Table of Contents
Chronic Ethanol Decreases the Left Ventricular Cardiac Performance
Published on: 15th April, 2024
Introduction: Spaced fiber bundles, less evident cell striations, deposition of collagen fiber bundles, and increased presence of fibroblasts in the cardiac tissue of rats that voluntarily and chronically ingested ethanol were observed by our research group. In addition, we observed increased proliferation and cell death of cardiomyocytes. To find out whether these changes lead to impaired heart functionality, some clinical tests were performed. Aim: to investigate whether chronic ethanol decreases the left ventricular performance assessed by exercise testing, electrocardiogram, and echocardiogram of male and female UChB strain rats. Material and methods: ten adult males and ten adult females, Wistar strain rats, named UChB (University of Chile), spontaneous high ethanol drinkers (consumption greater than 2 g ethanol / Kg body weight/day), and ten male UChB rats and ten adults female UChB rats, not exposed to ethanol, UChBC rats (controls) were used. Cardiac performance was evaluated by the stress test, electrocardiogram, and echocardiogram. Results: Exposed females showed ventricular morphological changes in the heart. The exposed females and males had the highest heart relative weight with females being larger than males. The exposed females showed altered electrocardiogram and echocardiogram. Conclusion: Chronic ethanol decreases the left ventricular cardiac performance in rats. Females are more sensitive to changes in cardiac electrical conduction.
A Complex Case with a Completely Percutaneous Solution: Treatment of a Severe Calcific Left Main in a Patient with Low-Flow Low-Gradient Aortic Stenosis
Published on: 2nd April, 2024
Background: This case study explores an integrated approach to managing a complex cardiac condition, presenting a comprehensive single-session intervention. This includes balloon valvuloplasty using a Nucleus 18 mm balloon, complex angioplasty with rotational atherectomy (rotablator) targeting calcified lesions in the left main and left anterior descending artery, and Transcatheter Aortic Valve Implantation (TAVI) with a 23 mm Sapien 3 valve, all performed on an 81-year-old woman. Furthermore, this report underscores the strategic left atrial appendage closure conducted three months post-procedure due to the patient’s elevated hemorrhagic risk.Case presentation: Facing critical coronary and valvular pathologies, the patient underwent a meticulously planned, single-session intervention. The process began with a balloon valvuloplasty using a Nucleus 18 mm balloon to address the aortic stenosis. This was followed by a high-risk angioplasty, during which the Impella CP device provided hemodynamic support and rotational atherectomy was employed to address the calcified coronary artery disease effectively. The same session saw the successful execution of TAVI using a 23 mm Sapien 3 valve. The comprehensive approach notably diminished procedural complications, illustrating the benefits of an integrated treatment pathway in managing high-risk patients. Three months later, the patient underwent a left atrial appendage closure, a critical move considering her high risk of hemorrhage. This procedure also provided an opportunity to assess the favorable outcomes of the previous angioplasty.Conclusion: This case validates the feasibility and efficacy of performing multiple advanced percutaneous interventions in a single session for high-risk cardiac patients. It underscores the crucial role of innovative and personalized treatment strategies in improving patient outcomes, particularly in complex clinical scenarios. Moreover, the case exemplifies the essential relationship between immediate, comprehensive intervention and subsequent follow-up procedures in ensuring optimal long-term patient care.
Diagnosing Peripartum Cardiomyopathy in a Resource-Limited Setting, a Clinical Perspective: Case Report
Published on: 29th March, 2024
Peripartum cardiomyopathy is a rare case of heart failure with reduced ejection fraction and is considered a diagnosis of exclusion. The symptoms of heart failure in patients with peripartum cardiomyopathy can mimic the physiologic conditions of normal pregnancy. In an acute decompensated state, PPCM can present with acute severe upper abdominal or epigastric pain. We are presenting a 24-year-old female with no personal or family history of heart disease and no identifiable risk factor for PPCM. Based on her initial presentation in the emergency department, a diagnosis of acute severe pancreatitis was sought, and she was referred to the Intensive Care Unit. After further evaluation of the serological tests and imaging, she was eventually diagnosed as a case of PPCM. We emphasize the rare nature of the disease with a diverse presentation which poses a diagnostic challenge, especially in a resource-limited setting where advanced diagnostic tools may be restricted and socioeconomic condition poses a barrier to further patient evaluation. This case exemplifies the infrequent occurrence and atypical manifestation, presenting a learning opportunity for future clinicians.
