More Information
Submitted: May 22, 2025 | Approved: May 27, 2025 | Published: May 28, 2025
How to cite this article: de Matos Luz CD, Horn AM, Dias VR, Fornari V, de Athayde Soares R. The Experience of Merit Wrapsody® Covered Stent for the Treatment of Popliteal Artery Aneurysms: an Alternative Device off the Shelf in a Case Series Report. J Cardiol Cardiovasc Med. 2025; 10(3): 093-097.
Available from: https://dx.doi.org/10.29328/journal.jccm.1001214
DOI: 10.29328/journal.jccm.1001214
Copyright license: © 2025 de Matos Luz CD, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The Experience of Merit Wrapsody® Covered Stent for the Treatment of Popliteal Artery Aneurysms: an Alternative Device off the Shelf in a Case Series Report
Cristiano Dias de Matos Luz, Alexandre Mariante Horn, Vinícius Renan Dias, Vinícius Fornari and Rafael de Athayde Soares*
Hospital for Public Servants of the State of São Paulo, IAMSPE, Brazil
*Address for Correspondence: Rafael de Athayde Soares, Hospital for Public Servants of the State of São Paulo, IAMSPE, Av. Ibirapuera 981, Brazil, Email: [email protected]; [email protected]
In this paper, we aimed to report the use of Merit Wrapsody® for popliteal artery aneurysms. We describe a case series involving 5 patients submitted to endovascular repair with Merit Wrapsody® for popliteal artery aneurysms. Merit Wrapsody® is a flexible self-expanding endoprosthesis indicated for use in hemodialysis patients for the treatment of stenosis or occlusion within the dialysis outflow circuit of an Arteriovenous (AV) fistula or AV graft, consisting of Nitinol, ePTFE, PTFE structure. In a case series communication, we aimed to describe the feasibility of a PTFE-lined stent for percutaneous treatment of conditions other than AV fistula obstruction. We report the successful use of Wrapsody® to percutaneously treat popliteal artery aneurysms. This case series illustrates the feasibility of the “off-label” use of self-expanded Wrapsody endoprosthesis to percutaneously treat arterial pathology conditions, especially popliteal artery aneurysms with satisfactory and excellent results.
It is well known that popliteal artery aneurysm represents 70% of all Peripheral Arterial Aneurysms (PAA), furthermore, the most common surgical treatment is ligation of the popliteal aneurysms associated with a femoropopliteal bypass with the great saphenous vein [1]. Covered stents formerly reserved for arteriovenous fistulas, iliac aneurysms, or iatrogenic perforations and ruptures. However, recent studies have provided encouraging results of covered stents compared with open surgeries for popliteal artery aneurysms, demonstrating that endovascular therapy offers similar results, with the same safety and efficacy for limb salvage rates and secondary patency [2,3].
Merit Wrapsody is a flexible self-expanding endoprosthesis indicated for use in hemodialysis patients for the treatment of stenosis or occlusion within the dialysis outflow circuit of an Arteriovenous (AV) fistula or AV graft, consisting of Nitinol, ePTFE, PTFE structure. Several studies have shown promising target lesion patency rates of 100% at 30 days (45 of 45 patients had reached 30 days of follow-up). The target lesion primary patency for the patients who had completed 12 months of follow-up was 84.6% (33 of 39) [4]. Indeed, although widely used in venous indications, a case report has shown positive outcomes for arterial use of the use of Wrapsody in popliteal artery aneurysms, with 1-year follow-up [5]. In this study, we aimed to report the use of Merit Wrapsody for popliteal artery aneurysms in a case series (5 patients).
