More Information
Submitted: December 30, 2024 | Approved: January 09, 2025 | Published: January 10, 2025
How to cite this article: Haqmal Z, Zaheer I. A Study of Endoscopic and Clinical Profile of Dyspepsia in Afghan Momand Medical Complex & Research Center, Eastern Region, Nangarhar, Afghanistan. J Cardiol Cardiovasc Med. 2025; 10(1): 005-007. Available from:
https://dx.doi.org/10.29328/journal.jccm.1001203
DOI: 10.29328/journal.jccm.1001203
Copyright license: © 2025 Haqmal Z, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Dyspepsia; Dysphagia; Candidiasis; Esophagitis; Hiatus hernia; Esophageal growth; Esophageal varices; Gastritis; Polyps; Ulcers; Snuff and Smoking
A Study of Endoscopic and Clinical Profile of Dyspepsia in Afghan Momand Medical Complex & Research Center, Eastern Region, Nangarhar, Afghanistan
Ziaulhaq Haqmal* and Ismatullah Zaheer
Afghan Momand Medical Complex & Research Center, Eastern Region, Nangarhar, Afghanistan
*Address for Correspondence: Ziaulhaq Haqmal, Afghan Momand Medical Complex & Research Center, Eastern Region, Nangarhar, Afghanistan, Email: [email protected]; [email protected]
Dyspepsia refers to acute, chronic, or recurrent pain or discomfort centered in the upper abdomen. An international committee of clinical investigators (Rome III Committee) has defined Dyspepsia as Epigastric pain or Burning, early satiety, or postprandial fullness Dyspepsia occurs in 15 % of the Adult population and accounts for 3% of general medical office visits. The descriptive study was carried out in Eastern Afghanistan, Afghan Momand Medical Complex & Research Center, Department of Gastroenterology, during the years 2023-2024. To know the Clinico-Endoscopy of Dyspepsia, for patients who present with investigated Dyspepsia to Gastroenterological OPD & IPD. The study result showed, there were a total of patients 467, and of these patients 230 were Male and 237 were Female. According to the Age, 45 patients were under Age < 20, 219 patients were between the ages 21-40 years, 130 patients were between ages 41-60 years and 73 patients were over 60 years of Age. However according to the presentation, 357 patients had Dyspepsia, 59 patients had Dysphagia, 13 patients had Chronic Liver Diseases & Screened for Varices, 3 patients presented after Acid ingestion, 2 patients had Anemia, 11 patients had persistent vomiting and 22 patients had suspected GI-Bleeding. Furthermore in Esophageal findings from a total of 467 patients 34 patients had Esophageal Candidacies, 6 patients had Esophageal Narrowing, 25 patients had Esophageal Growth, 71 patients had Hiatus Hernia, 180 patients had LA Grade A Esophagitis, 21 patients had LA Grade B Esophagitis, 6 patients had LA Grade C Esophagitis, 3 patient had LA Grade D Esophagitis. 16 patients had Lax Lower Esophageal Sphincter, 9 Patients had High-Risk Esophageal Varices, 3 patients had Small Esophageal Varices and 150 patients had Normal Esophagus and in Gastric findings from total all above patients, 4 patients had Antral Gastritis, 50 patients had Corpus Gastritis, 1 patient had Fundal Gastritis, 4 patients had Nodular Gastritis, 199 patients had Pan-Gastritis, 108 patients have Severe Pan Erosive Gastritis, 23 patient had Gastric Erosions, 6 patients had PHG (Portal Hypertensive Gastropathy), 3 Patients had Fundal Varices, 5 patients had Gastric Polyps, 5 patients had Gastric Growth, 2 patients had Pyloric Stenosis, 8 patients stomach not seen due to Esophageal Growth, 67 patients stomach were normal. In the present study there were Duodenal findings from a total of the above patients 48 had Duodenitis, 2 patients had Duodenal Polyps, 2 patients had duodenal ulcers, 1 patient had Duodenopathy, 2 patients had Duodenopathy, 2 patients Duodenum not seen due to Pyloric Stenosis and 413 patients Duodenum were normal. Regarding the habits in our study in which a total of 467 patients were examined 135 of the above patients had snuff habits, 103 patients had smoking habits, 2 patients were Heroin addicts and 227 of the total patients didn’t have any habits (the majority of them were using spicy food, overfeeding, drinking of nonalcoholic beverages, fatty foods, NSAIDs ...) and the higher incidence of Dyspepsia was in Female patients, Also with the age between 21-40 years (43%) patients, Also the higher incidence of Dysphagia 47% were in patients with Age >60 years, the Endoscopy showed that 83% patients had Gastritis also higher incidence regarding the habits 29% had snuff habit and 22% had a smoking habit.