The Ketogenic Diet: The Ke(y) - to Success? A Review of Weight Loss, Lipids, and Cardiovascular Risk
Published on: 6th March, 2024
Background: Obesity remains a global epidemic with over 2.8 million people dying due to complications of being overweight or obese every year. The low-carbohydrate and high-fat ketogenic diet has a rising popularity for its rapid weight loss potential. However, most studies have a maximal 2-year follow-up, and therefore long-term adverse events remain unclear including the risk of Atherosclerotic Cardiovascular Disease (ASCVD).Results: Based on current evidence on PubMed and Google Scholar, there is no strong indication ketogenic diet is advantageous for weight loss, lipid profile, and mortality. When comparing a hypocaloric ketogenic diet with a low-fat diet, there may be faster weight loss until 6 months, however, this then appears equivalent. Ketogenic diets have shown inconsistent Low-Density Lipoprotein (LDL) changes; perhaps from different saturated fat intake, dietary adherence, and genetics. Case reports have shown a 2-4-fold elevation in LDL in Familial hypercholesterolaemic patients which has mostly reversed upon dietary discontinuation. There is also concern about possible increased ASCVD and mortality: low (< 40%) carbohydrate intake has been associated with increased mortality, high LDL from saturated fats, high animal product consumption can increase trimethylamine N-oxide, and cardioprotective foods are likely minimally ingested.Conclusion: Ketogenic diets have been associated with short-term positive effects including larger weight reductions. However, by 2 years there appears no significant differences for most cardiometabolic risk markers. Therefore, this raises the question, excluding those who have a critical need to lose weight fast, is this diet worth the potentially higher risks of ASCVD and mortality while further long-term studies are awaited?
Rida Herbal Bitters Improve Cardiovascular Function in High-fat Diet/Streptozotocin-induced Diabetic Rats
Published on: 28th February, 2024
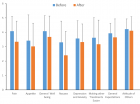
Background: Effective medication to manage diabetes mellitus-related organ complications with minimal adverse drug toxicity is still in pursuit by scientists worldwide. This study investigated the cardio-protective of Rida herbal bitter (RHB) in a high-fat diet/streptozotocin (STZ)-induced diabetic rats.Methods: Thirty-two matured male Wistar rats (250 ± 20g) were used. The animals were fed with high-fat diet (HFD) for 6 weeks before diabetes induction. A single dose of (35 mg/kgb.wt) freshly prepared STZ was injected intraperitoneally to induce diabetes. The animals were allocated into four groups, 8rats/group. Group I: control; Group II: HFD/STZ-induced diabetic rats; Groups III & IV: HFD/STZ-induced diabetic rats treated with 0.3 ml RHB & 200 mg/kgb.wt metformin respectively. At the end of the experiment, the animals were sacrificed, blood was sample collected via cardiac puncture and the heart was excised and homogenized. The blood samples and cardiac homogenates tissue were centrifuged to retrieve clear supernatant plasma for biochemical assay.Results: Diabetic rats exhibited significant (p < 0.05) elevated blood glucose, insulin, glycated hemoglobin (HbA1c), cardiac biomarkers, lipid profile, malondialdehyde (MDA), pro-inflammatory cytokines, food, and water intake levels with a reduction in body weight, cardiac antioxidant activity, and total protein. RHB administration significantly (p < 0.05) diminished the blood glucose, insulin, HbA1c, cardiac biomarkers, MDA, pro-inflammatory cytokines, lipid profile, food, and water intake, and improved the body weight cardiac antioxidant activity, and total protein.Conclusion: Rida herbal bitter possesses a cardio-protective effect from this study and could be a better alternative medication for managing diabetes and its related cardiovascular complications.