Case 1
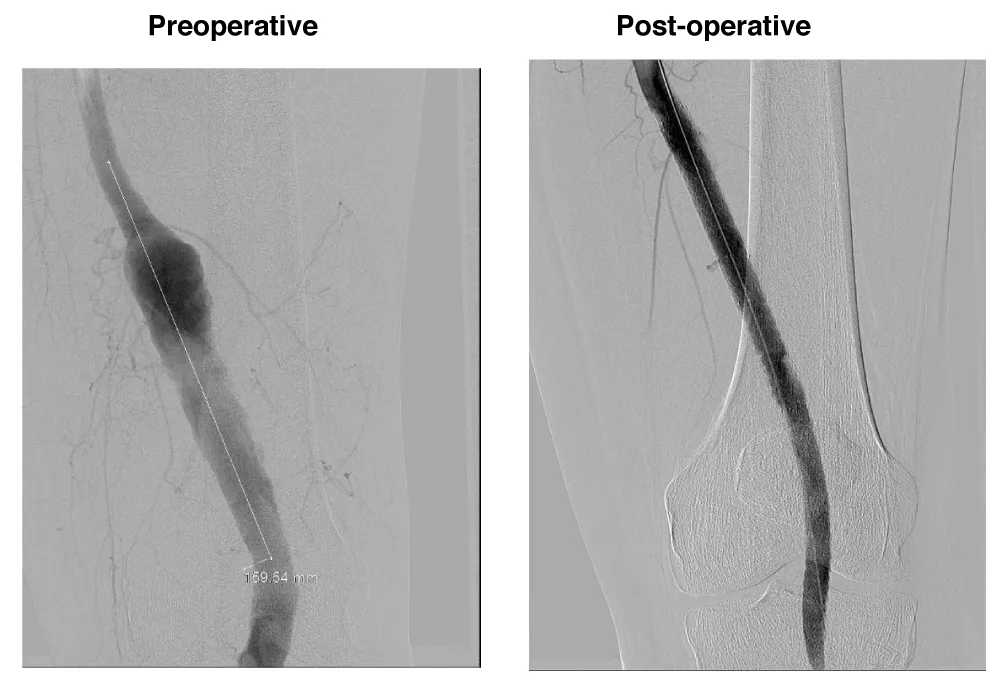
A male patient, 63 years, with arterial hypertension and dyslipidemia, was admitted with an asymptomatic popliteal artery aneurysm in the left Lower limb measuring 3,1 cm, discovered after an acute arterial occlusion at the right Lower limb due to popliteal artery aneurysm thrombosis. The following measures were observed: proximal neck diameter 10,21 mm, distal neck diameter 9,98 mm, with a diameter of 56 mm and 250 mm aneurysm length. The patient underwent endovascular treatment with the popliteal implant of endoprosthesis Wrapsody® 12x80 mm at the distal neck, followed by the implant of Wrapsody 12x125 mm and Wrapsody 12x80 mm at the proximal neck, followed by catheter balloon dilatation. The final image showed excellent results with no endoleaks (Figure 1). The patient was discharged from the hospital on the on the first postoperative day with Rivaroxaban 20 mg/day and a 6-month follow-up showed endoprosthesis patency with excellent flow and run-off.
Figure 1: Endovascular repair of a 63-year-old male with left popliteal artery aneurysm (56 mm): Preoperative imaging shows fusiform dilation of the popliteal artery. Postoperative image demonstrates successful deployment of three Wrapsody® endoprostheses (12×80 mm, 12×125 mm, and 12×80 mm) with complete exclusion of the aneurysm and no evidence of endoleak.