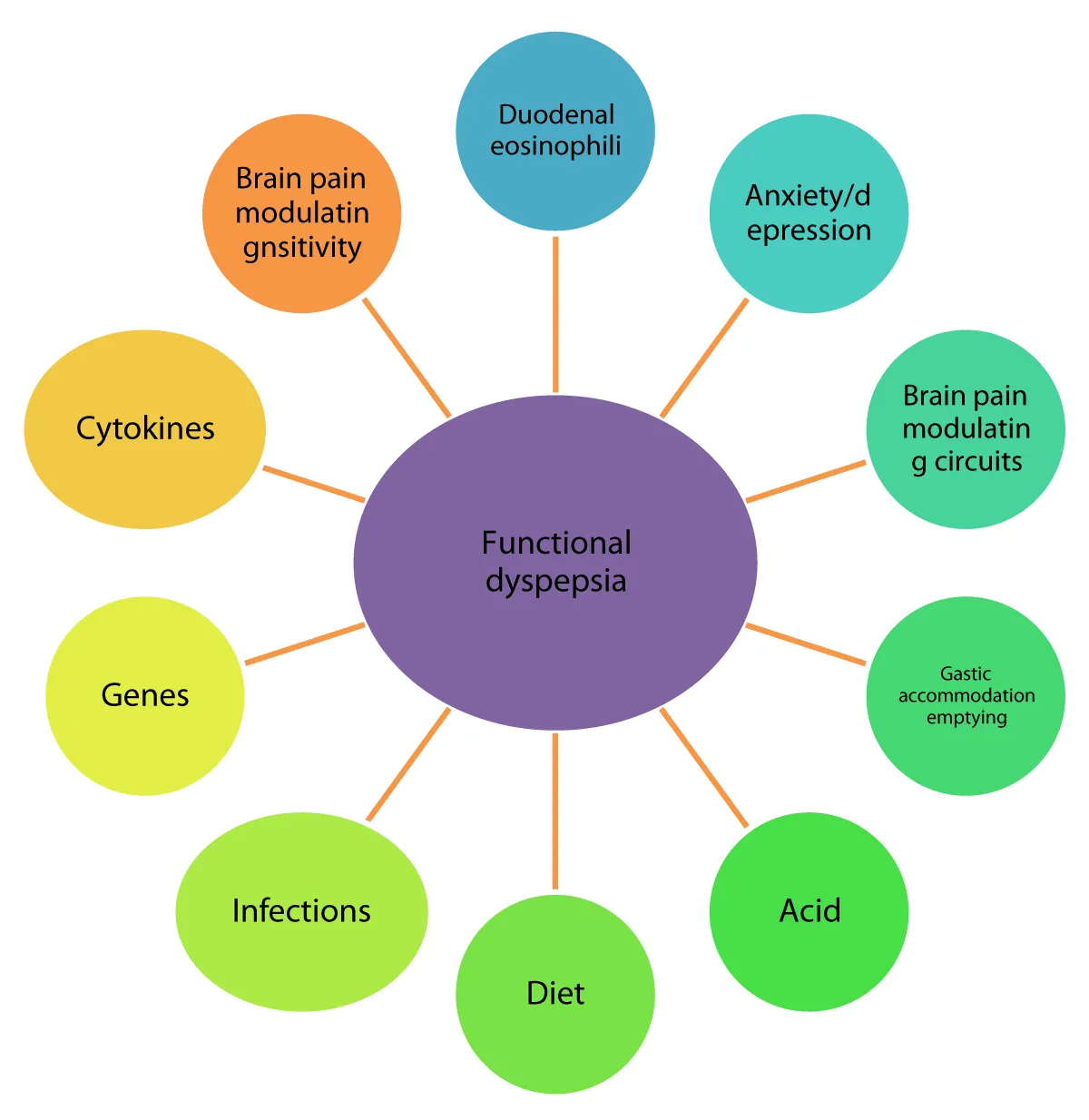
Dyspepsia is a Greek word meaning “dys” (bad or difficult) and “peptin” (to digest), which is described by patients as indigestion; both these words are a poor expression, as Dyspepsia has no relation to the digestion of food. Dyspepsia refers to upper abdominal symptoms usually following intake of food, which appear to arise from an abnormality in the upper gastrointestinal tract. Dyspepsia is a symptom and not a diagnosis (Figure 1). Symptoms may last for decades (even a lifetime) and remissions and relapses are common. It is one of the most common gastrointestinal malady affecting at least 25% of the population during a year. Its prevalence varies in different countries, depending upon the prevalence of Helicobacter pylori (H. pylori) infection, obesity, drug - alcohol - tobacco intake, and spices in the diet; furthermore, a significant and varying number of subjects do not seek medical treatment [1-4].
