidosis in Nangarhar University Teaching Hospital. NUIJB. 2024:14-17.
- Anderson SL. Dapagliflozin efficacy and safety: a perspective review. Ther Adv Drug Saf. 2014 Dec;5(6):242-54. doi: 10.1177/2042098614551938. PMID: 25436106; PMCID: PMC4232499.
- Semczuk-Kaczmarek K, Płatek AE, Szymański FM. Co-treatment of lower urinary tract symptoms and cardiovascular disease - where do we stand? Cent European J Urol. 2020;73(1):42-45. doi: 10.5173/ceju.2020.0029. Epub 2020 Mar 23. PMID: 32395322; PMCID: PMC7203768.
- Fusco F, D'Anzeo G, Sessa A, Pace G, Rossi A, Capece M, d'Emmanuele di Villa Bianca R. BPH/LUTS and ED: common pharmacological pathways for a common treatment. J Sex Med. 2013 Oct;10(10):2382-93. doi: 10.1111/jsm.12261. Epub 2013 Jul 22. PMID: 23875757