More Information
Submitted: September 30, 2024 | Approved: October 09, 2024 | Published: October 10, 2024
How to cite this article: Begum A, Chowdhury W, Suman KS, Arnab KC, Akteruzzaman M, Sushanta B. Association Between Electrocardiographic Abnormalities and In-Hospital Adverse Outcome in COVID-19 Patients. J Cardiol Cardiovasc Med. 2024; 9(3): 148-152. Available from: https://dx.doi.org/10.29328/journal.jccm.1001196
DOI: 10.29328/journal.jccm.1001196
Copyright License: © 2024 Begum A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: COVID-19; Electrocardiogram; In-Hospital mortality; Cardiovascular complications
Association Between Electrocardiographic Abnormalities and In-Hospital Adverse Outcome in COVID-19 Patients
Anjuman Begum1*, Wadud Chowdhury2, Suman KS3, Arnab KC4, Md. Akteruzzaman5 and Barua Sushanta6
1Junior Consultant, Mugda Medical College Hospital, Dhaka, Bangladesh
2Professor & Head of Cardiology, Dhaka Medical College, Dhaka, Bangladesh
3Assistant Professor of Cardiology, Dhaka Medical College, Dhaka, Bangladesh
4Medical Officer, Department of Cardiology, National Institute of Cardiovascular Diseases, Dhaka, Bangladesh
5Junior Consultant, Cardiology, Sathkira Medical College Hospital, Sathkira, Bangladesh
6Assistant Registrar, Department of Cardiology, National Institute of Cardiovascular Diseases, Dhaka, Bangladesh
*Address for Correspondence: Dr. Sushanta Barua, MBBS, MD (Cardiology), Assistant Registrar, Department of Cardiology, National Institute of Cardiovascular Disease, Dhaka 1207, Bangladesh, Email: [email protected]
Background: SARS-CoV-2 is increasingly recognized for its cardiovascular complications. To address the knowledge gap in our region, this study investigated the relationship between electrocardiographic (ECG) features and in-hospital mortality among COVID-19 patients.
Methods: A prospective cohort study was conducted involving 140 RT-PCR-confirmed COVID-19 patients at Dhaka Medical College Hospital from August 2021 to July 2022. Patients were divided into two groups based on ECG findings: normal (Group A) and abnormal (Group B). Clinical data and ECG parameters were analyzed using SPSS 24.0.
Results: Patients with abnormal ECGs were older, more likely male, and presented with higher rates of dyspnea and palpitations. They were also at increased risk of severe COVID-19 and had longer hospital stays. In-hospital mortality was significantly higher in Group B (21.4% vs.4.3%). ST-T changes and atrial fibrillation were associated with increased mortality. Independent predictors of in-hospital mortality included ECG abnormalities and admission SpO₂ < 90%.
Conclusion: ECG abnormalities are significantly associated with adverse outcomes in COVID-19 patients. Further large-scale studies are warranted to strengthen these findings.
The COVID-19 pandemic, caused by SARS-CoV-2, began in late 2019 [1]. Originating in Wuhan, China, the virus rapidly spread worldwide, overwhelming healthcare systems and causing unprecedented economic disruption. India and Bangladesh were among the hardest-hit countries by October 2020, when global COVID-19 cases reached 34.8 million and deaths surpassed a million [2]. Bangladesh experienced a rapid surge in COVID-19 cases after the first three were detected on March 8, 2020. This explosive growth propelled the country to a top ranking among infected nations [3]. COVID-19 primarily manifests as a respiratory illness but has been increasingly recognized for its systemic effects, including cardiovascular complications. Previous coronavirus outbreaks, such as SARS and MERS, were associated with significant cardiac morbidity, and evidence suggests a similar pattern with COVID-19 [4]. Autopsies have revealed myocardial inflammation and clinical studies have reported a high incidence of cardiac injury among patients [5]. Studies have indicated myocardial inflammation and arrhythmias in COVID-19 patients [6-8].