Figure 1: Pathophysiology of Dyspepsia [4].
Symptomatology
Symptoms of Dyspepsia are due to diseases of stomach-duodenum and include: abdominal pain above the umbilicus, retrosternal burning, regurgitation, belching (or eructation), abdominal distension (fullness), nausea, vomiting (occasional), early satiety after meals. Functional Dyspepsia was defined as “Upper Abdominal or Retro-sternal pain or discomfort, Heartburn, Nausea or Vomiting or other symptoms considered to be referable to the proximal alimentary tract and lasting for more than 4 weeks, unrelated to exercise and for which no focal lesion or systemic disease can be responsible.
Camilleri, et al. (2005) reported that excessive fullness after eating or the inability to finish a normal-sized meal and recurrent epigastric pain are common symptoms and reasons for consulting medical professionals, Structural investigations, including Esophago Gastro Duodenoscopy (EGD), usually fail to identify an obvious organic explanation, and these patients are labeled as having functional Dyspepsia (FD).
Other terms applied to the same condition in the past have included nervous Dyspepsia, non-ulcer Dyspepsia (NUD), and essential Dyspepsia, but FD is now the most common diagnosis and is included in the Rome criteria classification of functional gastrointestinal disorders (FGIDs). FD is important because it is not only highly prevalent but also impairs quality of life, work performance, and family relationships and incurs a high healthcare cost worldwide (Lacy, et al., 2013). Whiting, et al. (1853) in the eighteenth century reported that stomach disorders” became an obsession of developed countries. Hoffer (2007) reported that descriptions of symptoms of upper gastrointestinal date back thousands of years while the term Dyspepsia was first coined by Baron, et al. (2006).
The study was conducted in Eastern Afghanistan during 2023 and 2024. This paper describes the clinical presentation of 467 patients suffering from’ Dyspepsia’ at the time of their visit to the Afghan Momand Medical Complex & Research Center, Department of Gastroenterology. Cases were studied on a prospective base by scrutiny of the patient’s case records and in the vast majority of cases by personal interview and all the patients were withdrawn from all medications causing Dyspepsia. Endoscopy was done in patients under 20 years, 21-40, 41-60, and more than 60 years of age with Dyspepsia. The disease categories considered in this study were in Endoscopic finding: LA Grade Esophagitis, Candidiasis, Esophageal Varices, Esophageal Growth, Gastritis, Duodenitis, Gastric & Duodenal ulcer, Gastric growth, regarding the habits in our study 29% of the above patients had snuff habits, 22% had smoking habits, 2 patients had heroin habits and 37% of the total patients didn’t have any habits (the majority of them were using spicy food, overfeeding, drinking nonalcoholic beverages, fatty foods, NSAIDs ...).
Ethical declarations
The author certifies the permission regarding the ethics and the study has been done according to the research rules.
Dyspepsia and age of patients
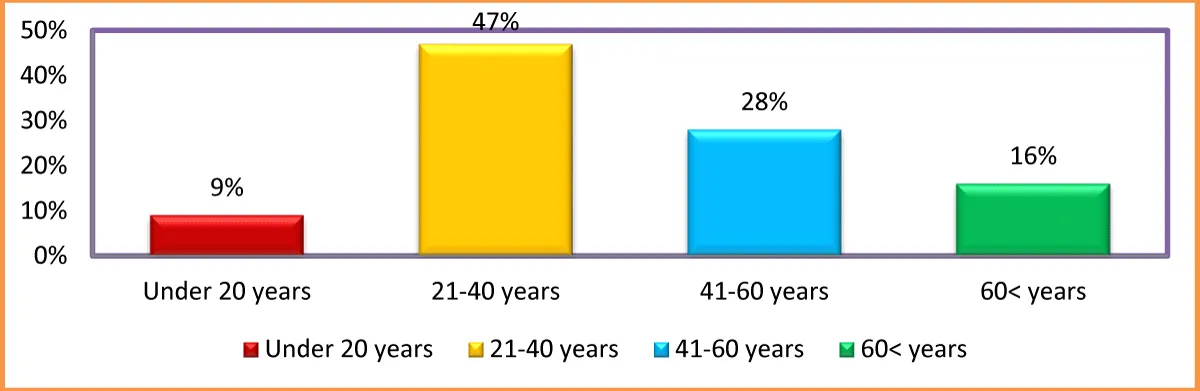
The causes of Dyspepsia are shown in Table 1 and the prevalence Figure 2, given are derived from the 100 people who are referred to gastroenterologists for investigation and definitive diagnosis. Causes of Dyspepsia reduction with increased age of patients. It can be reasonably assumed that more people with functional Dyspepsia under age 30 years old patients having about 34% Dyspepsia while more than 60-year-old patients resulted in 14% due to higher stress, Smoking, and Tobacco use under 30 years than older patients Similar were found early from M.K.C.G Medical College Hospital, Berhampur, India by (Jose, 2015). The data also indicated that 30-40, 41-50, and 51-60-year-old patients had 23%, 15%, and 16 % Dyspepsia, respectively. Similar results were found by Desai, et al. (2018) reported a study from urban Mumbai, India found that Dyspepsia was more prevalent in adults >40. The data regarding the clinical profile of Dyspepsia in Northeast India where there is a significant consumption of tobacco and smoking is lacking. Shah, et al. 2001 studies in Asia that dyspepsia is more common in the younger age groups (Figure 2 & Table 1).