Calcium Scoring on CT Coronary Angiography in Hypertensive Patients as a Criterion for the Prediction of Coronary Artery Disease
Published on: 19th February, 2024
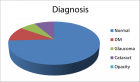
Introduction: Hypertension is the strongest independent predictor of Coronary Artery Disease (CAD) identified by Computed tomography of coronary arteries (CTCA). In this study, CTCA-assessed Coronary Calcium Scoring (CCS) was studied in hypertensive subjects referred for CTCA.Methods: After excluding TAVI and graft assessment patients, the individual electronic health records of 410 consecutive patients who underwent CTCA between July and November 2020, were reviewed with a mean age of 58.7 years. Risk factors were recorded including smoking (38%), hyperlipidaemia (33%), positive family history (22%), systemic hypertension (48%), diabetes mellitus (30%), and male gender (46%). Referral criteria, ethnicity, cardiac, and past medical history were recorded. Patients were stratified into four groups according to CAD severity: absent, mild, moderate, and severe disease, as seen on CTCA. The mean CCS for each CAD category was compared between hypertensive and non-hypertensive patients. Mean CCS were further compared according to the number of coronary arteries affected and the severity of CAD in each artery. Results: Out of all CTCA reports, 200 (48.8%) CCS were interpreted in the very low-risk category, 80 (19.5%) low risk, 58 (14.1%) moderate risk, 23 (5.6%) moderately high risk and 49 (12.0%) high risk. A significant difference in mean CCS and CAD severity was observed between mild, moderate, and severe CAD (p = 0.015 and p < 0.001). Comparison of CCS between hypertensives and non-hypertensives, across the four CAD severity categories, revealed a significant difference in mean CCS in the severe CAD category (p = 0.03). There was no significant difference in the CCS between hypertensives with chest pain and hypertensives without chest pain. A higher number of affected coronary arteries was associated with a higher mean CCS and a significant difference in CCS was observed between hypertensive and non-hypertensive subjects for the number of arteries affected. Similar results were observed when comparing mean CCS in moderate-severely affected coronary arteries.Conclusion: Hypertensive patients with a high CCS were associated with a higher incidence of severe CAD independent of the presence of chest pain. These results suggest that the incorporation of CCS in the investigation of CAD on CT angiography may pose a powerful adjunct in proposing an alternative paradigm for the assessment of patients with hypertension, in the progress of coronary artery disease.
Impact of Chronic Kidney Disease on Major Adverse Cardiac Events in Patients with Acute Myocardial Infarction: A Retrospective Cohort Study
Published on: 5th February, 2024
Background: Acute Myocardial Infarction (AMI) results in a reduction in patients’ life expectancy. Different risk factors affect the risk of Major Adverse Cardiac Events (MACE). Although the role of kidney dysfunction in patients with Chronic Kidney Disease (CKD) in cardiac events has been identified, many patients with AMI are unaware of their underlying kidney disease. This study aimed to compare the incidence of adverse cardiovascular events and identify predictors of major adverse cardiovascular events in the medium term among patients with and without renal dysfunction following AMI. Methods: This retrospective cohort study was conducted on 1039 patients who were hospitalized for Acute Myocardial Infarction (AMI) between 2018 and 2019. The patient cohort comprised 314 women (mean age: 69.8 ± 13.2 years) and 725 men (mean age: 60.5 ± 13.8 years). Patient data were obtained from the registry of patients with acute myocardial infarction and the participants were followed up for a minimum of one year following hospital discharge to assess the incidence of MACE.Results: The study found that patients with a Glomerular Filtration Rate (GFR) level below 60 had a significantly higher mortality rate than those with a GFR level of 60 or above (15.7% vs. 3.5%,p < 0.0001). The multivariate analysis showed that Diabetes Mellitus (DM), GFR, and Non-ST Elevation Myocardial Infarction (NSTEMI) are significant risk factors for cardiovascular events. (p = 0.016, p = 0.015, p = 0.006 respectively), while variables such as sex, age, and Hypertension (HTN) were not significant risk factors. There was a negative correlation between GFR and death (0.241 - = r, p < 0.0001)Conclusion: This study highlights the importance of detecting kidney disease during an AMI and managing risk factors for cardiovascular disease to improve health outcomes and reduce the risk of mortality.
Persistent Bilateral Vocal Cord Paralysis Following Unilateral Basal Ganglia Hemorrhage
Published on: 18th January, 2024
Post-stroke vocal cord paralysis is a condition much less recognized compared to dysphagia. We describe bilateral vocal cord palsy in a thirty-six-year-old man following a stroke.