The highest mortality rate among patients with cardiac involvement underscores the critical need for understanding the relationship between electrocardiographic abnormalities and adverse outcomes in these individuals. Our objective is to examine the correlation between electrocardiographic findings and in-hospital outcomes in COVID-19 patients, offering valuable insights into the cardiac implications of this disease.
Study design: Cross-section observation study.
Study setting: The study was undertaken in the COVID-19-dedicated Department of Medicine and Cardiology at Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh.
Study period: Data was collected from August 2021 to July 2022.
Study population: The study population comprised RT-PCR-confirmed COVID-19 patients admitted to the COVID-dedicated Department of Medicine and Cardiology at DMCH during the study period.
Sample size: 140
Inclusion criteria
- Age 18 years or older
- RT-PCR confirmed COVID-19 infection
- Provided informed consent
- Age less than 18 years
- Pre-existing cardiac disease
- Medication with known ECG-altering effects
- Pacemaker implantation
- Pregnancy
- Moderate to severe hepatic or renal impairment, malignancy, hypothyroidism, or hyperthyroidism
Study variables
- Demographic: Age, sex
- Clinical: Symptoms, disease severity (mild, moderate, severe, critical), SpO2 on admission
- Risk factors and comorbidities: Hypertension, diabetes mellitus, dyslipidemia, obesity, COPD/asthma
- Investigations: C-reactive protein (CRP), troponin-I, D-dimer, electrocardiogram (ECG)
- Outcome: In-hospital mortality, duration of hospital stay
Data collection
After obtaining ethical approval, 140 COVID-19 patients were enrolled. Participants were divided into two groups: Group A (normal ECG, n = 70) and Group B (abnormal ECG, n = 70).
- Detailed medical history, physical examination, and risk factor assessment were conducted.
- SpO2 was recorded on admission.
- A 12-lead ECG was performed on all patients using an advanced electrocardiograph, Model: ECG-12C. ECGs were analyzed by a senior cardiologist.
- Additional investigations (CBC, serum creatinine, SGPT, electrolytes, blood sugar, lipid profile, CRP, ferritin, LDH, chest X-ray, HRCT) were performed as indicated.
- Data was collected in a standardized form.
Data analysis
Data was analyzed using SPSS version 24. Continuous data is presented as mean ± standard deviation and categorical data as frequency and percentage. Chi-square or Fisher’s exact test was used to compare categorical variables and independent sample t-test for continuous variables. Binary logistic regression was employed to identify predictors of in-hospital mortality. Statistical significance was set at p < 0.05.
This prospective cohort study was conducted in the COVID-dedicated Department of Medicine and Cardiology, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh. After careful history taking, examination, and appropriate investigations fulfilling inclusion and exclusion criteria, a total of 140 admitted adult COVID-19 patients, irrespective of their age, sex, race, and ethnic group were included in this study. Among the study subjects 70 patients had normal ECG findings (Group A) and the other 70 patients had abnormal ECG findings (Group B). The main aim of the study was to determine the association between electrocardiographic abnormalities and in-hospital adverse outcomes in COVID-19 patients. In Table 1 clinical features of COVID-19 patients were stated and the mean age of Group-B was significantly higher than Group-A (56.70 ± 7.39 vs. 50.19 ± 8.41 years, p < 0.001). However, gender distribution was similar in both groups (74.3% in Group A and 61.4% in Group B, p > 0.05). DM (61.4% vs. 44.3%) and HTN (68.6% vs. 30%) were more predominant in the abnormal ECG group (B) and the normal ECG group (A), which were statistically significant (p < 0.05). However other risk factors were statistically similar in both groups (p > 0.05). Maximum COVID-19 patients in both groups A and B had moderate severity (95.7% vs. 85.71%). However, severe COVID-19 patients were more prone to have abnormalities. Dyspnea (75.7% vs. 30%, p < 0.001) and palpitation (64.3% vs. 42.9%, p = 0.011) were more common in patients with abnormal ECG than normal ECG. Besides, on admission, SpO2 was significantly lower in the abnormal ECG group than in normal ECG patients (91.24 ± 2.96 vs. 93.09 ± 2.08%, p < 0.001). Other clinical features were statistically similar in both groups (p > 0.05). Mean serum Troponin-I(4.13 ± 5.28 vs. 0.03 ± 0.02 ng/mL, p < 0.001) and D-dimer (5.36 ± 5.75 vs. 2.03 ± 2.20 μg/mL, p < 0.001) was significantly higher in patients with abnormal ECG than normal ECG group. Other laboratory markers were statistically similar in both groups as p > 0.05.ECG (14.29% vs. 4.3%, p < 0.05).