Case 2
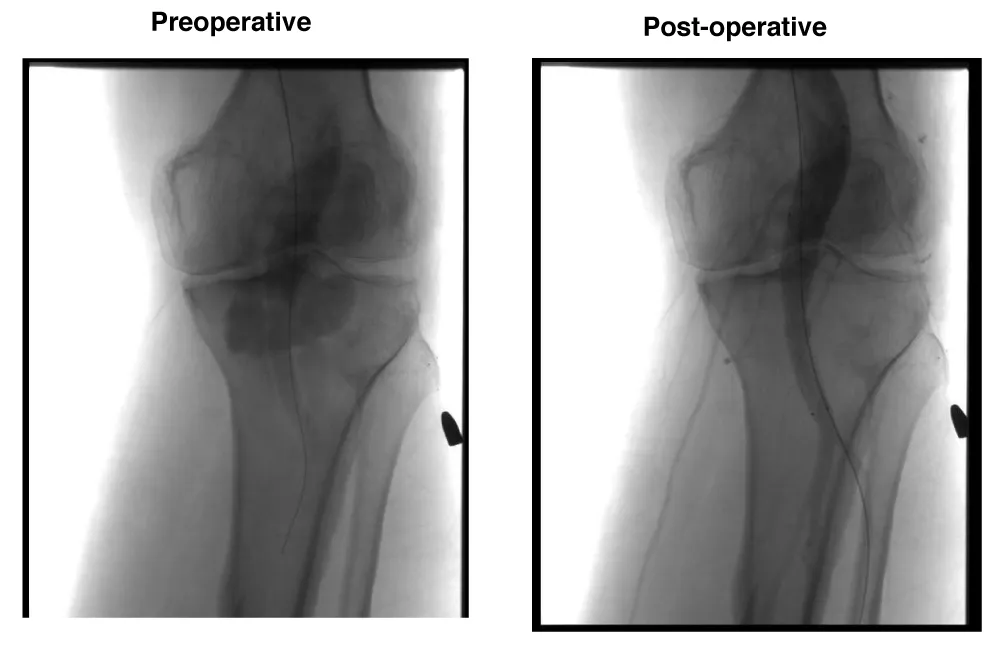
Male patient, 51 years, with arterial hypertension and a history of trauma due to gunshot. The patient evolved with a high-output arteriovenous fistula in the popliteal region causing significant symptoms and 30 mm a popliteal aneurysm. Due to this important symptom, the patient was scheduled to undergo an endovascular procedure with the popliteal implant of endoprosthesis Wrapsody® 12x80 mm at the distal neck, followed by the implant of Wrapsody 14x80 mm and two Wrapsody 16x80 mm at the proximal neck, followed by catheter balloon dilatation. (Figure 2). The patient was discharged from the hospital first day post-operative with Rivaroxaban 20 mg/day and a 6-month follow-up showed endoprosthesis patency and no endoleaks with complete resolution of the previous symptoms.
Figure 2: Endovascular treatment of a 51-year-old male with traumatic arteriovenous fistula and popliteal aneurysm (30 mm): Preoperative angiogram displays fistula formation and aneurysmal dilation. Postoperative image shows complete aneurysm exclusion using four Wrapsody® stents (12×80 mm, 14×80 mm, and two 16×80 mm), with restored vessel continuity and resolution of fistulous flow.
Case 3
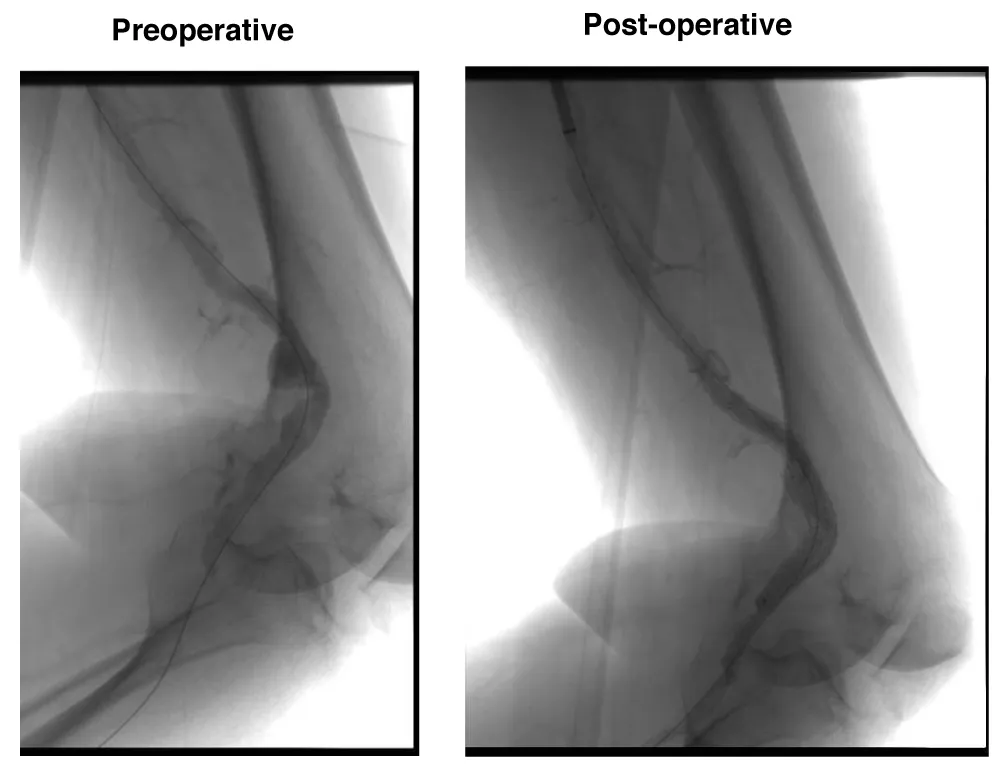