The Effect of SGLT-2i and GLP-1RA on Major Cardiovascular Conditions: A Meta-Analysis
Published on: 18th January, 2024
Purpose: Sodium-glucose co-transporter 2 inhibitors (SGLT-2i) and Glucagon-like Peptide-1 Receptor Agonists (GLP-1RA) are two common anti-hyperglycemic agents prescribed by clinicians. The effects on cardiovascular conditions such as Heart Failure (HF) hospitalization, stroke, Myocardial Infarctions (MI), and other cardiovascular conditions are not well studied. The purpose of this study is to analyze existing data on the effect of SGLT-2i and GLP-1RA on preventing these cardiovascular conditions. Methods: A retrospective meta-analysis of all existing literature on the effect of SGLT-2i and GLP-1RA on the rates of the following categories were researched: primary cardiovascular outcomes, HF hospitalizations, Atrial Fibrillation (AF), stroke, MI, and HF symptoms. Hazard ratios for each category were obtained, and the overall Hazard Ratio (HR) to determine overall statistical significance was computed. Result: Both medication classes provided a statistically significant reduction in preventing major cardiovascular events. Only SGLT-2i provided a statistically significant reduction in heart failure hospitalizations. Only GLP-1RA provided a statistically significant reduction in preventing stroke. Neither medication class provided a statistically significant benefit in preventing myocardial infarctions. More studies are needed on the effects of either SGLT-2i or GLP-1RA agonists on preventing HF symptoms or AF. Conclusion: This study demonstrates that SGLT-2i and GLP-1RA are important for improving both diabetic and cardiovascular health. In patients at risk for a major cardiovascular event, SGLT-2i or GLP-1RA may be prescribed by clinicians. More studies must be performed to draw more conclusions.
Aspirin for Primary Prevention of Cardiovascular Disease: What We Now Know
Published on: 9th January, 2024
Cardiovascular disease (CVD), including coronary artery disease and stroke, is the leading cause of death worldwide. Advances in primary and secondary prevention of CVD have improved patient prognoses and outcomes, however, it is imperative that the clinician and patient engage in early risk factor screening and preventive management of modifiable risk factors for CVD. In addition to blood lipid and blood pressure lowering medications, aspirin has been a long-standing therapy targeted to the prevention of CVD based on its antiplatelet and anti-inflammatory activity. However, recent articles and reports on updates to clinical guidelines for the primary prevention of CVD have resulted in confusion about aspirin recommendations. This review aims to assess the latest guidance on aspirin in CVD prevention and how to identify appropriately at-risk patients who may benefit from low-dose aspirin therapy as part of their CVD preventive healthcare choices. Additionally, this review will provide practical application guidance about clinician-patient conversations to clearly explain the benefits and risks of aspirin use and ensure a patient-centric decision to initiate aspirin therapy.
The Fulcrum of the Human Heart (Cardiac fulcrum)
Published on: 3rd January, 2024
Introduction: The functional anatomy of the myocardium allows envisioning that it initiates and ends at the origin of the great vessels. In our research, we have always considered that it should have a point of attachment to allow its helical rotation to fulfill the fundamental movements of shortening-torsion (systole) and lengthening-detorsion (suction), which once found, was called the cardiac fulcrum. Materials and methods: A total of 31 hearts, arising from the morgue and slaughterhouse were used: 17 corresponded to bovids and 14 were human. Anatomical and histological studies were performed. The heart was fixed in 10% buffered formalin. Hematoxylin-eosin, Masson’s trichrome staining technique, and 4-micron sections were used for the histological study, and 10 % formalin was used as a buffer. Results: The anatomical investigations have revealed that all the hearts (bovids and humans) have myocardial support whose histological structure in the analyzed specimens presents with an osseous or chondroid-tendinous character. In this structure, which we have called the cardiac fulcrum, are inserted the myocardial fibers at the origin and end of the band, which correspond to the continuous myocardium coiled as a helix.Conclusion: This description of the fulcrum would end the problem of lack of support of the myocardium to fulfill its function of suction/ejection.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."