| Table 1: Sample Characteristics. | |||
| Variables | Group-A (n = 70) | Group-B (n = 70) | p - value |
| Age group (in years) | |||
| < 40 | 8 (11.4%) | 0 (0.0%) | 0.006c |
| 40-49 | 33 (47.1%) | 13 (18.6%) | 0.0003a |
| 50-59 | 18 (25.7%) | 31 (44.3%) | 0.021a |
| 60-69 | 11 (15.7%) | 26 (37.1%) | 0.004a |
| Mean ± SD | 50.19 ± 8.41 | 56.70 ± 7.39 | <0.001a |
| Gender | 0.103a | ||
| Male | 52 (74.3%) | 43 (61.4%) | |
| Female | 18 (25.7%) | 27 (38.6%) | 0.042a |
| Risk Factors | |||
| DM | 31 (44.3%) | 43 (61.4) | |
| HTN | 21 (30%) | 48 (68.6) | <0.001a |
| Dyslipidaemia | 26 (37.1%) | 31 (44.3) | 0.390a |
| Obesity | 12 (17.1%) | 16 (22.9) | 0.398a |
| COPD/Asthma | 2 (2.9%) | 3 (4.3) | 1.00c |
| Severity of Covid | |||
| Moderate | 67 (95.7) | 60 (85.71) | 0.042 |
| Severe | 3 (4.3) | 10 (14.29) | |
| Clinical features | |||
| Fever | 50 (71.4%) | 59 (84.3%) | 0.067 |
| Sore throat | 38 (54.3%) | 40 (57.1%) | 0.734 |
| Cough | 47 (67.1%) | 57 (81.4%) | 0.053 |
| Dyspnoea | 21 (30%) | 53 (75.7%) | <0.001 |
| Haemoptysis | 4 (5.7%) | 8 (11.4%) | 0.227 |
| Chest pain | 19 (27.1%) | 27 (38.6%) | 0.150 |
| Palpitation | 30 (42.9%) | 45 (64.3%) | 0.011 |
| On admission SpO2 | 93.09 ± 2.08 | 91.24 ± 2.96 | <0.001 |
| Cough | 47 (67.1%) | 57 (81.4%) | 0.053 |
| Laboratory investigation | |||
| Haemoglobin (gm/dL) | 10.81 ± 1.76 | 10.56 ± 1.49 | 0.371 |
| White blood cell (per mm3) | 9887.43 ± 3982.21 | 9747.86 ± 4079.19 | 0.838 |
| Neutrophil Lymphocyte Ratio | 5.83 ± 7.86 | 6.96 ± 9.75 | 0.453 |
| Total platelet count (per mm3) | 140442.86 ± 93414.71 | 135614.29 ± 77161.28 | 0.739 |
| White blood cell (per mm3) | 9887.43 ± 3982.21 | 9747.86 ± 4079.19 | 0.838 |
| Troponin I (ng/mL) | 0.03 ± 0.02 | 4.13 ± 5.28 | <0.001 |