A male patient, 74 years old, with arterial hypertension and diabetes was admitted with right Lower limb rest pain due to acute arterial occlusion. The patient underwent AngioCT scan which demonstrated a 26 mm popliteal artery aneurysm thrombosis. The patient was submitted to endovascular surgery with popliteal implant of endoprosthesis Wrapsody® 12x80 mm at distal neck and Wrapsody 12x80 mm at proximal neck, followed by catheter balloon dilatation, after proper intra-arterial thrombolysis (Figure 3). The patient was discharged from the hospital on the first day post-operative with Rivaroxaban 20mg/day and a 2-month follow-up showed endoprosthesis patency with complete resolution of the previous symptoms.
Figure 3: Endovascular thrombolysis and stenting of a 74-year-old male with acute thrombosed 26 mm popliteal artery aneurysm: Preoperative CT angiography reveals occlusion and aneurysmal dilation. Postoperative image confirms successful thrombolysis and exclusion with two Wrapsody® stents (12×80 mm each), with reestablished distal perfusion.
Case 4
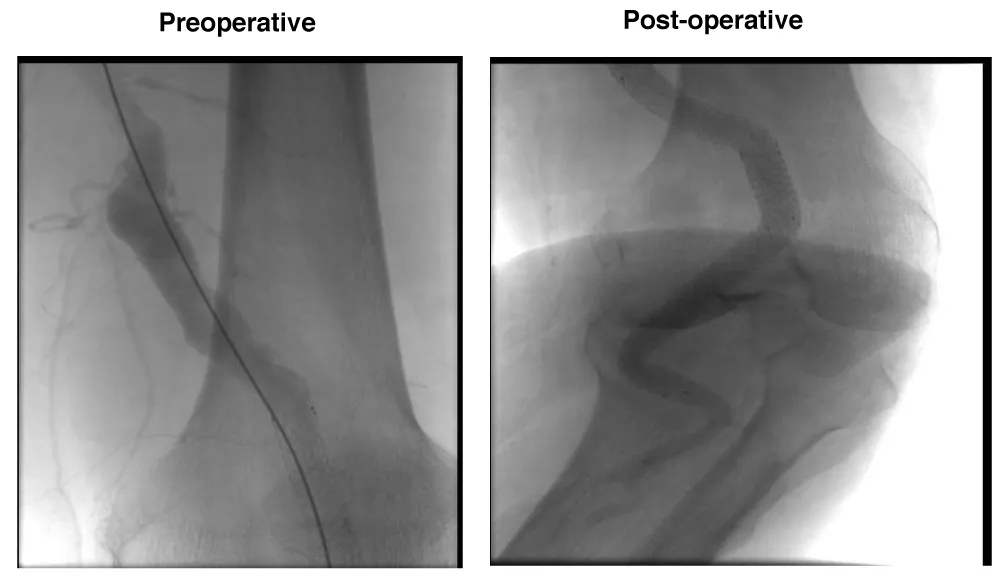
A male patient, 81 years, active smoker, with arterial hypertension and diabetes was admitted with right Lower limb distal microembolization, due to a 24 mm popliteal arterial aneurysm. The patient was submitted to endovascular surgery with the popliteal implant of endoprosthesis Wrapsody® 10x125 mm at distal neck, followed by an implant of Wrapsody 10x125 mm and Wrapsody 12x80 mm at proximal neck, followed by catheter balloon dilatation. (Figure 4).