Figure 2: Age-wise Percentage of the patients having Dyspepsia in AMMC& Research Center.
| Table 1: Age-wise distribution of Percentage of patients affected with Dyspepsia. | |||
| S/no | Age of the patients | N = 467 patients | Percentage of patients |
| 1 | Under 20 years | 45 | 9% |
| 2 | 21-40 years | 219 | 47% |
| 3 | 41-60 years | 130 | 28% |
| 4 | 60< years | 73 | 16% |
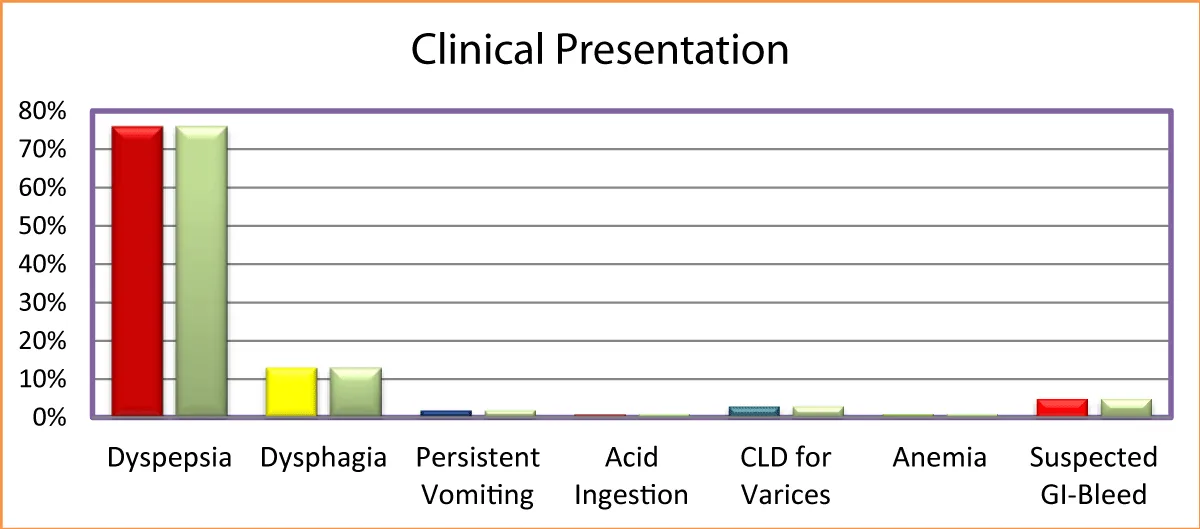
Clinical presentation to gastroenterology department
The data regarding clinical presentation in Table 3 show that 357 patients had Dyspepsia, 59 patients had Dysphagia, 13 patients had Chronic Liver Diseases (CLD) & Screen for Varices, 3 patients were presented after Acid ingestion, 2 patients had Anemia, 11 patients had persistent vomiting and 22 patients had suspected GI-Bleeding (Figure 3 & Table 2).