| D-dimer(µg/mL) | 2.03 ± 2.20 | 5.36 ± 5.75 | <0.001 |
| LDH (IU/L) | 446.13 ± 218.48 | 490.57 ± 249.93 | 0.265 |
| Values are expressed as Mean ± SD and within parenthesis percentage (%) over the column in Total. p - values were obtained by aPearson Chi-square test and bIndependent Sample T-test. |
|||
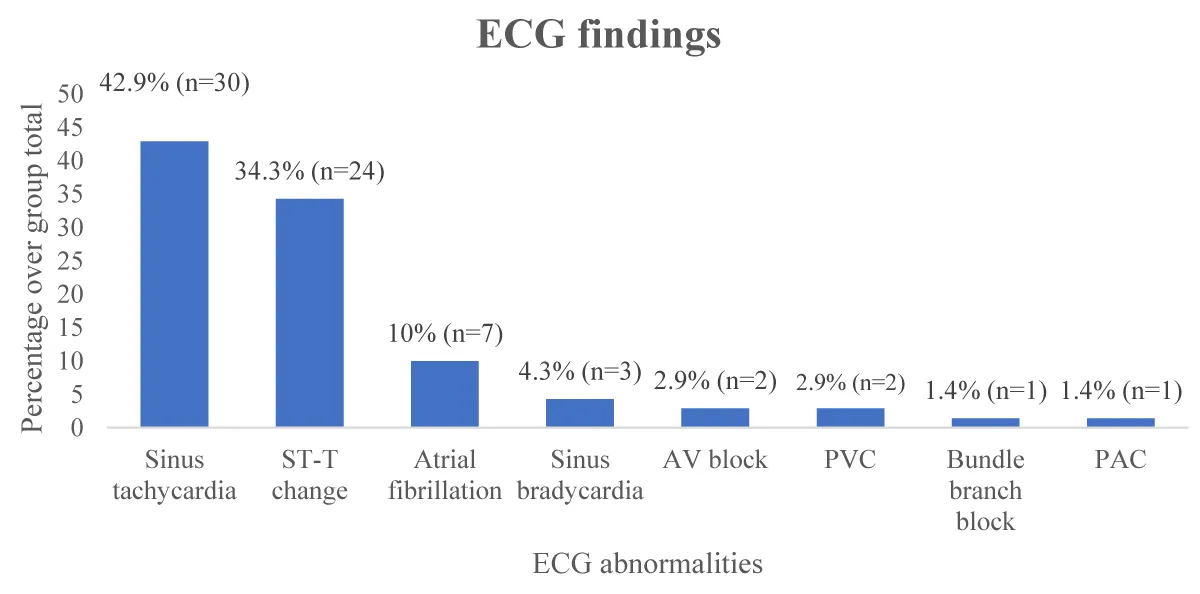
In Figure 1 out of 140 patients, 70 had normal ECG (Group-A). Among the group with abnormal ECG findings (Group-B), sinus tachycardia was maximum (42.9%) followed by ST-T change (34.3%), atrial fibrillation (10%), sinus bradycardia (4.3%), AV block (2.9%), premature ventricular contraction (2.9%), premature atrial contraction (1.4%) and right bundle branch block (1.4%).
Figure 1: Findings of COVID-19 patients with abnormal ECG (n = 70). PAC: Premature Atrial Contraction; PVS: Premature Ventricular Contraction; AVblock: Atrioventricular Block
In Table 2 COVID-19 patients with abnormal ECG findings had significantly greater in-hospital mortality rate than the normal ECG group (21.4% vs. 4.3%, p = 0.002). Besides, abnormal ECG patients had longer duration of hospital stay than normal ECG patients (11.69 ± 3.98 vs. 7.71 ± 3.79 days, p < 0.001).
| Table 2: In-hospital outcome of study patients (n = 140). | |||
| Variables | Group-A (n = 70) | Group-B (n = 70) | p - value |
| In-hospital mortality | 3 (4.3%) | 15 (21.4%) | 0.002a |
| Duration of Hospital stay (in days) | 7.71 ± 3.79 | 11.69 ± 3.98 | <0.001c |
| Values are expressed as Mean ± SD and within parenthesis percentage (%) over the column in Total. p - values were obtained by aPearson Chi-square test and cFisher’s exact test. | |||
In Table 3 ST-T change in ECG and atrial fibrillation were significantly associated with in-hospital Mortality (p < 0.05).