Figure 4: Repair of a 24 mm popliteal artery aneurysm in an 81-year-old male with distal embolization: Preoperative image highlights microembolization signs and aneurysm. Postoperative angiogram demonstrates successful repair using three Wrapsody® endoprostheses (10×125 mm, 10×125 mm, 12×80 mm) with full restoration of patency and distal flow.
The patient was discharged from the hospital first day post-operative with Rivaroxaban 20 mg/day and a 1-month follow-up showed endoprosthesis patency with complete resolution of the previous symptoms.
Case 5
A male patient, 86 years old, with arterial hypertension, and diabetes was admitted, congestive heart failure, and a history of infra-renal abdominal aortic surgery was admitted with right Lower limb disabling claudication. AngioCT-Scan 60 mm popliteal artery aneurysm. The patient was submitted to endovascular surgery with the popliteal implant of endoprosthesis Wrapsody® 9x125 mm at the distal neck, followed by an implant of Wrapsody 10x125 mm and Wrapsody 10x50 mm at the proximal neck, followed by a catheter balloon dilatation (Figure 5). The patient was discharged from the hospital first day post-operative with Rivaroxaban 20 mg/day and a 1-month follow-up showed endoprosthesis patency with complete resolution of the previous symptoms.
Figure 5: Endovascular exclusion of a large 60 mm aneurysm in an 86-year-old male with disabling claudication: Preoperative imaging shows a saccular aneurysm in the popliteal segment. Postoperative view illustrates complete aneurysm sealing using Wrapsody® stents (9×125 mm, 10×125 mm, 10×50 mm) with proper distal runoff and no endoleak.
All those data are summarized at Table 1.
| Table 1: Summary of indications, procedural details, and outcomes in five patients treated with Merit Wrapsody® stents for popliteal artery aneurysms. All patients received Rivaroxaban 20 mg/day postoperatively. | |||
| Cases Report | Indications | Procedural details | Outcomes |
| Case 1 | Popliteal artery diameter 56mm | 3 Wrapsody 12x80, 12x125 and 12x80 mm | 6-month patency, asymptomatic, taking Rivaroxaban 20 mg/day. |
| Case 2 | Arteriovenous fistula in popliteal vessels after a trauma | 4 Wrapsody: 12x80, 14 x80, 16x80 and 16x80 mm | 6-month patency, asymptomatic, taking Rivaroxaban 20 mg/day. |
| Case 3 | Acute arterial occlusion and popliteal artery thrombosis | 2 Wrapsody: 12x80 and 12x80 mm. | 2-month patency, asymptomatic, taking Rivaroxaban 20 mg/day. |
| Case 4 | Microembolization of popliteal artery aneurysm | 3 Wrapsody: 10x125, 10x125 and 12x80 mm. | 1-month patency, asymptomatic, taking Rivaroxaban 20 mg/day. |
| Case 5 | Disabling claudication due to a 60mm popliteal artery aneurysm | 3 Wrapsody: 9x125, 10x125 and 10x50 mm. | 1-month patency, asymptomatic, taking Rivaroxaban 20 mg/day. |
| Note:All patients received Rivaroxaban 20 mg/day postoperatively as part of the standard anticoagulation regimen following endovascular treatment with Wrapsody® stents. | |||
This paper presents a challenging case series report of patients with popliteal artery aneurysms with severe comorbidities, treated with endovascular repair with a new device for off-the-shelf use. Popliteal Artery Aneurysms (PAAs) represent 70% of peripheral aneurysms. Despite this, their estimated incidence is 0.1% [5,6]. PAAs mainly affect people aged > 65 years and have two characteristic features: they are often bilateral, and in 40% to 60% of cases, aneurysmal disease is also observed at other levels. Most PAAs are asymptomatic, although up to 30% may show complications, especially those related to embolization to infrapopliteal vessels or aneurysm thrombosis. PAA rupture has only rarely been reported [5,6].