Figure 3: Percentage of Patients according to Clinical Presentation.
| Table 2: Percentage of Patients according to Clinical Presentation. | |||
| S/No | Clinical Presentation | Number of Patients | Percentage of Patients |
| 1 | Dyspepsia | 357 | 76% |
| 2 | Dysphagia | 59 | 13% |
| 3 | Persistent Vomiting | 11 | 2% |
| 4 | Acid Ingestion | 3 | 1% |
| 5 | CLD for Varices | 13 | 3% |
| 6 | Anemia | 2 | 1% |
| 7 | Suspected GI-Bleed | 22 | 5% |
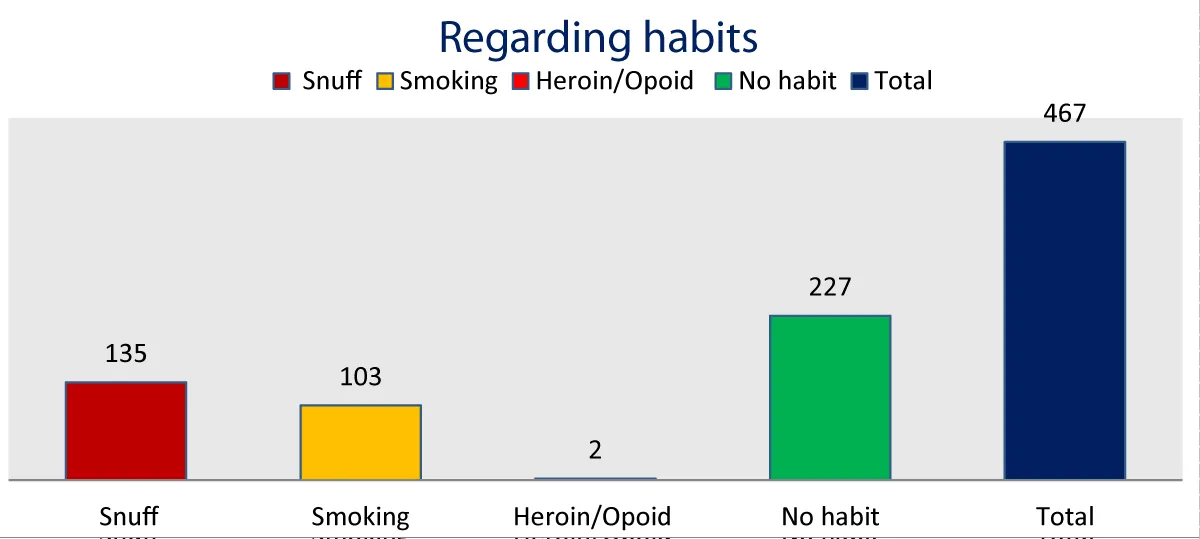
Regarding the habits in our study in which a total of 467 patients were examined 135 of the above patients had snuff habits, 103 had smoking habits, 2 patients were heroin addicts and 227 of the total patients didn’t have any habits (the majority of them were using spicy food, overfeeding, drinking of nonalcoholic beverages, fatty foods, NSAIDs (Figure 4 & Table 3).
Figure 4: Dyspepsia cases regarding habits.
| Table 3: Dyspepsia cases regarding habits. | ||
| S/No | Habits | Number of Patients |
| 1 | Snuff | 135 |
| 2 | Smoking | 103 |
| 3 | Heroin/Opioid | 2 |
| 4 | No habit | 227 |
| 5 | Total | 467 |
The present study demonstrated that Dyspepsia, especially in the elderly is associated with a significant underlying disease. Most of the patients are associated with alarm features. There was also a high percentage of patients with Gastritis followed by NFD and Duodenal ulcer. Thus all the patients who are above 20 years were with have higher cases of Dyspepsia than older patients also regarding the Habits Majority of the patients had Snuff habits some of them had smoking habits, as our society is Islamic Alcohol use was not the major cause of Dyspepsia. Also, the cases of Dysphagia and Esophageal Growth were more common in Female patients and patients who were more than 40 years of Age.
- Feldman M, Friedman LS, Brandt LJ. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 12th ed. Elsevier; 2020. eBook ISBN: 9780323710947.
- Fauci AS, Jameson JL, Kasper DL, Longo DL. Harrison's Principles of Internal Medicine. 21st ed. McGraw-Hill Professional; [cited 2025 Jan 9]. Available from: https://accesspharmacy.mhmedical.com/book.aspx?bookid=3095
- Friedman S, Blumberg RS, Saltzman JR. Greenberger's CURRENT Diagnosis & Treatment, Gastroenterology, Hepatology, and Endoscopy.4th ed. McGraw Hill Education; 2022. ISBN: 9781260473438. Available from: https://accessmedicine.mhmedical.com/book.aspx?bookid=3204
- Talley NJ. Functional dyspepsia: new insights into pathogenesis and therapy. Korean J Intern Med. 2016 May;31(3):444-456. doi: 10.3904/kjim.2016.091. Available from: https://doi.org/10.3904/kjim.2016.091