| Table 3: Association of abnormal ECG findings with in-hospital mortality (n = 70). | |||
| Variables | Survived (n = 55) N (%) |
Expired (n = 15) N (%) |
p - value |
| Sinus tachycardia | 0.123γ | ||
| Present | 30 (54.5) | 1 (6.7) | |
| Absent | 25 (45.5) | 14 (92.3) | |
| ST-T change | 0.001γ | ||
| Present | 15 (27.3) | 9 (60) | |
| Absent | 40 (72.7) | 6 (40) | |
| Atrial fibrillation | 0.003γ | ||
| Present | 2 (3.6) | 4 (26.7) | |
| Absent | 53 (96.4) | 11 (72.3) | |
| Sinus bradycardia | 1.00γ | ||
| Present | 3 (5.5) | 0 (0) | |
| Absent | 52 (94.5) | 15 (100) | |
| AV block | 0.241γ | ||
| Present | 1 (1.8) | 1 (6.7) | |
| Absent | 54 (98.2) | 14 (92.3) | |
| PVC | 1.00γ | ||
| Present | 2 (3.6) | 0 (0) | |
| Absent | 53 (96.4) | 15 (100) | |
| Bundle branch block | 1.00γ | ||
| Present | 1 (1.8) | 0 (0) | |
| Absent | 54 (98.2) | 15 (100) | |
| PAC | |||
| Present | 1 (1.8) | 0 (0) | 1.00γ |
| Absent | 54 (98.2) | 15 (100) | |
| PAC: Premature Atrial Contraction; PVC: Premature Ventricular Contraction; AV block: Atrioventricular block. Values are expressed within parenthesis percentage (%) over the column in total. p - values were obtained by γFisher’s exact test. | |||
In Table 4 univariate logistic regression analysis showed that age ≥50 years (OR = 5.94, 95% CI = 1.31 - 26.99), SpO2 on admission < 90% (OR = 15.02, 95% CI = 4.78 - 47.27), and having abnormal ECG findings (OR = 6.09, 95% CI = 1.68 - 22.12) were the significant risk factors for in-hospital mortality of COVID-19 patients.
| Table 5: Multivariate logistic regression to detect independent predictors of In-hospital mortality (n = 140). | ||||
| Risk factors | OR | 95% CI | p - value | |
| Lower | Upper | |||
| Age (>50 years) | 5.374 | .963 | 30.000 | .055 |
| On admission SpO2 < 90% | 18.152 | 5.079 | 64.878 | <0.001 |
| Abnormal ECG | 4.861 | 1.113 | 21.234 | .036 |
| OR: Odds Ratio; CI: Confidence Interval. | ||||
In Table 5 the multivariate model included all parameters with a p - value < 0.05 in the univariate analysis and demonstrated that on admission SpO2 < 90% and ECG abnormality were the most powerful and independent predictor of in-hospital mortality in COVID-19 patients (p < 0.05).