Currently, the two most widely accepted therapeutic options for the treatment of a PAA is exclusion, followed by venous or prosthetic bypass and the use of a stent graft for endovascular repair. In a prospective randomized trial comparing the open repair and endovascular treatment of asymptomatic PDAs, 15 PAAs were treated using the Viabahn stent graft, and a further 15 PAAS were surgically treated. The mean follow-up was 46 months [5,7]. Results revealed no significant differences between the two groups: primary patency at 12 months was 100% for the open repair group and 87% for the endovascular repair group. Furthermore in another paper [5,8], these same authors reported similar midterm results for 27 patients in their open surgery group and 21 in the endovascular treatment group, including no difference in 6-year patency.
Recently, the PARADE study [9] aimed to compare elective surgical repair of Popliteal Artery Aneurysms (PAAs) via a posterior approach vs. endovascular exclusion, analyzing early and five-year outcomes in a multicentre retrospective study. Their findings are very interesting, demonstrating that at 30 days, no differences were found in major morbidity, mortality, graft occlusion, or re-interventions. Three patients (0.7%) in the open group experienced nerve injury. Moreover, at five-year follow-up, freedom from re-intervention was higher in the open group (82.2% vs. 68.4%; p = .021). No differences were observed in secondary patency (open group 90.7% vs. endo group 85.2%; p = .25) or amputation-free survival (open group 99.0% vs. endo group 98.4%; p = .73). The authors concluded that early and long term outcomes following elective repair of PAAs measuring ≤ 60 mm via a posterior approach or endovascular exclusion seem comparable [9]. The sensible reduction in morbidity and mortality of endovascularly repaired PAAs has shifted clinical practice toward an interventional approach.
In this present case series report, most of the patients were older, with several comorbidities. In the decision-making process, the superiority of endovascular technique in avoiding the risk of nerve injury and reducing the length of hospitalization should be considered in selected patients, especially in patients with high cardiac risk.
The advantages of endovascular repair are low invasiveness, minor blood loss; and a short duration of intervention. Further major benefits of this minimally invasive procedure are short hospitalization and short recovery times with fewer wound complications. However, the use of endovascular repair is limited by the patient’s anatomy. For a successful stent-graft implantation, patients with at least two runoff vessels and suitable proximal and distal landing zones (2 cm) are preferred [5,10]. Predictors of failure in endovascular PAA repair have been hypothesized but are not well-established in literature. Many authors have suggested that endovascular repair for popliteal artery aneurysms should be performed on patients with Proximal and distal landing zones greater than 15 mm of healthy artery, and a tibial runoff with more than two vessels. In the present case series all patients had a proper run-off vessel patency, with all infrapopliteal arteries patency during and after the surgery. This supports better outcomes for the endovascular approach in treating popliteal artery aneurysms.
Merit Wrapsody is are flexible self-expanding endoprosthesis indicated for use in hemodialysis patients for the treatment of stenosis or occlusion within the dialysis outflow circuit of an Arteriovenous (AV) fistula or AV graft, consisting of Nitinol, ePTFE, PTFE structure. Several papers showed encouraging results regarding the target lesion primary patency at 30 days of 100% (45 of 45 patients had reached 30 days of follow-up). The target lesion primary patency for the patients who had completed 12 months of follow-up was 84.6% (33 of 39) [5,11]. This case series report has some limitations, since it is a small sample size, with short-term follow-up and no comparator arm, mainly open-surgery patients arm or endovascular surgery arm with other endovascular devices. Larger, randomized, and prospective studies should be performed to evaluate the safety and efficacy of endovascular treatment with Merit Wrapsody for PAA.