This study investigated the association between electrocardiographic (ECG) abnormalities and in-hospital outcomes among 140 COVID-19 patients. Our findings demonstrate that ECG abnormalities were a significant and independent predictor of in-hospital mortality (adjusted odds ratio 4.861, 95% CI 1.13 - 21.23). Patients with abnormal ECGs exhibited a notably higher mortality rate (21.4%) compared to those with normal ECGs (4.3%). These results align with previous studies highlighting the correlation between ECG changes and mortality in COVID-19 patients [9-13]. While the precise mechanisms underlying cardiac involvement in COVID-19 remain unclear, pathological findings of myocardial inflammation support the hypothesis of direct cardiac injury [5]. Additionally, indirect factors such as hypoxia, hypotension, and decreased cardiac output may contribute to these ECG abnormalities. Sinus tachycardia was the most prevalent ECG abnormality (42.9%), followed by ST-T changes (34.3%). Atrial fibrillation, significantly associated with increased mortality risk, was observed in 10% of patients. These findings corroborate previous research emphasizing the frequency of arrhythmias in COVID-19 patients [14-16]. This study observed that atrial fibrillation was significantly associated with in-hospital mortality, which was also supported by previous studies [9,11,17,18]. While the exact mechanisms are not fully understood, inflammatory cytokine release and subsequent atrial remodeling are potential contributors [19]. ST-segment changes, another significant predictor of mortality in our study, have been observed in previous research [9,11,20,21]. Although often associated with myocardial ischemia, the etiology of COVID-19 is complex and may involve various factors, including direct viral injury, systemic inflammation, and other underlying conditions. Interestingly, sinus tachycardia and bradycardia were not linked to higher mortality rates in our study, consistent with previous findings [9,22]. Nonetheless, the recognition of any ECG abnormalities should prompt clinicians to closely monitor COVID-19 patients for potential disease progression. Our study also identified age as a significant risk factor for in-hospital mortality, aligning with previous research [13,23,24]. Patients with abnormal ECGs were also more likely to experience severe or critical COVID-19.
In conclusion, ECG abnormalities, particularly atrial fibrillation, and ST-segment changes, are strong predictors of in-hospital mortality in COVID-19 patients. Early identification of these ECG abnormalities may aid in risk stratification and timely intervention. Further research is needed to elucidate the precise mechanisms underlying cardiac involvement in COVID-19.
Acknowledges study population & department of cardiology.
Ethical approval: An ethical clearance was taken from Dhaka Medical College.ERC-DMC/ECC/2021/434®
Funding source: Self
- Harapan H, Itoh N, Yufika A, Winardi W, Keam S, Te H, et al. Coronavirus disease 2019 (COVID-19): A literature review. J Infect Public Health. 2020;13(5):667–673. Available from: https://doi.org/10.1016/j.jiph.2020.03.019
- Ibrahim OR, Suleiman BM, Abdullahi SB, Oloyede T, Sanda A, Gbadamosi MS, et al. Epidemiology of COVID-19 and predictors of outcome in Nigeria: A single-center study. Am J Trop Med Hyg. 2020;103(6):2376-2381. Available from: https://doi.org/10.4269/ajtmh.20-0759
- Rahman MR, Sajib EH, Chowdhury IM, Banik A, Bhattacharya R, Ahmed H. Present scenario of COVID-19 in Bangladesh and government preparedness for facing challenges. J Adv Biotechnol Exp Ther. 2021;4(2):187-199. Available from: https://www.bsmiab.org/jabet/178-1611907708-present-scenario-of-covid-19-in-bangladesh-and-government-preparedness-for-facing-challenges
- Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352-2371. Available from: https://doi.org/10.1016/j.jacc.2020.03.031
- Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420-422. Available from: https://doi.org/10.1016/s2213-2600(20)30076-x
- Chen C, Zhou Y, Wang DW. SARS-CoV-2: A potential novel etiology of fulminant myocarditis. Herz. 2020;45(3):230-232. Available from: https://doi.org/10.1007/s00059-020-04909-z
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395(10223):507-513. Available from: https://doi.org/10.1016/s0140-6736(20)30211-7
- Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259-260. Available from: https://doi.org/10.1038/s41569-020-0360-5
- Antwi-Amoabeng D, Beutler BD, Singh S, Taha M, Ghuman J, Hanfy A, et al. Association between electrocardiographic features and mortality in COVID-19 patients. Ann Noninvasive Electrocardiol. 2021;26(4):1-7. Available from: https://doi.org/10.1111/anec.12833
- Aikawa T, Takagi H, Ishikawa K, Kuno T. Myocardial injury characterized by elevated cardiac troponin and in-hospital mortality of COVID-19: An insight from a meta-analysis. J Med Virol. 2021. Available from: https://doi.org/10.1002/jmv.26108
- De Carvalho H, Leonard-Pons L, Segard J, Goffinet N, Javaudin F, Martinage A, et al. Electrocardiographic abnormalities in COVID-19 patients visiting the emergency department: A multicenter retrospective study. BMC Emerg Med. 2021;21(1):1-7. Available from: https://doi.org/10.1186/s12873-021-00539-8
- Rosén J, Noreland M, Stattin K, Lipcsey M, Frithiof R, Malinovschi A, et al. ECG pathology and its association with death in critically ill COVID-19 patients: A cohort study. PLoS ONE. 2021;16(12):1-15. Available from: https://doi.org/10.1371/journal.pone.0261315
- Savelloni G, Gatto MC, Cancelli F, Barbetti A, Dezza FC, Franchi C, et al. Prognostic value of 12-leads electrocardiogram at emergency department in hospitalized patients with coronavirus disease-19. Available from: https://doi.org/10.3390/jcm11092537
- Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390. Available from: https://doi.org/10.1016/j.pcad.2020.03.001
- Lombardi CM, Carubelli V, Iorio A, Inciardi RM, Bellasi A, Canale C, et al. Association of troponin levels with mortality in Italian patients hospitalized with coronavirus disease 2019: Results of a multicenter study. JAMA Cardiol. 2020;5(11):1274-1280. Available from: https://doi.org/10.1001/jamacardio.2020.3538
- McCullough SA, Goyal P, Krishnan U, Choi JJ, Safford MM, Okin PM. Electrocardiographic findings in coronavirus disease-19: Insights on mortality and underlying myocardial processes. J Card Fail. 2020;26(7):626-632. Available from: https://doi.org/10.1016/j.cardfail.2020.06.005
- Romiti GF, Corica B, Lip GYH, Proietti M. Prevalence and impact of atrial fibrillation in hospitalized patients with COVID-19: A systematic review and meta-analysis. J Clin Med. 2021;10(11):2490. Available from: https://doi.org/10.3390/jcm10112490
- Yarmohammadi H, Morrow JP, Dizon J, Biviano A, Ehlert F, Saluja D, et al. Frequency of atrial arrhythmia in hospitalized patients with COVID-19. Am J Cardiol. 2021;147:52-57. Available from: https://doi.org/10.1016/j.amjcard.2021.01.039
- Harada M, Van Wagoner DR, Nattel S. Role of inflammation in atrial fibrillation pathophysiology and management. Circ J. 2015;79(3):495-502. Available from: https://doi.org/10.1253/circj.CJ-15-0138
- Awal A, Al Mamun KS, Karim MR, Azad MSU, Ahmed FU. Prognostic value of electrocardiographic abnormalities and troponin-I elevation in hospitalized COVID-19 patients. Bangladesh Heart J. 2021;36(2):105-112. Available from: https://doi.org/10.3329/bhj.v36i2.56036
- Hu B, Deng Q, Zhou Q. Cardiac involvement of COVID-19: Looking forward to novel discoveries and clinically valuable evidence. Int J Cardiol. 2020. Available from: https://doi.org/10.1016/j.ijcard.2020.05.049
- Kumar S, Arcuri C, Chaudhuri S, Gupta R, Aseri M, Barve P, et al. A novel study on SARS-CoV-2 virus associated bradycardia as a predictor of mortality: Retrospective multicenter analysis. Clin Cardiol. 2021;44(6):857-862. Available from: https://doi.org/10.1002/clc.23622
- Izcovich A, Ragusa MA, Tortosa F, Lavena Marzio MA, Agnoletti C, Bengolea A, et al. Prognostic factors for severity and mortality in patients infected with COVID-19: A systematic review. PLoS One. 2020;15(11). Available from: https://doi.org/10.1371/journal.pone.0241955
- Karbalai Saleh S, Oraii A, Soleimani A, Hadadi A, Shajari Z, Montazeri M, et al. The association between cardiac injury and outcomes in hospitalized patients with COVID-19. Intern Emerg Med. 2020;15(8):1415-1424. Available from: https://doi.org/10.1007/s11739-020-02466-1