Endovascular treatment with Merit Wrapsody® covered stents for PAA seems to be a safe and effective alternative for treating this condition in a minimally invasive manner, leading to adequate exclusion of the aneurysm and preservation of flow in this preliminary analysis. Larger, prospective controlled trials are required to validate these initial findings.
Informed consent has been obtained from the patient for publication of the case report and accompanying images.
- Cecenarro RR, Allende JN, Barreras Molinelli L, et al. Popliteal artery aneurysms: Literature review and presentation of case. Rev Fac Cien Med Univ Nac Cordoba. 2018;75(1):41-45. Available from: https://doi.org/10.31053/1853.0605.v75.n1.16097
- Tielliu IF, Verhoeven EL, Zeebregts CJ, Prins TR, Bos WT, Van den Dungen JJ. Endovascular treatment of popliteal artery aneurysms: is the technique a valid alternative to open surgery? J Cardiovasc Surg (Torino). 2007;48:275-279. Available from: https://pubmed.ncbi.nlm.nih.gov/17505430/
- Saunders JH, Abisi S, Altaf N, Yong Y, MacSweeney ST, Whittaker S, et al. Long-term outcome of endovascular repair of popliteal artery aneurysm present a credible alternative to open surgery. Cardiovasc Intervent Radiol. 2014;37:914–9. Available from: https://doi.org/10.1007/s00270-013-0744-6
- Gilbert J, Rai J, Kingsmore D, Skousen J, Ptohis N. First clinical results of the Merit WRAPSODY™ cell-impermeable endoprosthesis for treatment of access circuit stenosis in haemodialysis patients. Cardiovasc Intervent Radiol. 2021 Dec;44(12):1903–13. Available from: https://doi.org/10.1007/s00270-021-02953-8
- de Athayde Soares R, Cury MVM, Futigami AY. Popliteal artery aneurysm treated with endovascular technique and new device: case report and literature review. JSM Heart Surg Case Images. 2024;4(1):1012. Available from: https://www.jscimedcentral.com/jounal-article-info/JSM-Heart-Surgery-Cases-and-Images/Popliteal-Artery-Aneurysm-Treated-With-Endovascular-Technique-and-New-Device:-Case-Report-and-Literature-Review-11805#
- Galland RB. History of the management of popliteal artery aneurysms. Eur J Vasc Endovasc Surg. 2008;35:466–72. Available from: https://doi.org/10.1016/j.ejvs.2007.11.011
- Antonello M, Frigatti P, Battocchio P, Lepidi S, Cognolato D, Dall’Antonia A, et al. Open repair versus endovascular treatment for asymptomatic popliteal artery aneurysm: results of a prospective randomized study. J Vasc Surg. 2005;42:185–93. Available from: https://doi.org/10.1016/j.jvs.2005.04.049
- Antonello M, Frigatti P, Battocchio P, Lepidi S, Dall’Antonia A, Deriu GP, et al. Endovascular treatment for asymptomatic popliteal artery aneurysm: 8-year concurrent comparison with open repair. J Cardiovasc Surg (Torino). 2007;48:267–74. Available from: https://pubmed.ncbi.nlm.nih.gov/17505429/
- Troisi N, Bertagna G, Saratzis A, Zayed H, Torsello GB, Dorigo W, et al. Elective surgical repair of popliteal artery aneurysms with posterior approach vs. endovascular exclusion: early and long term outcomes of multicentre PARADE study. Eur J Vasc Endovasc Surg. 2025;69:110–7. Available from: https://doi.org/10.1016/j.ejvs.2024.08.011
- Siauw R, Koh EH, Walker SR. Endovascular repair of popliteal artery aneurysms: techniques, current evidence and recent experience. ANZ J Surg. 2006;76:505–11. Available from: https://doi.org/10.1111/j.1445-2197.2006.03745.x
- Gilbert J. Prospective first-in-human study of the Merit WRAPSODY endovascular stent graft for treatment of access circuit outflow stenosis in hemodialysis patients. J Vasc Surg. 2022;75(4S):7S. Available from: https://doi.org/10.1016/j.jvs.2022.01.038